In the mid-1940s, as part of a series of expeditions to remote Canadian Artic regions, refractive errors of native Inuit populations were measured. Initial levels of myopia were encouragingly low, less than 2%. Early hypotheses alluded to a genetic advantage. Yet shortly afterwards, amongst parts of the community, myopia had risen ten-fold in little over a decade. Such change, over a short period, meant genetics were an unlikely cause, but isolating a single environmental factor would prove challenging. Lifestyles had transformed dramatically. Shifts away from a predominantly outdoors lifestyle, an increased consumption of refined sugars and carbohydrates, and the introduction of mandatory schooling were all potential suspects.1 The whole episode illustrates the potency of environmental influences on our health.
More recently, global events created natural experimental conditions for myopia to be studied. Extended lockdown periods, mandated during the COVID-19 pandemic, led to reports of an increase in myopia; with early data suggesting younger children may have been particularly susceptible to environmental changes.2
Outside of such extremities, everyone’s lifestyle remains subject to a subtle but inevitable evolution: modern-day routines seldom match those of generations past. So, which aspect of our current lifestyles warrants change? And is it too late to correct our myopia-inducing ways? This article explores the evidence for commonly considered environmental factors, the underlying theories, and highlights the gaps in our knowledge.
Near work, screen work
The UK has the second highest level of screen use amongst children: 44 hours per week. For example, UK children spend longer looking at a screen than the average full-time working adult spends at work.3, 4 Yet, problems extend far beyond the UK. Globally, screen-related health concerns have prompted action from governments. In Taiwan, for example, parents can be issued fines if their child uses electronic devices for extended periods.4 Whilst in China, children are prohibited from online gaming on weekdays and limited to just 1 hour during weekends and holidays.6
Speculation linking screen work to negative health outcomes, such as obesity, poorer sleep, and reduced cognitive abilities has been corroborated by research7, 8 but the influence of screens on myopia remains unclear. Academics stress epidemiological data show an upwards trajectory of myopia which predates the introduction of many handheld digital devices,9 raising the question of whether it is near work, screen work, both, or neither which increases risk of myopia?
The underlying theories:
Determining the specifics of how near work impacts myopia has proven elusive. Outlined below are several interrelated theories, each aiming to explain the connection. Affiliated mechanisms, also considered part of the process, relate to accommodation-convergence ratios; pupil function; near phoria; and spatial frequency.10
- Accommodative lag
Larger accommodative lags are observed in myopes compared to emmetropes leading to speculation that lag acts as a precursor to myopia. In actuality, several longitudinal studies have failed to verify such claims; suggesting lag may be correlative with, but not the cause of, myopia.11, 12
- Peripheral hyperopia
A longstanding hypothesis suggests peripheral retinal hyperopic defocus, relative to the fovea, provides a signal for ocular growth13 and although myopia management therapies based on this premise have yielded positive outcomes, the validity of the peripheral hyperopia theory has been contested.14,15
- Ciliary body
Differences in both ciliary muscle size and thickness have been observed in myopes compared to emmetropes. Changes to muscle morphology could, potentially, affect accommodative function and ultimately compromise the eyes’ biomechanical properties and shape,15 but these changes in myopic eyes are often regarded a consequence rather than a cause of myopia.10
- Contrast polarity
White text on a black background is reported to induce choroidal thickening and overstimulate retinal ON channel pathways, with the converse true of black text on white backgrounds.16 A recent study reports regional differences in sensitivity to text contrast polarity between emmetropes and myopes, with distinct responses noted from the perifoveal region.17
What the research tells us:
Evidence linking screen work to myopia is mixed;18, 19 often hampered by a failure to treat screen use separately from other forms of near work. Data can be compromised further if screen exposure estimates rely upon subjective (eg questionnaires, interviews) rather than objective methods.
Foreman et al (2021) attempted to dissect the issue of screen work and myopia through a detailed meta-analysis and review. Risk of myopia for children was found to increase significantly with smart device usage (defined as smartphones and tablets). Risk increased further when smart devices were used in conjunction with computers, but when smart device use was considered alongside other non-screen based near-vision tasks then 54% of the studies failed to find an association between duration of near work and myopia. Nevertheless, the authors highlight specific studies where each additional hour of near work (digital device uses, reading books etc) has been shown to increase the odds of myopia by 1%.
The use of subjective screen time estimates and presence of uncontrolled variables led Foreman et al (2012) to ultimately deem the literature on smart device exposure and myopia to be insufficient and conflicting.18
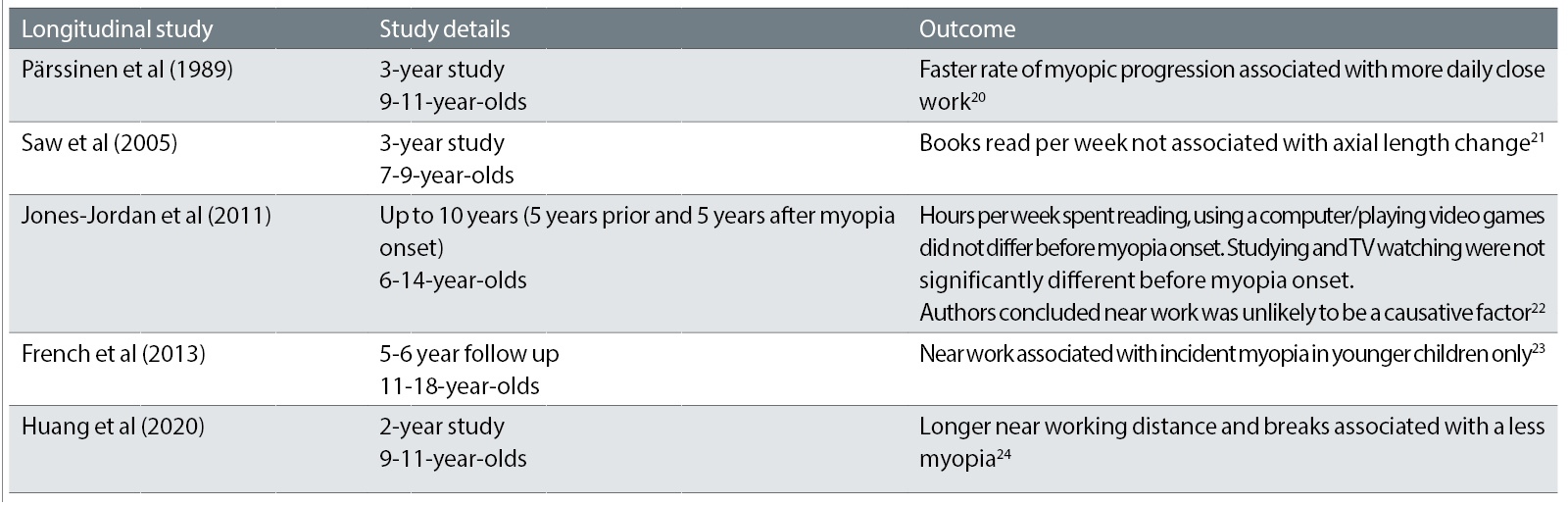
Longitudinal studies of myopia and near work/screen work report conflicting outcomes (see Table 1) but a recent literature synthesis suggests a precipitating role of near work may be related to its nature rather than overall duration. Specifically, working distances closer than 30 cm and continuous near work exceeding 30 mins were linked to increased risk of myopia.15
Table 1: Near work and myopia outcomes from longitudinal studies in children (adapted from Gajjar and Ostrin 2021).15 Note that outdoor time did appear to influence outcomes in at least some of the studies
Television
Contrary to expectations, many studies do not find longer TV viewing times to be associated with increased myopia25-28 although there are notable exceptions.29-31 Any disparities amongst findings are, at least partly, explained by differences in viewing distances.15 For situations necessitating screen use, i.e., in the case of lockdown home-schooling, a television or projector is shown to induce less of a myopic shift compared to a mobile phone or tablet.32
Future directions:
Advances in the usability, validity, and access to objective methods of measuring near working distances, specifically those which allow continuous measurement, will galvanise future research efforts into myopia and near work.
Novel applications of existing technologies have shown potential to characterise indoor scenes via construction of dioptric maps, thus offering more comprehensive approaches to studying indoor environments.33
For now, practitioners have been advised to promote a healthy balance of time outdoors and near work is used everywhere.34
Education
The underlying theories:
Mechanisms believed to underlie a relationship between myopia and education overlap with those outlined for near/screen work. Contributory factors may be compounded by genetic predispositions, and/or relate to other environmental influences such as time indoors.9
What the research tells us:
Studies in different population groups (both different ethnicities and geographical locations) have linked myopia to aspects of education. Several overarching conclusions may be drawn: (i) myopia prevalence is lower in places where children do not attend school (ii) amongst adults, those who pursued higher education or completed more years of schooling have a tendency to be more myopic (iii) and countries with an epidemic of myopia are also often those associated with early educational pressures.9
A causal relationship between myopia and education has also been identified.35 Mountjoy et al (2018) assessed both the influence of genetic predisposition to myopia on years of education and, conversely, influence of genetic predisposition to years of education on myopia. Each additional year of education was associated with an increase of -0.27D. Put another way, a UK university graduate, with around 17 years of education, could be at least -1D more myopic than someone who left school at the age of 16.35
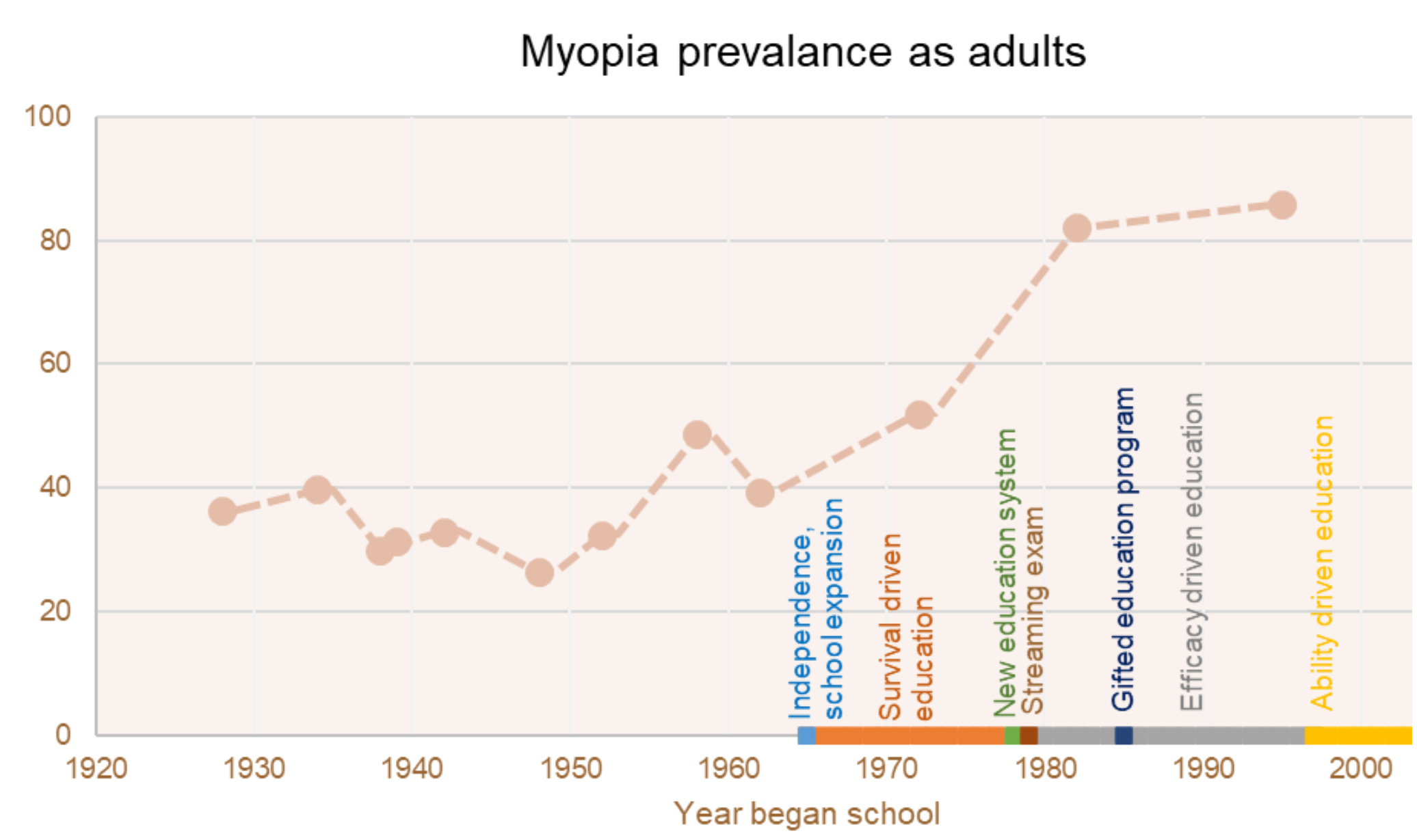
Aside from years spent studying, patterns of educational delivery are suspected to exacerbate myopia development. For example, a study of Singaporean adults showed a rise in myopia amongst those who began school around the 1980s (see figure 1), this coincides with introduction of major educational reforms at the time including more intensive, accelerated schooling.36
Figure 1: Percentage prevalence of myopia amongst Singaporean adults and year schooling began (based on Sensaki et al 2017)36. Following Singaporean independence, a redesign of education systems led to three main phases. Survival-driven education (1965-1978): expansion of education system, focused on enabling all children to have access to schooling. Efficacy-driven education (1978-1997): aimed to minimise performance variation, universal high standards. Ability-driven education (1997-ongoing): designed to increase choice and quality in the educational system36, 37
Future directions:
Countries with high myopia tend to have educational systems which integrate extensive engagement with after-school tutorials and other more concentrated forms of learning.38 Yet international educational outcome rankings show countries both with – and without high myopia levels lie within the highest performing quartile.38, 39 It is thereby implied that minimising additional educational load could offer protection against myopia without compromising on educational outcomes.
As our understanding of the causative factors continues to build, both educational surroundings and patterns of educational delivery will likely evolve to offer safeguards against myopia.
Time outdoors
Amongst its reputed benefits, time spent outdoors improves mental wellbeing, facilitates cognitive development, and reduces obesity.40-42 Relevant to myopia is the prospect that time outdoors offers a seemingly cheap and effective way to delay myopia onset.
The underlying theories:
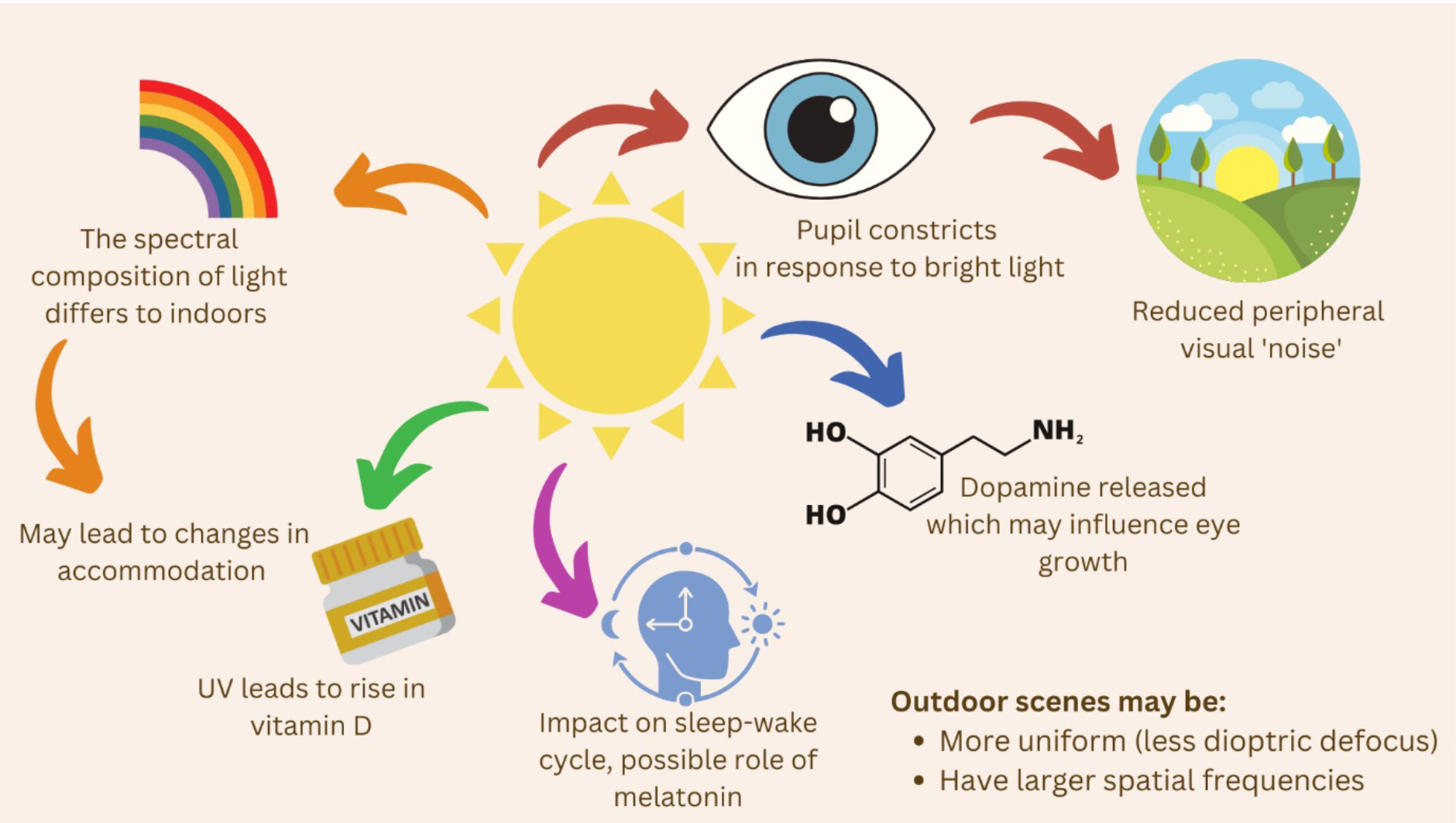
Theories of how time outdoors counteracts myopia are wide-ranging and far from definitive. Outdoor environments are, of course, unlike the indoors. Light is brighter and vistas may be more dioptrically uniform with greater spatial frequencies, all of which will alter the visual experience and associated ocular response (eg, pupil size, accommodative effort required).
Mechanisms proposed to underlie the protective effects of time outdoors against myopia are summarised in figure 2. Theories may be broadly classed as those relating to properties of light (brightness, spectral composition), relating to the visual scene (dioptric defocus, uniformity), and those which are associated with systemic or retinal release of neuromodulators and other chemicals.43
Figure 2: Current and past proposals to explain the underlying influencing factors of time outdoors on myopia9,43-45
What the research tells us:
Causality between time outdoors and myopia has been confirmed through school-based randomised control trials (RCTs). RCTs, along with observational studies, show evidence is stronger for time outdoors inhibiting myopia onset rather than slowing down its progression.46 Based on clinical trials outcomes, spending time outdoors reduces the relative risk of incident myopia by 24-39%.46
Where a slowing of myopia progression is reported, typical annual values range from ~0.13 to 0.17D for SER and by ~-0.03 to -0.08mm for axial length, but these amounts fall short of the desired minimum change needed to demonstrate clinical significance (i.e., an annual difference of 0.25D in refractive error or a slowing of axial elongation by 0.11mm).46, 47
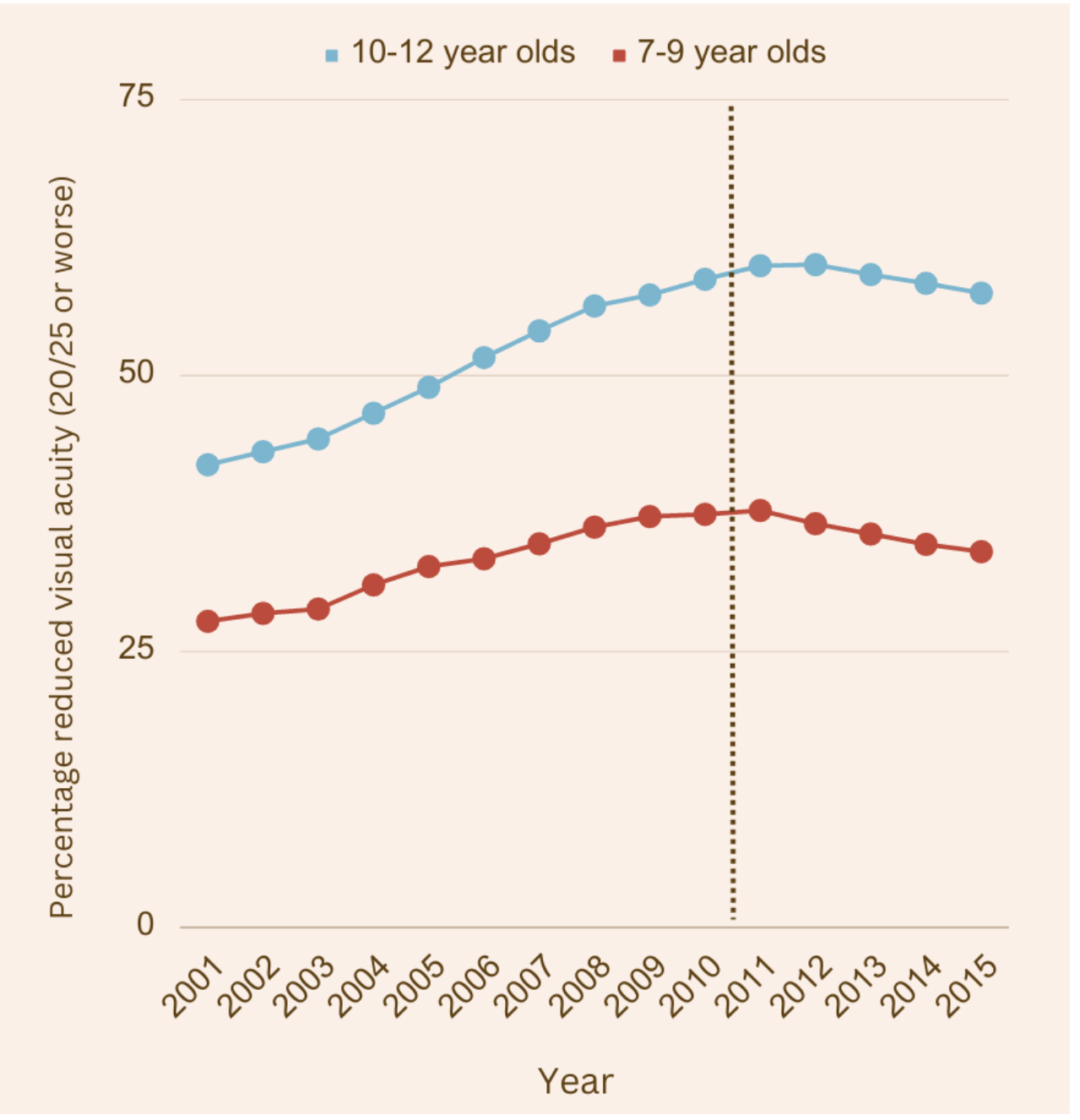
Elsewhere, reports suggest spending time outdoors can offset the myopia risk introduced by having myopic parents or undertaking near work.9 Promising findings are also reported following an initiative in Taiwan where the introduction of a mandatory 120 minute daily outdoor exposure is credited for an apparent reversal of the myopia trend (see figure 3).48
Although evidence is exceedingly in favour of spending time outdoors, our knowledge remains incomplete. For instance, a study published in 2019 reported on a potential myopia rebound effect within the three years following a one-year outdoor jogging programme.49 The study, while limited in several respects, reiterates the importance of post-interventional follow up.49
Questions also remain over the dose-response relationship concerning brightness and duration of outdoor exposure.46 A clinical trial reported lower intensity light (e.g., under the shade) could still inhibit myopia if exposure durations were sufficiently long (≥200mins). Higher intensity light (i.e., stronger sunlight) was shown to be effective in non-myopes even when exposure durations were short (125-199 mins).50 There are even suggestions that elevating indoor school lighting levels could help thwart myopia onset.51
Figure 3: Prevalence of reduced visual acuity in primary school children in Taiwan from 2001-2015. Dashed line denotes beginning of outdoor activities initiatives to prevent myopia (after Wu et al 2020)48
Future directions:
A desire to counter myopia by replicating outdoor environments within the classroom has inspired innovative proposals, these include wallpapering classrooms to reflect the spectra of outdoor spatial frequencies and trials evaluating efficacy of light-filled glass classrooms.52, 53
Advances in tools which objectively measure outdoor time can also facilitate future research efforts.54-56 In a sign of times to come, a newly released feature on Apple Inc devices allows both daylight exposure and screen viewing distances to be measured. The companies’ promotional material makes specific reference to myopia, signifying a rising awareness of the issue.57
On an immediate practical level, the College of Optometrists’ myopia management guidance suggests encouraging a healthy balance of near work and time spent outdoors. More specific advice from the International Myopia Institute recommends schoolchildren spend more time outdoors of at least 80-120 minutes a day.58
Physical activity
The underlying theories:
Physical exercise reportedly mitigates risk of all major causes of blindness (glaucoma, diabetic retinopathy, macula degeneration, and cataracts).59-61 How pathogenic mechanisms might be disrupted is yet to be established, but current speculations include improvements in vascular endothelial function, reduced inflammation and oxidative stress.
Of relevance to myopia is that scleral hypoxia has been implicated in the ocular growth process. Since exercise can boost choroidal blood flow, and thereby available oxygen, exercise could theoretically safeguard against scleral hypoxia and, by extension, against myopia.62-64 Other proposed pathways involve an exercise induced change in growth hormones or changes to insulin resistance.65
What the research tells us:
Study outcomes are equivocal.66-69 Where the literature does find consensus is that evidence for physical activity as an independent risk factor for myopia remains insufficient. Difficulties in isolating the impact of physical activity are partly due the confounding influence of time outdoors, as both often take place simultaneously.
It is also feasible that rather than physical activity inhibiting myopia, the reverse is true ie, myopia inhibits enthusiasm for physical activity.
Future directions:
Further data are needed to disentangle the influence of physical activity from merely spending time outdoors; indoor activity from outdoor; and a better characterisation of how day-to-day and seasonal physical activity patterns vary.67
Other environmental factors
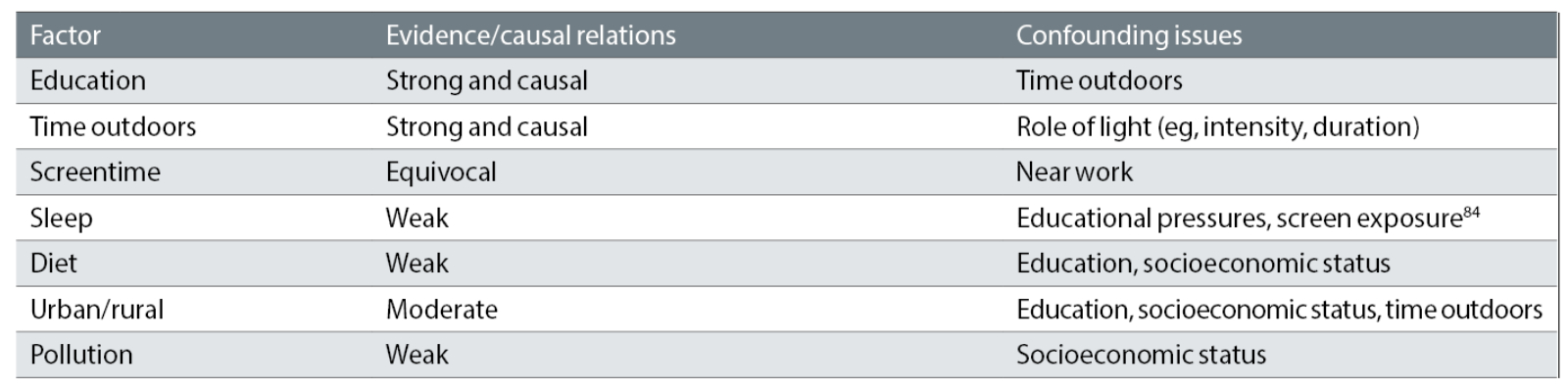
Urbanisation, smoking, pollution, and even posture have all been considered possible culprits in the search to identify myopiogenic risks. Few lines of enquiry have produced strong evidence, and most are confounded by other variables (see table 2). Two emerging areas of interest are described below.
Table 2: Examples of potential environmental risk factors for myopia, strength of evidence, and associated confounding issues (adapted from Morgan et al 2021)9
Sleep
Poorer sleep outcomes in children are attributed to reduced physical activity, increased screen time,70 and educational load.71 Appropriately timed light exposure can, via mediation of the hormone melatonin, synchronise the body’s circadian clock to daily light/dark cycles; leading to better sleep. The circadian clock and melatonin also contribute to the regulation of dopamine release.72 Hence, substantial overlap exists between environmental factors known to influence sleep and those believed to impact myopia.
Despite inferences of a possible connection, a recently published review deemed current evidence linking myopia to sleep as insufficient. The authors did, however, find associations with less sleep in seven out of 15 studies reviewed; poor sleep quality in three out of four studies; and late bedtimes in three out of six studies.45 Variability in the sleep-wake cycles of myopic children were also noted, implying there may be factors interlinking sleep, light exposure, and myopia.
Diet
The dominant hypothesis linking myopia to nutrition is rooted in findings from animal studies showing insulin can interfere with eye growth.73,74 Related are suggestions that poor glycaemic control in humans, possibly induced through consumption of refined carbohydrates, may also play a contributory role.
While studies have shown genetic associations between high-grade myopia and insulin-like factors, data are limited and conflicting.9, 75-77 A recently published study has, however, used Mendelian randomisation to provide compelling evidence of a causal relationship between myopia and glycaemic traits.78 Specifically, lower adiponectin (a protein secreted by adipocytes and involved in insulin resistance),79 and to a lesser extent elevated HbA1c (an indicator of blood glucose) were both linked to an increased risk of myopia.
Further support is provided by several dietary studies. A large national dataset from the US showed raised insulin levels to increase the odds of myopia.80 In France, consumption of refined carbohydrates was reported to significantly increase probability of myopia in girls but decreased it for boys, the difference explained by potential disparities in physical activity between boys and girls.81 And encouraging outcomes from China show wholegrain consumption to be inversely correlated with myopia.82
Other theories of diet and myopia consider the role of vitamin D; lower levels are reported in myopes compared to emmetropes, but this may simply be a consequence of spending less time outdoors. Various trace elements have also been associated with myopia, but current data are limited.44
Despite the growing evidence base, the most recent systematic review on the topic has concluded that while an effect of diet on myopia is implied, further research is necessary to understand the specific nutrients and dietary aspects involved.44
Conclusion
Our modern-day lifestyles come with many strings attached; increased risk of obesity, cancers, cardiovascular disease, and now it appears myopia can be added to this unfortunate list.83
Of the suspected environmental influences, few are supported by strong evidence; exceptions include education and outdoor time (see Table 2, above). Yet most lines of enquiry, particularly those where links to myopia may be unproven, simply refer to factors conducive to good general health: eat well, sleep well, move more.
Whether by acting as an independent risk factor or in synergy with genetic predispositions, our environment has been attributed for the rise in myopia prevalence. The obvious good news is that both our surroundings and behaviour are modifiable.
- Dr Manbir Nagra is an optometrist with a background in academia. She currently undertakes consultancy work within the optical sector.
- Dr Natalia Vlasak is Global Head of Medical and Scientific Affairs at Hoya Vision Care.
References
- Rozema JJ, Boulet C, Cohen Y, Stell WK, Iribarren L, van Rens GHMB, et al. Reappraisal of the historical myopia epidemic in native Arctic communities. Ophthalmic Physiol Opt. 2021 Nov;41(6):1332–45.
- Wang J, Li Y, Musch DC, Wei N, Qi X, Ding G, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. 2021 Mar 1;139(3):293–300.
- British children spend almost two days a week staring at screens, the second highest of all countries surveyed in first-ever global Child Online Safety Index [Internet]. [cited 2023 Jul 31]. Available from: https://www.dqinstitute.org/2021/12/10/british-children-spend-almost-two-days-a-week-staring-at-screens-the-second-highest-of-all-countries-surveyed-in-first-ever-global-child-online-safety-index/
- Average weekly hours of work for full-time workers in the UK 1992-2023 [Internet]. Statista. [cited 2023 Jul 31]. Available from: https://www.statista.com/statistics/280763/average-working-hours-uk/
- The protection of children and youths welfare and rights act - article content - laws & regulations database of the republic of China (Taiwan) [Internet]. [cited 2023 Jul 31]. Available from: https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=D0050001
- Buckley C. China tightens limits for young online gamers and bans school night play. The New York times [Internet]. 2021 Aug 30 [cited 2023 Jul 31]; Available from: https://www.nytimes.com/2021/08/30/business/media/china-online-games.html
- Kininmonth AR, Smith AD, Llewellyn CH, Dye L, Lawton CL, Fildes A. The relationship between the home environment and child adiposity: a systematic review. Int J Behav Nutr Phys Act [Internet]. 2021 Dec;18(1). Available from: http://dx.doi.org/10.1186/s12966-020-01073-9
- Wolf C, Wolf S, Weiss M, Nino G. Children’s environmental health in the digital era: Understanding early screen exposure as a preventable risk factor for obesity and sleep disorders. Children (Basel). 2018 Feb 23;5(2):31.
- Morgan IG, Wu P-C, Ostrin LA, Tideman JWL, Yam JC, Lan W, et al. IMI risk factors for myopia. Invest Ophthalmol Vis Sci. 2021 Apr 28;62(5):3.
- Logan NS, Radhakrishnan H, Cruickshank FE, Allen PM, Bandela PK, Davies LN, et al. IMI accommodation and binocular vision in myopia development and progression. Invest Ophthalmol Vis Sci. 2021 Apr 28;62(5):4.
- Mutti DO, Mitchell GL, Hayes JR, Jones LA, Moeschberger ML, Cotter SA, et al. Accommodative lag before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2006 Mar;47(3):837–46.
- Weizhong L, Zhikuan Y, Wen L, Xiang C, Jian G. A longitudinal study on the relationship between myopia development and near accommodation lag in myopic children. Ophthalmic Physiol Opt. 2008 Jan;28(1):57–61.
- Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia. Neuron. 2012 Apr;74(1):207.
- Atchison DA, Li S-M, Li H, Li S-Y, Liu L-R, Kang M-T, et al. Relative peripheral hyperopia does not predict development and progression of myopia in children. Invest Ophthalmol Vis Sci. 2015 Sep 1;56(10):6162–70.
- Gajjar S, Ostrin LA. A systematic review of near work and myopia: measurement, relationships, mechanisms and clinical corollaries. Acta Ophthalmol. 2022 Jun;100(4):376–87.
- Aleman AC, Wang M, Schaeffel F. Reading and myopia: Contrast polarity matters. Sci Rep. 2018 Jul 18;8(1):10840.
- Wagner S, Strasser T. Impact of text contrast polarity on the retinal activity in myopes and emmetropes using modified pattern ERG. Sci Rep. 2023 Jul 9;13(1):11101.
- Foreman J, Salim AT, Praveen A, Fonseka D, Ting DSW, Guang He M, et al. Association between digital smart device use and myopia: a systematic review and meta-analysis. Lancet Digit Health. 2021 Dec;3(12):e806–18.
- Lanca C, Saw S-M. The association between digital screen time and myopia: A systematic review. Ophthalmic Physiol Opt. 2020 Mar;40(2):216–29.
- Pärssinen O, Hemminki E, Klemetti A. Effect of spectacle use and accommodation on myopic progression: final results of a three-year randomised clinical trial among schoolchildren. Br J Ophthalmol. 1989 Jul;73(7):547–51.
- Saw SM, Chua WH, Gazzard G, Koh D, Tan DTH, Stone RA. Eye growth changes in myopic children in Singapore. Br J Ophthalmol. 2005 Nov;89(11):1489–94.
- Jones-Jordan LA, Mitchell GL, Cotter SA, Kleinstein RN, Manny RE, Mutti DO, et al. Visual activity before and after the onset of juvenile myopia. Invest Ophthalmol Vis Sci. 2011 Mar;52(3):1841–50.
- French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren: the Sydney adolescent vascular and eye study. Ophthalmology. 2013 Oct;120(10):2100–8.
- Huang P-C, Hsiao Y-C, Tsai C-Y, Tsai D-C, Chen C-W, Hsu C-C, et al. Protective behaviours of near work and time outdoors in myopia prevalence and progression in myopic children: a 2-year prospective population study. Br J Ophthalmol. 2020 Jul;104(7):956–61.
- Pärssinen O, Kauppinen M. Associations of near work time, watching TV, outdoors time, and parents’ myopia with myopia among school children based on 38-year-old historical data. Acta Ophthalmol. 2022 Mar;100(2):e430–8.
- Guan H, Yu NN, Wang H, Boswell M, Shi Y, Rozelle S, et al. Impact of various types of near work and time spent outdoors at different times of day on visual acuity and refractive error among Chinese school-going children. PLoS One. 2019 Apr 26;14(4):e0215827.
- Kinge B, Midelfart A, Jacobsen G, Rystad J. The influence of near-work on development of myopia among university students. A three-year longitudinal study among engineering students in Norway. Acta Ophthalmol Scand. 2000 Feb;78(1):26–9.
- Czepita M, Czepita D, Lubiński W. The influence of environmental factors on the prevalence of myopia in Poland. J Ophthalmol. 2017;2017:1–5.
- Guo L, Yang J, Mai J, Du X, Guo Y, Li P, et al. Prevalence and associated factors of myopia among primary and middle school-aged students: a school-based study in Guangzhou. EYE. 2016 Jun;30(6):796–804.
- Deng L, Gwiazda J, Thorn F. Children’s refractions and visual activities in the school year and summer. Optom Vis Sci. 2010 Jun;87(6):406–13.
- He X, Sankaridurg P, Xiong S, Li W, Naduvilath T, Lin S, et al. Prevalence of myopia and high myopia, and the association with education: Shanghai Child and Adolescent Large-scale Eye Study (SCALE): a cross-sectional study. BMJ Open. 2021 Dec 23;11(12):e048450.
- Ma M, Xiong S, Zhao S, Zheng Z, Sun T, Li C. COVID-19 home quarantine accelerated the progression of myopia in children aged 7 to 12 years in China. Invest Ophthalmol Vis Sci. 2021 Aug 2;62(10):37.
- García MG, Ohlendorf A, Schaeffel F, Wahl S. Dioptric defocus maps across the visual field for different indoor environments. Biomed Opt Express. 2018 Jan 1;9(1):347.
- [cited 2023 Jul 31]. Available from: https://www.college-optometrists.org/category-landing-pages/clinical-topics/myopia/myopia-management – guidance-for-optometrists
- Mountjoy E, Davies NM, Plotnikov D, Smith GD, Rodriguez S, Williams CE, et al. Education and myopia: assessing the direction of causality by mendelian randomisation. BMJ. 2018 Jun 6;361:k2022.
- Sensaki S, Sabanayagam C, Verkicharla PK, Awodele A, Tan KH, Chia A, et al. An ecologic study of trends in the prevalence of myopia in Chinese adults in Singapore born from the 1920s to 1980s. Ann Acad Med Singapore. 2017 Jun;46(6):229–36.
- How a ‘top-performing’ Asian school system formulates and implements policy: The case of Singapore.
- Morgan IG, Rose KA. Myopia and international educational performance. Ophthalmic Physiol Opt. 2013 May;33(3):329–38.
- OECD Programme for International Student Assessment (PISA) [Internet]. 2023. Available from: https://www.oecd.org/pisa/publications/pisa-2018-results.htm
- Mccurdy LE, Winterbottom KE, Mehta SS, Roberts JR. Using nature and outdoor activity to improve children’s health. Curr Probl Pediatr Adolesc Health Care. 2010;40:102–17.
- McCormick R. Does access to green space impact the mental well-being of children: A systematic review. J Pediatr Nurs. 2017 Nov;37:3–7.
- Ansari A, Pettit K, Gershoff E. Combating obesity in Head Start: Outdoor play and change in children’s body mass index. J Dev Behav Pediatr. 2015 Oct;36(8):605–12.
- Ngo C, Saw S-M, Dharani R, Flitcroft I. Does sunlight (bright lights) explain the protective effects of outdoor activity against myopia? Ophthalmic Physiol Opt. 2013 May;33(3):368–72.
- Chamarty S, Gupta SK, Dhakal R, Verkicharla PK. Is there any association between nutrition and myopia?: A systematic review. Optom Vis Sci [Internet]. 2023 Jul 3; Available from: http://dx.doi.org/10.1097/opx.0000000000002035
- Liu XN, Naduvilath TJ, Sankaridurg PR. Myopia and sleep in children—a systematic review. Sleep [Internet]. 2023 Jun 29; Available from: http://dx.doi.org/10.1093/sleep/zsad162
- Dhakal R, Shah R, Huntjens B, Verkicharla PK, Lawrenson JG. Time spent outdoors as an intervention for myopia prevention and control in children: an overview of systematic reviews. Ophthalmic Physiol Opt. 2022 May;42(3):545–58.
- Walline JJ, Robboy MW, Hilmantel G, Tarver ME, Afshari NA, Dhaliwal DK, et al. Food and Drug Administration, American Academy of Ophthalmology, American Academy of Optometry, American Association for Pediatric Ophthalmology and Strabismus, American Optometric Association, American Society of Cataract and Refractive Surgery, and Contact Lens Association of Ophthalmologists co-sponsored workshop: Controlling the progression of myopia: Contact lenses and future medical devices. Eye Contact Lens. 2018 Jul;44(4):205–11.
- Wu P-C, Chen C-T, Chang L-C, Niu Y-Z, Chen M-L, Liao L-L, et al. Increased time outdoors is followed by reversal of the long-term trend to reduced visual acuity in Taiwan primary school students. Ophthalmology. 2020 Nov;127(11):1462–9.
- Guo Y, Liu L, Lv Y, Tang P, Feng Y, Wu M, et al. Outdoor jogging and myopia progression in school children from rural Beijing: The Beijing children eye study. Transl Vis Sci Technol. 2019 May;8(3):2.
- Wu P-C, Chen C-T, Lin K-K, Sun C-C, Kuo C-N, Huang H-M, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology. 2018 Aug;125(8):1239–50.
- Hua W-J, Jin J-X, Wu X-Y, Yang J-W, Jiang X, Gao G-P, et al. Elevated light levels in schools have a protective effect on myopia. Ophthalmic Physiol Opt. 2015 May;35(3):252–62.
- Zhou Z, Chen T, Wang M, Jin L, Zhao Y, Chen S, et al. Pilot study of a novel classroom designed to prevent myopia by increasing children’s exposure to outdoor light. PLoS One. 2017 Jul 31;12(7):e0181772.
- Yi X, Wen L, Gong Y, Zhe Y, Luo Z, Pan W, et al. Outdoor scene classrooms to arrest myopia: Design and baseline characteristics. Optom Vis Sci. 2023 Jul 27;10.1097/OPX.0000000000002046.
- Nagra M, Rodriguez-Carmona M, Blane S, Huntjens B. Intra- and inter-model variability of light detection using a commercially available light sensor. J Med Syst. 2021 Feb 27;45(4):46.
- Wen L, Cheng Q, Cao Y, Li X, Pan L, Li L, et al. The Clouclip, a wearable device for measuring near-work and outdoor time: validation and comparison of objective measures with questionnaire estimates. Acta Ophthalmol. 2021 Nov;99(7):e1222–35.
- Bhandari KR, Shukla D, Mirhajianmoghadam H, Ostrin LA. Objective measures of near viewing and light exposure in schoolchildren during COVID-19. Optom Vis Sci. 2022 Mar 1;99(3):241–52.
- Apple. Apple provides powerful insights into new areas of health [Internet]. Apple. 2023 [cited 2023 Jul 31]. Available from: https://www.apple.com/uk/newsroom/2023/06/apple-provides-powerful-insights-into-new-areas-of-health/
- Jonas JB, Ang M, Cho P, Guggenheim JA, He MG, Jong M, et al. IMI prevention of myopia and its progression. Invest Ophthalmol Vis Sci. 2021 Apr 28;62(5):6.
- Perez CI, Singh K, Lin S. Relationship of lifestyle, exercise, and nutrition with glaucoma. Curr Opin Ophthalmol. 2019 Mar;30(2):82–8.
- Ong SR, Crowston JG, Loprinzi PD, Ramulu PY. Physical activity, visual impairment, and eye disease. EYE. 2018 Aug;32(8):1296–303.
- Jiang H, Wang L-N, Liu Y, Li M, Wu M, Yin Y, et al. Physical activity and risk of age-related cataract. Int J Ophthalmol. 2020 Apr 18;13(4):643–9.
- Francisco B-M, Salvador M, Amparo N. Oxidative stress in myopia. Oxid Med Cell Longev. 2015 Apr 1;2015:750637.
- Zhao F, Zhang D, Zhou Q, Zhao F, He M, Yang Z, et al. Scleral HIF-1 is a prominent regulatory candidate for genetic and environmental interactions in human myopia pathogenesis. EBioMedicine. 2020 Jul;57(102878):102878.
- Wu H, Chen W, Zhao F, Zhou Q, Reinach PS, Deng L, et al. Scleral hypoxia is a target for myopia control. Proc Natl Acad Sci U S A. 2018 Jul 24;115(30):E7091–100.
- Does the Level of Physical Activity in University Students Influence Development and Progression of Myopia?-A 2-Year Prospective Cohort Study.
- Read SA, Collins MJ, Vincent SJ. Light exposure and physical activity in myopic and emmetropic children. Optom Vis Sci. 2014 Mar;91(3):330–41.
- Lundberg K, Suhr Thykjaer A, Søgaard Hansen R, Vestergaard AH, Jacobsen N, Goldschmidt E, et al. Physical activity and myopia in Danish children-The CHAMPS Eye Study. Acta Ophthalmol. 2018 Mar;96(2):134–41.
- Suhr Thykjaer A, Lundberg K, Grauslund J. Physical activity in relation to development and progression of myopia - a systematic review. Acta Ophthalmol. 2017 Nov;95(7):651–9.
- Karthikeyan SK, Ashwini DL, Priyanka M, Nayak A, Biswas S. Physical activity, time spent outdoors, and near work in relation to myopia prevalence, incidence, and progression: An overview of systematic reviews and meta-analyses. Indian J Ophthalmol. 2022 Mar;70(3):728–39.
- Janssen X, Martin A, Hughes AR, Hill CM, Kotronoulas G, Hesketh KR. Associations of screen time, sedentary time and physical activity with sleep in under 5s: A systematic review and meta-analysis. Sleep Med Rev. 2020 Feb;49(101226):101226.
- Qin L, Chen S, Luo B, Chen Y. The effect of learning burnout on sleep quality in primary school students: The mediating role of mental health. Healthcare (Basel). 2022 Oct 19;10(10):2076.
- Ostrin LA. Ocular and systemic melatonin and the influence of light exposure. Clin Exp Optom. 2019 Mar;102(2):99–108.
- Penha AM, Burkhardt E, Schaeffel F, Feldkaemper MP. Effects of intravitreal insulin and insulin signaling cascade inhibitors on emmetropization in the chick. Mol Vis. 2012 Oct 20;18:2608–22.
- Feldkaemper MP, Neacsu I, Schaeffel F. Insulin acts as a powerful stimulator of axial myopia in chicks. Invest Ophthalmol Vis Sci. 2009 Jan 1;50(1):13.
- Cheng T, Wang J, Xiong S, Zhang B, Li Q, Xu X, et al. Association of IGF1 single-nucleotide polymorphisms with myopia in Chinese children. PeerJ. 2020 Jan 27;8(e8436):e8436.
- Rydzanicz M, Nowak DM, Karolak JA, Frajdenberg A, Podfigurna-Musielak M, Mrugacz M, et al. IGF-1 gene polymorphisms in Polish families with high-grade myopia. Mol Vis. 2011 Sep 21;17:2428–39.
- Cordain L, Eades MR, Eades MD. Hyperinsulinemic diseases of civilization: more than just Syndrome X. Comp Biochem Physiol A Mol Integr Physiol. Comp Biochem Physiol A Mol Integr Physiol. 2003;136(1):95–112.
- Li F-F, Zhu M-C, Shao Y-L, Lu F, Yi Q-Y, Huang X-F. Causal relationships between glycemic traits and myopia. Invest Ophthalmol Vis Sci. 2023 Mar 1;64(3):7.
- Fisman EZ, Tenenbaum A. Adiponectin: a manifold therapeutic target for metabolic syndrome, diabetes, and coronary disease? Cardiovasc Diabetol. 2014 Jun 23;13(1):103.
- Harb EN, Wildsoet CF. Nutritional factors and myopia: An analysis of National Health and Nutrition Examination Survey data. Optom Vis Sci. 2021 May 1;98(5):458–68.
- Berticat C, Mamouni S, Ciais A, Villain M, Raymond M, Daien V. Probability of myopia in children with high refined carbohydrates consumption in France. BMC Ophthalmol. 2020 Aug 18;20(1):337.
- Liu Z, Wang Q, Zhao Q, Gao F, Jin N, Wang D, et al. Association between whole-grain intake and myopia in chinese children: a cross-sectional epidemiological study. BMC Ophthalmol. 2023 Jan 2;23(1):1.
- Website NHS. Why we should sit less [Internet]. nhs.uk. 2023 [cited 2023 Jul 31]. Available from: https://www.nhs.uk/live-well/exercise/exercise-guidelines/why-sitting-too-much-is-bad-for-us/
- Hale L, Kirschen GW, LeBourgeois MK, Gradisar M, Garrison MM, Montgomery-Downs H, et al. Youth screen media habits and sleep. Child Adolesc Psychiatr Clin N Am. 2018 Apr;27(2):229–45.
