Convergence insufficiency (CI) is a common binocular disorder where the eyes have decreased ability to work together while carrying out close up tasks. It is defined by a remote near point convergence, higher exophoria at near than distance, and a low positive fusional vergence (PFV).1,2 Symptoms can be categorised into eye-related and performance-related issues. Examples of eye-related symptoms are eye fatigue, double vision, headaches, and blurred vision. Performance-related symptoms include loss of concentration, having to re-read, and slower reading.3,4
Background
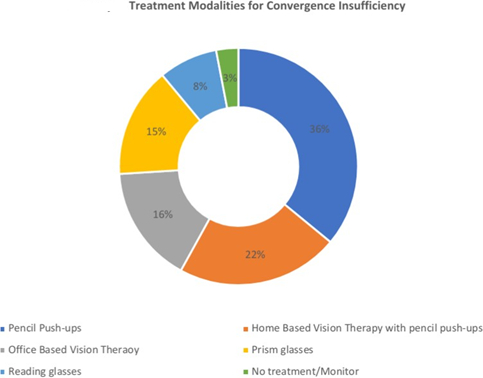
CI is not a rare condition, literature reviews have stated that CI prevalence is between 5% and 13% in school children.1,5 In adults, prevalence seems to be higher with one in six adults acquiring CI – significantly increasing in frequency with age.6,7 CI can be treated with convergence exercises – pencil push-ups (figure 1), computerised vision therapy, prism glasses or strabismus surgery if severe, but uncommon. The orthoptic exercises are thought to improve one’s fusional reserves to overcome convergence insufficiency.5
As normal physical exercise strengthens muscles, pencil push-ups (convergence exercises) strengthen eye muscles. Pencil push-ups can be done in two ways; the first way is patients are given a target either the tip of a pencil/pen and instructed to hold it at arm’s length. The pencil is then slowly drawn towards the nose, where the patient has to maintain focus and single vision.
Figure 1: Author demonstrating how pencil push-ups are carried out

If the patient sees double, they have to start again from arm’s length. The alternative method is the pencil has 6/12 sized letters and a white card is placed in the background. This time the patient works to maintain single vision when looking at the letters on the pencil while bringing it towards the nose from arm’s length.8
Pencil push-ups are very commonly prescribed as the first line of treatment for CI. Fifty-eight percent of optometrists recommend pencil push-ups or home-based vision therapy reinforced with pencil push-ups (figure 2).3 A study carried out in India also stated that pencil push-ups was the most popular treatment prescribed by 79% of ophthalmologists.9 These statistics suggest that pencil push-ups are very frequently advised across the world and emphasises the importance of evaluating its effectiveness.
In a recent systematic review conducted by Scheiman et al,10 it was concluded that office-based vergence therapy with home reinforcement is the most effective form of treatment for CI compared to home-based pencil push-ups. However, the lead author of the review is also the principal investigator of the majority of the randomised controlled trials (RCT). This raises issues of internal validity, as there is a possibility that the flaws of the studies he conducted were overlooked, invalidating any conclusions drawn.
Hence, the purpose of this dissertation is to investigate the efficacy of home-based convergence exercises for the treatment of CI in a valid and accurate manner, using a high level of research evidence that is up to date.
This review will compare the effectiveness of treatment in adults and children to explore if there is any significant difference due to the varied stages of eye development. It will also consider any contrast in the symptomatic changes and objective results seen. The high prevalence of CI, particularly in the younger subjects who have greater demands for near tasks, increases the need for this study because of the consequent academic effects CI may cause.
This text will also look into the overall successes of convergence exercises taking into account complexity, costs, and feasibility.
Figure 2: Pie chart demonstrating the distribution of commonly prescribed treatments for convergence insufficiency with a response rate of 58%3
Published Evidence
An in-depth literature search was carried out utilising the following databases:
- Cochrane Central Register of Controlled Trials
- MEDLINE
- EMBASE
Keywords searched were: ‘convergence insufficiency’ and ‘home-based treatments’ or ‘convergence exercises’ or ‘pencil-pushups’; ‘convergence insufficiency’ and ‘treatments’ or ‘therapy’; ‘convergence insufficiency’ and ‘effective treatment’ or ‘efficacy of treatment’ or ‘efficacy of therapy’; ‘convergence insufficiency’ and ‘children’ or ‘paediatric’ or ‘adults’.
Inclusion criteria
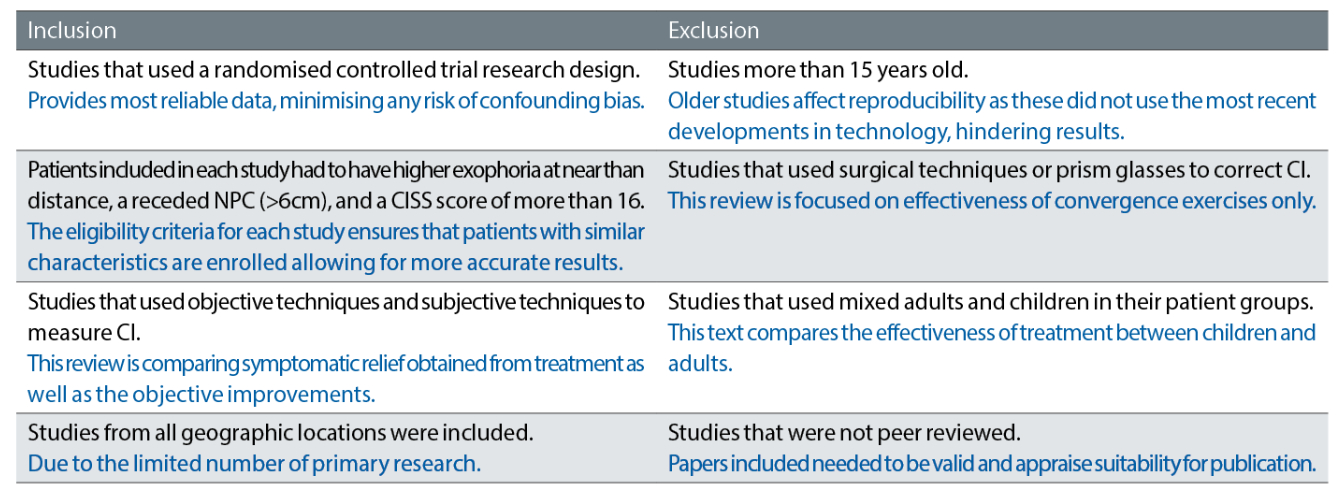
The study selection process is summarised in figure 3. Table 1 shows the inclusion and exclusion criteria used for this systematic review, with reasons for why each criterion was adopted.
Figure 3: Prisma flow chart illustrating the flow of information through the steps of this systematic review
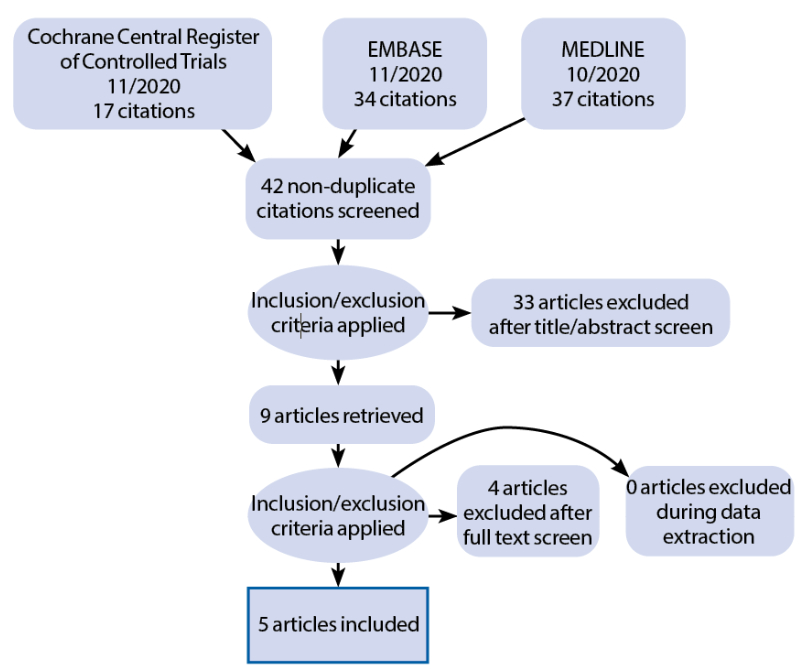
The study conducted by the convergence insufficiency treatment trial study group in 2009 was removed from this review even though criteria were satisfied.11 The study compared long-term effectiveness of treatments by enrolling patients who had previously undergone the pilot study. The number of children in the pilot study was 47, the number of children in this study was 79. It is clear that not all patients were in the pilot study and therefore cannot evaluate the long-term effectiveness of treatment if they all did not have the same. Hence, any conclusions obtained from this study are considered invalid and therefore removed.
Two other studies were also removed because they used both children and adults. Meaning that comparisons cannot be made between paediatric and adult patient groups.12,13
Table 1: Inclusion and exclusion criteria, with the reasonings in blue
Risk of bias
The five studies were then considered for any bias with the widely used Cochrane risk of bias tool 2 (RoB-2). RoB-2 (figure 4) was used instead of RoB-1 due to the issues it presented with such as being too simplistic, used inconsistently and had a higher tendency for ‘unclear risk’ to be overused as there is no algorithm for authors to follow (Lorenzo, 2019). RoB-2 has fewer domains to consider that cover all important aspects and was innovated with ‘signalling questions’ incorporated into the algorithm to facilitate judgement making.15
Figure 4: Explaining the bias domains considered in ROB- 2 for a randomised control trial14
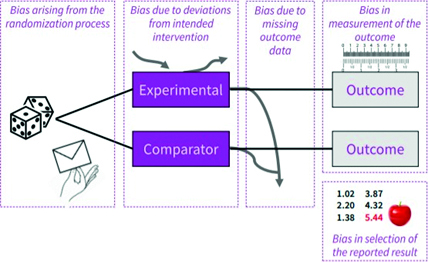
The domains explored are:
- Bias arising from the randomisation process; this is related to how participants are allocated into treatment arms and if it was concealed
- Bias due to deviations from intended interventions; this investigates if trial protocol was breached by practitioners, if the participants actually adhered to the intervention and if intervention was implemented correctly
- Bias due to missing outcome data; this considers any loss to follow up, withdrawals and other missing data (attrition bias)
- Bias in measurement of outcome; this explores how the treatment outcomes are assessed; in this review the domain was split into bias in measurement of outcome for subjective and objective measures
- Bias in selection of reported results; this reflects on the likelihood of the data to be only reported when results were in favour of the intervention or when p values were low (publication bias)16
The results of the bias analysis are summarised in figure 5. All studies randomly allocated subjects into each treatment arm. The CITT trials8, 11 used a central study website to randomise (Data Coordinating Centre) while PEDIG17 used a permuted-block randomisation method. Meaning that the investigators were unable to predict allocation, reducing any selection bias factors and confounding factors.
However, Momeni-Moghaddam et al18 used block randomisation – odd numbered participants to home-based therapy and even numbered participants to office-based therapy. By executing this method, it is more likely that the investigators may have had an impact on the designations, raising some concerns of selection bias. The CITT trials and PEDIG stated that assessing personnel for primary and secondary outcomes were masked, lowering risk of bias and treatment was concealed from patients, greatly reducing the placebo effect. Momeni-Moghaddam et al did not disclose if the researchers were masked.
Figure 5: Risk of Bias Tool 2 Cochrane Training.15 Key: + = low risk of bias; ? = some concerns; – = high risk of bias
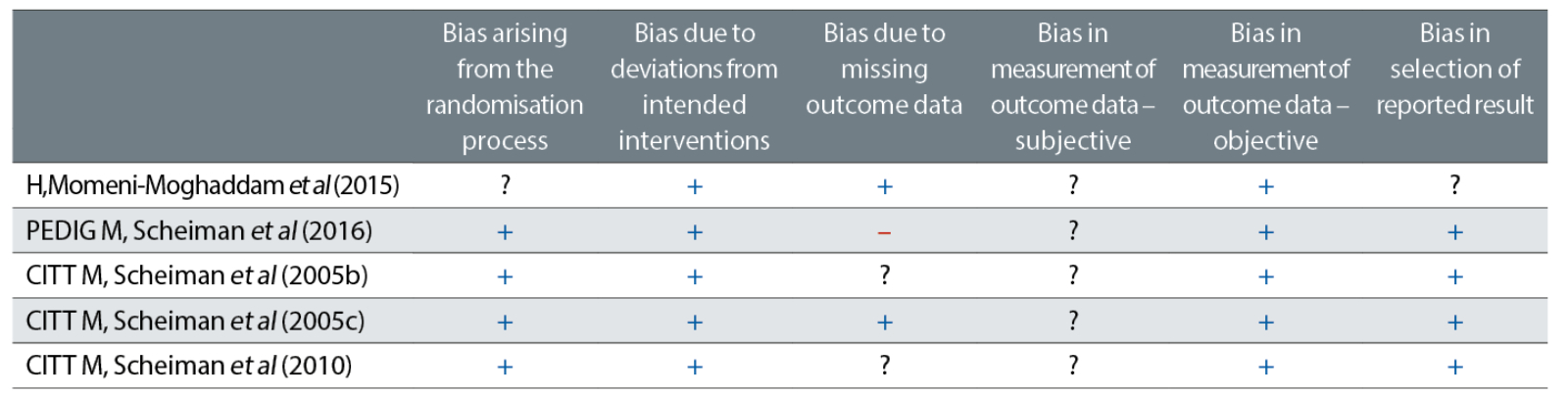
All studies had a strict eligibility and exclusion criteria, which lowers risk of deviating from intended interventions as all patients had evidence of suffering from CI. Also, each paper had laid out protocol that was precisely followed by practitioners. However, as for the home-based pencil push-ups, patients had to report on their own if they conducted the intervention or not in all of the studies. This brings up issues of response and recall bias.
Momeni-Moghaddam et al revealed no loss of subjects. The CITT trials had some missing data and is not clear if this data was accounted for. The Cochrane review, Non-surgical Interventions for convergence insufficiency, stated that ‘personal contact with the CITT trial statistician revealed that missing data were not imputed in the four CITT trials’, and therefore concluded there was no risk of bias for these studies in this domain.10
However, there was no written confirmation submitted to support the statement made, therefore this review will consider the risk of bias present. CITT (2008) stated that ‘no imputation methods were employed to account for missing data’, questioning the internal validity of this study. PEDIG (2016) reported many lost to follow cases in each of the treatment groups; 8% in home-based computer vergence, 19% in home-based near target push-up, and 30% in the home-based placebo group. The rule of thumb for lost to follow is any less than 5% can be excused as it will only lead to a negligible bias.19 In this instance, the lost to follow percentages are significantly higher, thus was judged to have high risk of bias.
All studies were carried out by experienced and highly qualified individuals therefore all objective means of obtaining data can be deemed accurate and reliable. However, the patients were asked to fill out a CISS questionnaire to obtain symptoms results. As this form of data collection is very subjective, risk of bias is higher. All CITT trials (2005b; 2005c; 2010) and PEDIG (2016) clearly stated all outcome data diminishing reporting bias. There was not enough information to assess risk of selective reporting in Momeni-Moghaddam et al (2015).
In summary, the CITT trials were rated to be at low risk of bias. Momeni-Moghaddam et al (2015) was judged to have some concerns. And PEDIG (2016) was rated at a high risk of bias.
Results
A total of 620 participants were included in this review. Children age range was seven to 18 years old and the adult age range was 19 to 30 years old. In the adult group, 70% were female, and in the children’s group 58% were female.4 RCTs were undertaken in the United States, and one in Iran.
The results are divided into paediatric (three studies) and adult (two studies) patient groups due to the differing stages of eye development and therefore the ability to intervene with treatment, as well as the varying accommodative abilities that are age-related. Each study measured the outcome in a slightly different manner as illustrated in table 2. To compare and contrast results, only near point convergence (NPC) and the convergence insufficiency symptom survey (CISS) is considered.
Table 2: Techniques used to measure effectiveness of treatments in each of the studies
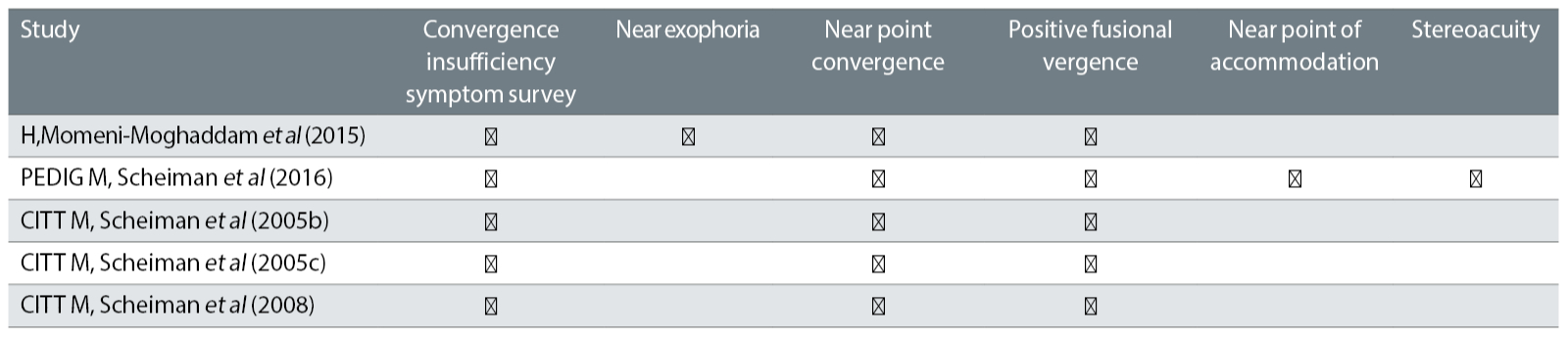
This will also be useful to explore any differences between the symptomatic relief provided by interventions in comparison to the objective improvements. Although all studies examined NPC and PFR, this review will only take into account NPC as a study conducted by Menijvar et al concluded that NPC break performed the best at diagnosing CI in patients because it is less subjective.20
As this review aims to evaluate the effectiveness of home-based convergence exercises (pencil push-ups), comparisons will only be made between home-based pencil push-up groups and office-based therapy groups or home-based placebo groups, for NPC and CISS.
Paediatric studies
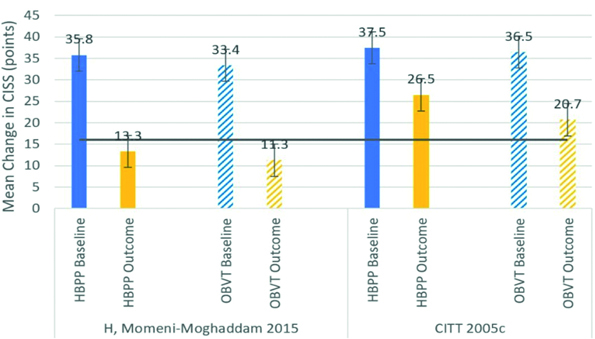
Table 3 consists of the RCTs included in this review for paediatric patients; including participants, groups, and results for near point convergence (NPC) and convergence insufficiency symptom score (CISS).
Table 3: Data presented as mean change in NPC and CISS from baseline to end of treatment. - symbol means negative change (improvement) in NPC (cm) and CISS score. Percentage change calculated as [ (New value - Original value)/ Original value ] to allow both objective and subjective results to be easily comparable to 3 s.f. Green values are statistically significant results, confidence level is greater than or equal to 95% (p≤0.05). Red values are statistically insignificant results, confidence level less than 95% (≥0.05). Blue writing highlights groups of each study that was compared in the results
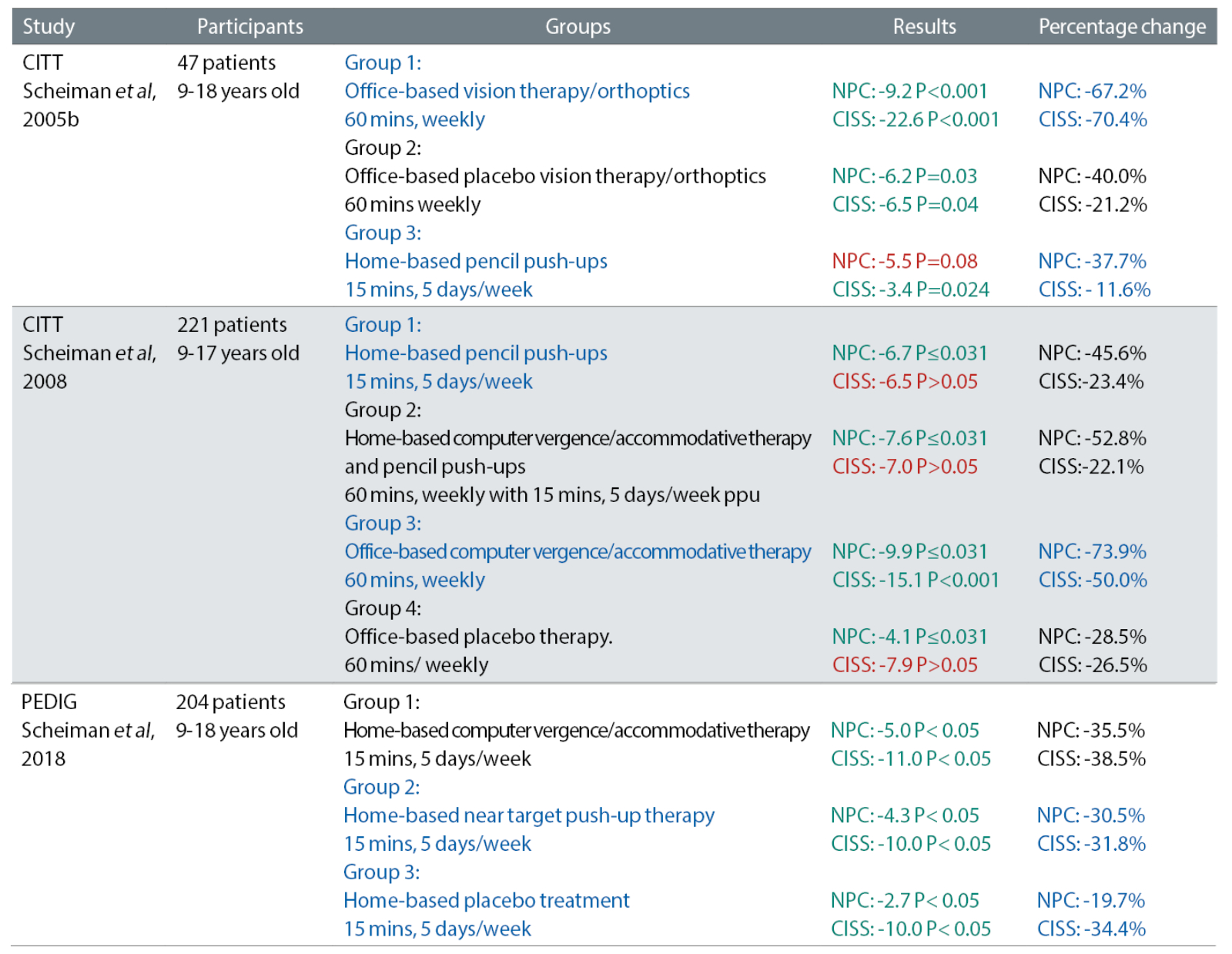
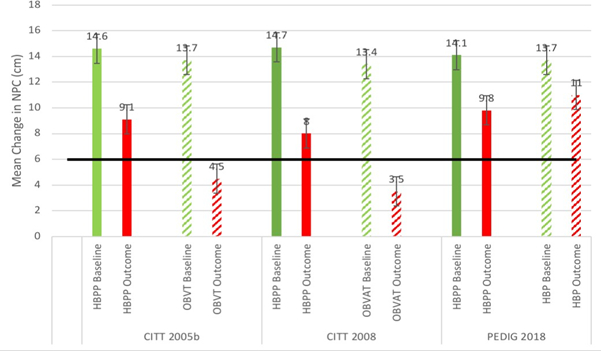
Near point convergence
The CITT (2005b) and CITT (2008) compared home-based pencil push-ups (HBPP) against office-based vision therapy (OBVT/OBVAT). CITT (2005b) found OBVT to be more effective than HBPP as there was a greater decrease (improvement) in NPC from baseline measurements to final outcome measurements taken after 12 weeks. In OBVT there was a decrease of 9.2cm (p<0.001) as opposed to 5.5cm (p=0.8) in the HBPP. In the CITT (2008) study, OBVAT had 1.24 times greater improvement in NPC compared to HBPP with both improvements statistically significant (p≤0.031).
The PEDIG (2018) compared HBPP to placebo treatment, and found that HBPP was more effective with a larger change in NPC 5.0cm as opposed to 2.7cm – almost half the Improvement. Results, summarised in figure 6, were considered statistically significant with p<0.05 for both interventions.
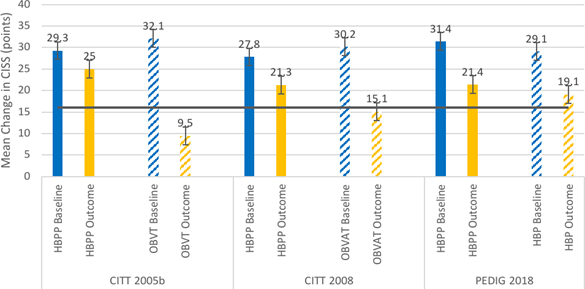
Figure 6: Bar graph showing the difference of NPC (cm) at baseline and outcome for each group, in each of the studies. (CITT, 2005b; CITT, 2008; PEDIG, 2018). Black line indicates the normal NPC value of 6cm
Convergence insufficiency symptom score (CISS)
CITT (2005b) and CITT (2008) found that OBVT was much more effective at improving symptoms of CI measured by CISS. CITT (2005b) revealed a decrease (improvement) of 22.6 points in the OBVAT group (p<0.001), compared to a decrease of just 3.4 points in the HBPP group (p=0.024). OBVT had 6.65 times greater improvement than HBPP. CITT (2008) found statistically insignificant results (p>0.05) for the improvement of CISS in the HBPP group with a change of 6.5 points. In the OBVAT group, CISS improved by 15.1 points (p<0.001).
PEDIG (2018) compared HBPP to placebo interventions and found that HBPP was as effective at reducing CI symptoms as the placebo group. Both treatment arms revealed a 10.0 points decrease and both statistically significant (p<0.05).
Figure 7: Bar graph showing the difference of CISS (points) at baseline and outcome for each group, in each of the studies. (CITT, 2005b; CITT, 2008; PEDIG, 2018). Black line indicating the normal CISS score of 16 points
Adult studies
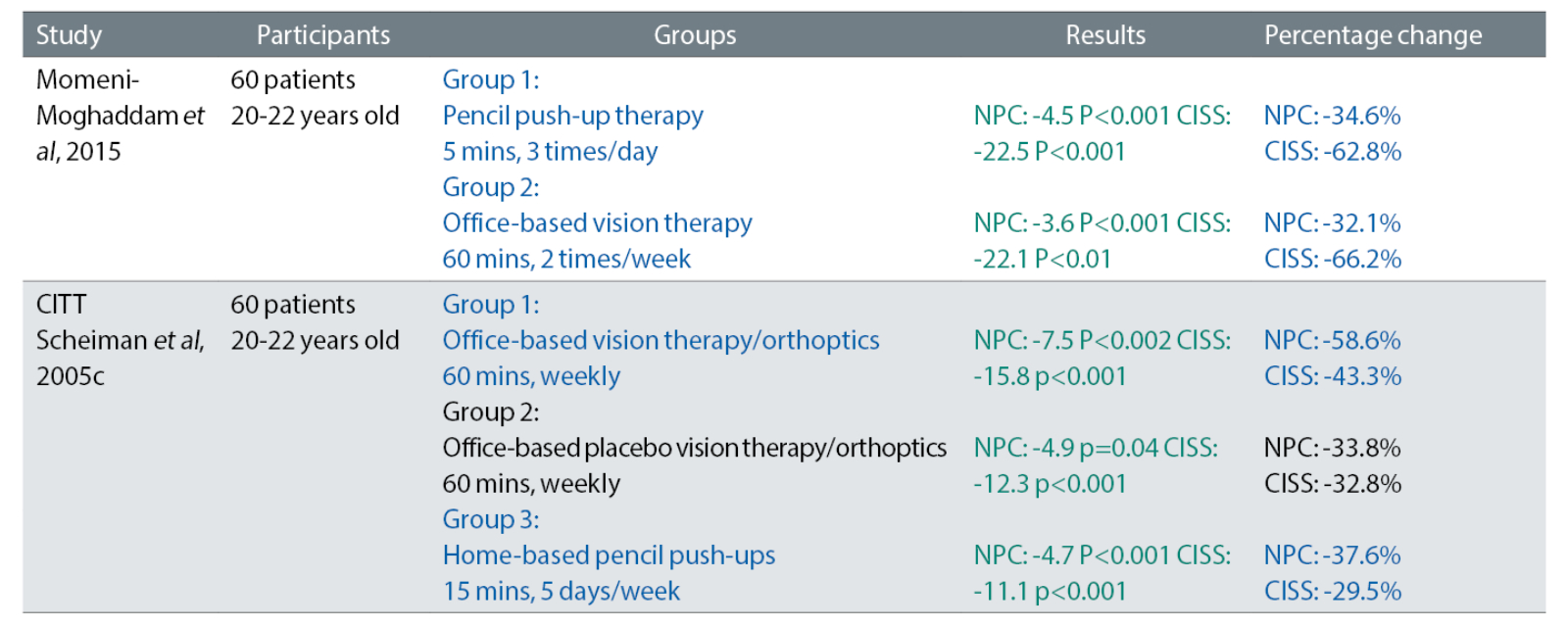
Table 4 shows the RCTs included in this review for adult patients; including participants, groups, and results for NPC and CISS.
Table 4: Data presented as mean change in NPC and CISS. - symbol means negative change (improvement) in NPC (cm) and CISS score. Percentage change calculated as [ (New value - Original value)/ Original value ] with mean differences to allow both objective and subjective results to be easily comparable to 3 s.f. Green values are statistically significant results with confidence level greater than or equal to 95% (p≤0.05). Blue writing highlighted groups within studies that were compared in results
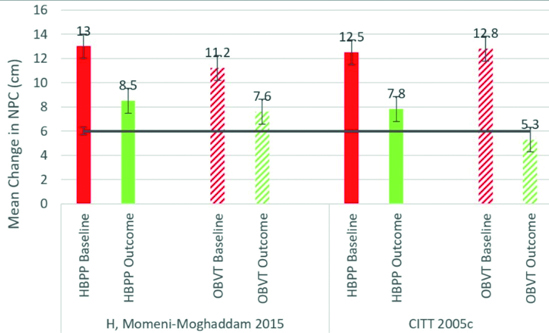
Near point convergence (NPC)
Both studies compared home-based pencil push-ups (HBPP) to office-based vision/orthoptic therapy (OBVT). Momeni-Moghaddam et al (2015) revealed that HBPP was more effective at reducing (improving) NPC with statistically significant results. Where the HBPP group had a change of 4.5cm (p<0.001) while the OBVT group had a change of 3.6cm (p<0.001). However, CITT (2005c) found that the OBVT intervention performed better with an NPC improvement of 7.5cm (p<0.002), in comparison to a 4.7cm reduction in the HBPP group (p<0.001). Results are summarised in figure 8.
Figure 8: Bar graph showing the difference of NPC (cm) at baseline and outcome for each group, in each of the studies. (Momeni-Moghaddam, 2015; CITT, 2005c). Black line illustrating normal NPC value of 6cm
Convergence insufficiency symptom score (CISS)
Momeni-Moghaddam et al (2015) found that HBPP was better at reducing symptoms of CI measured using CISS, whereas CITT 2005c found contrasting results. Momeni-Moghaddam et al (2015) revealed a 22.5 point decrease in CISS in the HBPP group (p<0.001) compared to 22.1 in the OBVT group (p<0.001). CITT (2005c) found CISS was reduced more by OBVT by 15.8 (p<0.001) in contrast to a 11.1 decrease in the HBPP group (p<0.001). Results are summarised in figure 9.
Figure 9: Bar graph showing the difference of CISS (points) at baseline and outcome for each group, in each of the studies. (Momeni-Moghaddam, 2015; CITT, 2005c). Black line illustrates normal CISS score of 16 points
Discussion
This review set out to evaluate the effectiveness of convergence exercises – pencil push-ups (PPU) as treatment for convergence insufficiency (CI). As shown by the results above, office-based vision therapy (OBVT) performed better at treating CI in both paediatric and adult patients. This result was consistent across objective, near point convergence (NPC), and subjective, the convergence insufficiency symptom score (CISS) measures with the exception of a few results and the Momeni-Moghaddam et al (2015) study.
Paediatrics
The highest level of research evidence (CITT, 2005b; CITT 2008) demonstrated that OBVT performed better than home-based pencil push-ups (HBPP) at lowering NPC values. Results were statistically and clinically significant, as anything less than 6cm of NPC is considered normal or less likely to be symptomatic (Hayes et al, 1998). The HBPP group in the CITT (2005b) study had statistically insignificant results, suggesting a weak correlation between the variables. Indicating that any change found in the HBPP group is more likely to be due to chance rather than as a result of the intervention.
A similar trend was seen with the subjective improvements measured with CISS. OBVT performed remarkably better at reducing symptoms, compared to HBPP. The CITT (2008) study revealed insignificant results in the HBPP group. As the sample size was large this was less likely to be the cause for insignificant results inferring that the change in outcome measures were not observed as a result of pencil push-ups.
PEDIG (2018), rated at high risk of bias, found that HBPP was more effective than placebo treatment at decreasing NPC. Only a difference of 1.2cm was noted between the groups, while statistically significant these results become insignificant when considered at a clinical level.
This calls into question the effectiveness of pencil push-ups due to the inadequate differences perceived between placebo and pencil push-ups. For the CISS, the same point decrease was revealed. It should be acknowledged that the findings may have been masked by the placebo effect, where patients’ positive belief in the treatment resolves any analgesia or symptomatic issues.21 This means that the results from the placebo group suggest no real treatment effect was seen.
All paediatric studies stated that the pencil push-ups were clearly demonstrated and practitioners ensured participants’ understanding. Subjects were aged nine to 18 years, so comprehension of the intervention is questionable in young subjects. Practitioners could have instructed and educated parents or guardians to ensure understanding therefore enhancing treatment compliance. It was not mentioned if patients were age-matched in each group. This is important as older patients will have understood the exercises better and conducted them correctly. At the same time, older patients can find carrying out the pencil push-ups tedious, becoming less motivated to do them.
Adults
Higher level research evidence revealed findings that coincide with trends appreciated in paediatric patients, where OBVT showed better improvements in both NPC and CISS. Contrastingly, Momeni-Moghaddam et al (2015), judged to have some concerns for bias, found that HBPP performed better for subjective and objective measures.
It should be noted that the participant population in this study was university students, possibly studying optometry or medicine, as this was not something mentioned in their exclusion criteria. One could argue that if the patients were optometry/medical students, they would have better understanding of the exercises and, therefore, are more likely to execute the interventions as they are aware of the benefits and possibly for the purpose of research.
Perhaps, if patients were compliant HBPP would be an effective form of treatment. With regard to the subjective improvements minimal change was seen. While HBPP performed better, it was only by 0.4 points, suggesting that this result was not a notable enough difference when considering the effectiveness of HBPP.
Overall
The conclusions drawn are in agreement with other reviews conducted in the same field of research,2, 10, 22 as well as the recent update on the meta-analysis Cochrane review.
All studies (adults and paediatric) specified that outcome measures were taken three times at each visit allowing for a mean calculation, increasing accuracy of results. The sample sizes were acceptable across studies as they were greater than 50, which is considered sufficient to obtain a firm mean and standard deviations.23 Only CITT (2005b) and CITT (2005c) where sample size was 47 and 46 respectively were below this threshold.
The disadvantage of using a small sample size is the conclusions drawn may not be representative of the whole population, as data is more prone to error skewing. A small sample size may not be able to detect an effect,24 and thus impacts effective overall reliability and validity. The fact that a high number of participants dropped out in the PEDIG (2016) study is another limitation as this poses a greater likelihood of attrition bias.
The convergence insufficiency symptom survey was used as a primary outcome measure in the studies, which was found to be a valid tool to use on both adults and children.25, 26 While this may be true, patients had to repeat the survey at every follow up where after a few times, patients will become familiar with the questions and the expected responses. Thus, patients may tailor their answers leading to the placebo effect being seen and response bias affecting data.
Using an objective outcome measure only approach can aid in overcoming any subjective variations. However, CI is very much a symptom-based condition therefore it is important not to discount symptomatic relief when evaluating treatments.
The length of treatment was 12 weeks in the CITT trials and PEDIG (2018) and eight weeks in Momeni-Moghaddam et al (2015). A positive relationship between treatment lengths and improvements was not seen causing a lack of clarity when deciding preferred treatment lengths. A long-term large-scale randomised control trial is required to determine an optimum length of therapy.
Another element of evaluating the efficacy of treatments is to note if patients relapsed and signs and symptoms of CI returned after stopping treatments. Finally, the costs of the interventions were not specified; OBVT is more likely to be expensive due to the longer treatment time in practise and the equipment used. Cost is an important aspect to review as it is responsible for the overall feasibility and consideration of treatment.
In order to evaluate home-based treatments, patient-led monitoring is necessary. The studies considered adopted calendars or log books, which carry a higher risk of bias due to patients providing inaccurate or untruthful answers as a result of response or recall bias. Although treatment adherence was said to be around the 70% to 80% mark, these percentages may not be of true reflection for the aforementioned reasons.
When it comes to therapies that are dependent on patient compliance, there is always an element of non-adherence to account for. For instance, in amblyopia patching treatment, only 50% of patients were found to be compliant.27, 28 The main way to overcome this is to educate patients on the importance of compliance and the benefit they stand to gain, which can be utilised as motivation.
The current Covid-19 pandemic restrictions have led to the preferred treatment where less clinic/office time is required. This covers the underlying factor that face-to-face treatments had previously required taking time off school or work making this more inconvenient and costly. The pandemic forced a cultural shift in clinics where many things previously done in person had to be modified and implemented online via zoom or teams for example.
This has become beneficial as it can be incorporated into home-based therapies, allowing practitioners to observe and feedback on patients carrying out these exercises virtually, subsequently increasing compliance and effectiveness of the therapies. A practitioner could conduct the initial session with follow-ups being carried out by junior staff to better utilise the practitioner’s time.
An alternative method that could be considered is to develop an app or software that the patient can download and use to aid with HBPP. The app would perhaps send notifications for when patients should carry out the exercise and they could take a video of themselves doing it for the practitioner to view later, eye tracking software could be used to get quantitative measurements too.
This use of technology would heighten the effectiveness of pencil push-ups and is much more cost effective. Mohan et al investigated the effectiveness of using smartphone-based exercises along with a myopic correction for CI treatment.29 Statistically significant improvements in NPC, PFV and near exophoria were seen. These findings suggest there could be an exciting position for technology in the treatment of CI, intensifying the need for further research to be carried out.
Conclusion
In conclusion, the studies showed that OBVT carries more benefits with improving symptoms of CI and the objective advancements in both paediatric and adult cases. Research for adults is limited in quantity thus a strong interpretation cannot be inferred. It could be said that HBPP if carried out correctly with good compliance is an excellent intervention due to simplicity and affordability, having a role in treatment of CI. There is hope for more technologically advanced forms of therapy for CI, which will require more research to emerge in the future.
- The author would like to thank my supervisor Dr Miriam Conway for all her help and support.
- This is an edited version of the 2021 City University/Optician Best Dissertation prize-winner written by the author as a final year undergraduate.
References
- Rouse, M., Hyman, L., Hussein, M. and Solan, H., (1998) Frequency of Convergence Insufficiency in Optometry Clinic Settings. Optometry and Vision Science, 75(2), pp.88-96
- Lavrich, J., (2010) Convergence insufficiency and its current treatment. Current Opinion in Ophthalmology, 21(5), pp.356-360
- Scheiman, M., Cooper, J., Mitchell, G., Land, P., Cotter, S., Borsting, E., London, R. and Rouse, M., (2002) A Survey of Treatment Modalities for Convergence Insufficiency. Optometry and Vision Science, 79(3), pp.151-157
- Cooper, J., and Jamal, N.,(2012) Convergence insufficiency-a major review. Optometry. Apr 30;83(4):137-58
- Goering M, Drennan KB, Moshirfar M. Convergence Insufficiency, (2020) In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554390/ [Accessed 28 December 2020]
- Porcar, E. and Martinez-Palomera, A., (1997) Prevalence of General Binocular Dysfunctions in a Population of University Students. Optometry and Vision Science, 74(2), pp.111-113
- Ghadban, R., Martinez, J. M., Diehl, N. N., & Mohney, B. G. (2015). The incidence and clinical characteristics of adult-onset convergence insufficiency. Ophthalmology, 122(5), 1056–1059
- Convergence Insufficiency Treatment Trial Study Group, (2008) Randomized Clinical Trial of Treatments for Symptomatic Convergence Insufficiency in Children. Archives of Ophthalmology, 126(10), p.1336
- Sharma, P., Saxena, R., Khanduja, S. and Patwardhan, S., (2008) Preferred clinical practice in convergence insufficiency in India: A survey. Indian Journal of Ophthalmology, 56(4), p.303.
- 10Scheiman, M., Gwiazda, J., & Li, T. (2011) Non-surgical interventions for convergence insufficiency. The Cochrane database of systematic reviews, (3), CD006768
- Convergence Insufficiency Treatment Trial Study Group, (2005) A Randomized Clinical Trial of Treatments for Convergence Insufficiency in Children. Archives of Ophthalmology, 123(1), p.14
- Aletaha, M., Daneshvar, F., Mosallaei, M., Bagheri, A., Khalili, MR., (2018) Comparison of three vision therapy approaches for convergence insufficiency. Journal of Ophthalmic and Vision Research;13(3):307-14
- Singh, A., Saxena, V., Yadav, S., Agrawal, A., Ramawat, A., Samanta, R., Panyala, R. and Kumar, B., (2021) Comparison of home-based pencil push-up therapy and office-based orthoptic therapy in symptomatic patients of convergence insufficiency: a randomized controlled trial. International Ophthalmology, 41(4), pp.1327-1336
- Training.cochrane.org. 2021. RoB 2 Domain 2: Bias due to deviations from the intended interventions. [online] Available at: https://training.cochrane.org/resource/rob-2-domain-2-bias-due-deviations-intended-interventions [Accessed 25 March 2021]
- Sterne, J., Savović, J., Page, M., Elbers, R., Blencowe, N., Boutron, I., Cates, C., Cheng, H., Corbett, M., Eldridge, S., Emberson, J., Hernán, M., Hopewell, S., Hróbjartsson, A., Junqueira, D., Jüni, P., Kirkham, J., Lasserson, T., Li, T., McAleenan, A., Reeves, B., Shepperd, S., Shrier, I., Stewart, L., Tilling, K., White, I., Whiting, P. and Higgins, J., (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ, p.l4898
- Higgins, J., Altman, D., Gotzsche, P., Juni, P., Moher, D., Oxman, A., Savovic, J., Schulz, K., Weeks, L. and Sterne, J., (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343(oct18 2), pp.d5928-d5928
- Paediatric Eye Disease Investigator Group, 2018. Home-Based Therapy for Symptomatic Convergence Insufficiency in Children: A Randomized Clinical Trial. Optometry and Vision Science, 93(12), pp.1457-1465
- Momeni-Moghaddam, H., Kundart, J., Azimi, A. and Hassanyani, F., 2015. The effectiveness of home-based pencil push-up therapy versus office-based therapy for the treatment of symptomatic convergence insufficiency in young adults. Middle East African Journal of Ophthalmology, 22(1), p.97
- Dettori, J., (2011) Loss to follow-up. Evidence-Based Spine-Care Journal, 2(01), pp.7-10
- Menjivar, A., Kulp, M., Mitchell, G., Toole, A. and Reuter, K., (2018) Screening for convergence insufficiency in school-age children. Clinical and Experimental Optometry, 101(4), pp.578-584
- Colloca, L., (2019) The placebo effect in pain therapies. Annual Review of Pharmacology and Toxicology, 59(1), pp.191-211
- Scheiman, M., Rouse, M., Kulp, M., Cotter, S., Hertle, R. and Mitchell, G., (2009) Treatment of Convergence Insufficiency in Childhood: A Current Perspective. Optometry and Vision Science, 86(5), pp.420-428
- Piovesana, A. and Senior, G., (2016) How Small Is Big: Sample Size and Skewness. Assessment, 25(6), pp.793-800
- Noordzij, M., Dekker, F., Zoccali, C. and Jager, K., (2011) Sample Size Calculations. Nephron Clinical Practice, 118(4), pp.c319-c323
- Borsting, E., Rouse, M., Mitchell, G., Scheiman, M., Cotter, S., Cooper, J., Kulp, M. and London, R., (2003) Validity and Reliability of the Revised Convergence Insufficiency Symptom Survey in Children Aged 9 to 18 Years. Optometry and Vision Science, 80(12), pp.832-838
- Rouse, M., Borsting, E., Lynn Mitchell, G., Scheiman, M., Cotter, S., Cooper, J., Kulp, M., London, R. and Wensveen, J., (2004) Validity and reliability of the revised convergence insufficiency symptom survey in adults. Ophthalmic and Physiological Optics, 24(5), pp.384-390
- Ganesh, A., Al-Zuhaibi, S., Al-Harthi, I., Cooymans, P., Al-Busaidi, A. and Al-Farsi, Y., (2009) Compliance of amblyopic patients with occlusion therapy: A pilot study. Oman Journal of Ophthalmology, 2(2), p.67
- Wallace, M., Stewart, C., Moseley, M., Stephens, D. and Fielder, A., (2016) Treatment of amblyopia using personalized dosing strategies: Statistical modelling and clinical implementation. Strabismus, 24(4), pp.161-168
- Mohan, A., Kaur, N., Sen, P., Jain, E. and Gajraj, M., (2019) Efficacy of Smartphone-based Exercises in Conjunction with Modified Glasses Prescription in the Treatment of Convergence Insufficiency and Fusion Weakness. Journal of Binocular Vision and Ocular Motility, 69(1), pp.30-33
