 There are now an ever-increasing number of options that eye care practitioners (ECPs) can offer to their myopic paediatric patients with a view to slowing myopia’s predictable progression.
There are now an ever-increasing number of options that eye care practitioners (ECPs) can offer to their myopic paediatric patients with a view to slowing myopia’s predictable progression.
There have been an increase in available options for myopia management spectacle lenses meaning patients now have orthokeratology, soft contact lens, and spectacles lens options when considering myopia management. In addition, the importance of lifestyle advice, time spent outdoors discussions being part of all conversations with patients regarding myopia management treatment options.
Myopia management poses a number of dilemmas in terms of the application of ethical and professional standards.
GOC Standards of Practice require registered opticians to be evidence-based reflective practitioners and to ensure they gain valid consent from their patients and/or their parents/carers.1 ECPs must inform patients of the likely progression of their myopia, any interventions that may slow its progression, and the potential consequences of the various options patients (and their carers) have open to them.
Not so long ago, at face to face Continuing Professional Development (CPD) discussion workshops registrants would argue whether they should mention myopia control lenses if they worked in a practice that did not offer them.
This is supported by evidence from Moore et al a retrospective data analysis investigating prescribing patterns of soft myopia control contact lenses in Ireland, which showed that as few as one third of practices were offering any myopia management interventions as recently as 2021.2
Patients, parents and carers have the right to decide what treatment they follow based on informed choices, this requires an on-going dialogue between patient and ECP ensuring information is presented clearly and accurately in a way that is understood and supported by written information.3,4
If you had a form of cancer that could be treated by radical excision surgery (eg mastectomy, resection of the bowel, etc), chemotherapy or radiotherapy, or a combination of all three. Would you expect the oncologist to only carry out surgery because that was what he specialised in and not offer the alternatives?
Faced with that kind of argument the consensus quickly came round to the opinion that we all have a duty to appraise patients/parents of the risks associated with high myopia and to mention myopia management options whether or not it is something we can personally offer.
This opinion seems to have also gained traction at corporate level as all UK practices now seem to offer myopia management contact lenses, and most offer at least one spectacle lens that claims to slow the progression of myopia.
The question that is now being posed is whether, given the large range of alternatives, ECPs have a duty to offer more than one spectacle lens option for myopia control in the same way that most seem to offer more than one contact lens option? The answer is, as always, it depends.
ECPs are required to keep their knowledge and skills up to date and must engage in CPD so that they are aware of current good practice, able to take into account relevant developments in clinical research, and apply this to the care they provide.5 However, deciding whether a range of spectacle lenses should be offered is easier said than done.
Keeping to a single supplier for almost all spectacle lenses is a common business strategy in optics as it allows for the best possible purchasing price, which in turn can be passed on to the patient, and also provides a clear differentiator from neighbouring practices.
It is likely that the new products that have become available from almost all major lens manufacturers will simply allow brand loyal opticians and consumers to stay with that manufacturer, but should ECPs offer a range of myopia management spectacle lens options or simply stay loyal to one?
This question is quite difficult to answer because although there is much research it mainly concentrates on comparing a single myopia management option to a control group of myopes wearing conventional single vision spectacles or contact lenses and does not directly compare one myopia management to another.
Probably the best source of data and research into myopia management options is the International Myopia Institute (IMI), which formed in 2015 following a presentation by the Brien Holden Vision Institute (BHVI) to the World Health Organisation (WHO).
The IMI (myopiainstitute.org) exists to advance myopia research and education to prevent future blindness, publishing detailed clinical data, and useful summaries of all interventions relating to myopia management including those that might be considered historical as well as those at the cutting edge of new research to aid ECPs, governments, educators, and the general public understand myopia.
IMI Series Three has been published this year myopiainstitute.org/imi-white-papers-clinical-summaries/.
Myopia management spectacles with a growing evidence base demonstrating similar efficacy to myopia management soft contact lenses are now being prescribed with greater frequency compared to myopia management soft contact lenses (overall 14% and 9% respectively).6
Limitations in Myopia Research
It is difficult to make direct comparisons between research papers, and as a result it is not really possible to say, for example, which spectacle lens or contact lens is ‘the best’ in terms of its ability to slow myopia progression.
Studies differ in terms of sample size, methodology, refraction technique, and even in terms of defining myopia and at what point it becomes high. In an attempt to encourage standardisation, the IMI has defined high myopia as ≤-6.00D, meaning -6.00D or more myopic so it is hoped that there will be some consistency in the future.7
In these authors’ opinion (which it is hoped will stimulate some academic debate) the use of spherical equivalent refraction (SER) may be a particular source of error or inconsistency in some research results.
While simple myopia can clearly be axial (due to a longer than normal eyeball) or refractive (due to an overly curved cornea) or a combination of the two, significant astigmatism must, by definition, be refractive in nature caused by a cornea that is shaped like the side of a rugby ball, or a tilted/malformed crystalline lens.
It should be born in mind that myopic astigmats cannot see clearly at any distance whereas simple myopes can see clearly up to the reciprocal of their prescription and therefore they may be subject to different mechanisms of eye growth and visual development.
It would appear wise therefore for researchers to limit their subjects to patients with the level of astigmatism typically corrected by spherical contact lenses rather than torics (ie up to 0.75 or 1.00D). Most studies do impose a limit on astigmatism with clear study inclusion criteria but each can differ.8
MiSight RCT applied inclusion criteria for SER between -0.75D and -4.00D astigmatism ≤-0.75DC and anisometropia <1.00D.9 DIMS spectacle lens RCT used inclusion criteria for SER -1.00 to -4.00D astigmatism and anisometropia 1.50D or less.
Significant astigmatism, especially if oblique, could be considered a confounding variable that makes interpretation of results difficult as the child will experience form deprivation and is surely at greater risk of amblyopia.
Simple myopia (with little or no astigmatism) on the other hand leads to a fixation on close tasks, sitting closer to the TV, becoming a bookworm etc, if uncorrected, but does not lead to amblyopia since form deprivation does not occur at near distances.
The IMI clinical Myopia Control Trials Report10 felt that as the amount of astigmatism was restricted in each trial and in most cases was no greater than 1.50D whether spherical or spherical equivalent refraction was used for inclusion criteria was ‘inconsequential’ and that all but orthokeratology studies used spherical equivalent refraction for myopic progression.
The public health burden of myopia
There is now clear evidence that high myopia and the associated sight threatening complications are a considerable burden on health systems worldwide, a burden that was set to double by 2050 if something could not be done to turn the tide.
Thankfully, a plethora of myopia management solutions have been developed. These solutions are more necessary than ever since myopia is reaching pandemic proportions with predictions that half of all people worldwide will be myopic by 2050.11
Already 83% of young adults in Singapore are myopic, and around one fifth of them are expected to progress to high myopia by 2050. Globally around 10% are expected to have high myopia with consequences of serious pathology including retinal detachment, myopic maculopathy, glaucoma and cataract.
Whether myopia management can reduce the future risk of sight threatening ocular pathology does require more direct evidence but population-based studies have shown that slowing myopia by 1.00D can reduce myopic maculopathy by 40%.12
The risks for those with high myopia ≤-6.00D are significant. Flitcroft13 showed the odds ratio of pathology for even 1.00D myopia can double risk of PSC cataract and myopic maculopathy compared to an emmetrope.
Patients with greater than 9.00 dioptres of myopia are over 300 times more likely to develop maculopathy and 44 times more likely to suffer a retinal detachment than an emmetrope.
The fact that there are safe and effective contact lens and spectacle lens treatment options highlights discussions with those at risk of myopia and myopia progression should take place at earliest possible opportunity. Professional guidance from both the College of Optometrists and the Association of British Dispensing Opticians (ABDO) includes guidance that discussions with patients/parents should take place.14,15
Some ECPs may feel these guidelines do not go far enough while others still want to see more evidence. It should be remembered that professional bodies have to carefully consider all the available evidence before making guidance statements.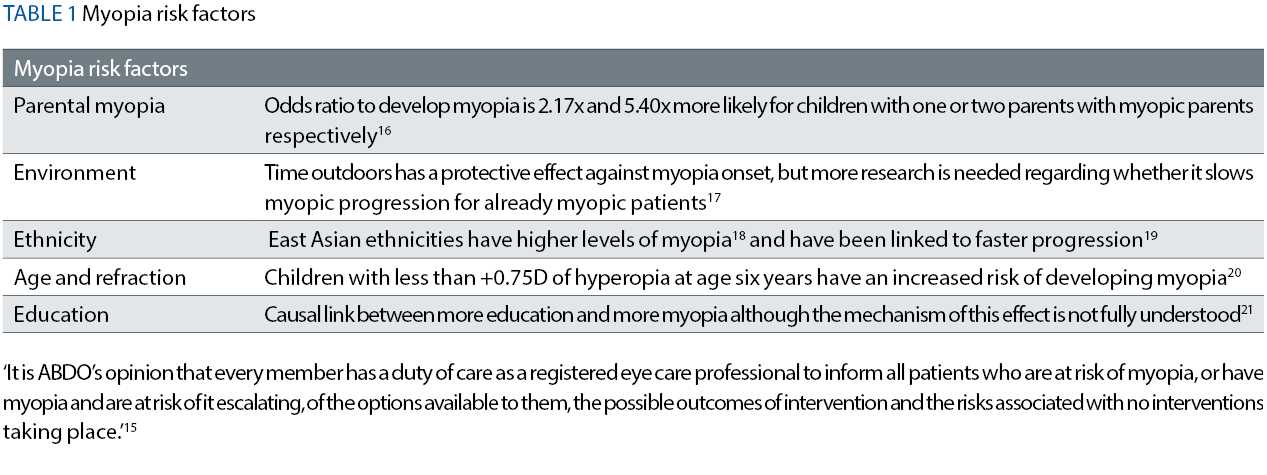
There is evidence that helps to identify those patients that are subject to a greater risk of myopia (see Table 1), another useful resource is the Predicting Myopia Onset and Progression (PreMO) evidence based risk indicator derived from NICER Study outcomes, and as stated is best suited to primary school children of white ethnicity living in the UK. ulster.ac.uk/__data/assets/pdf_file/0011/826184/PreMO-risk-indicator-for-website.pdf.
There are numerous myopia progression and management articles that have appeared in optical journals in recent years regarding the role of relative peripheral refraction in stimulating axial eye growth, and this is the mechanism upon which most contact lens and spectacle lens treatment options are based.
Figure 5: Hoya MiyoSmart, showing defocus incorporated multiple segments (DIMS) lenslets

Figure 6: Defocus areas in Rodenstock MyCon lenses
Previously discussed spectacle lens options:
- Miyosmart (Hoya) (figure 5)
- Mycon (Rodenstock) (figure 6)
- My-Nor (Norville)
- MyoCare and MyoCare S (Zeiss)
- Stellast (Essilor)
- Vision DOT 0.2 (SightGlass)
New lenses introduced since last update:
- Optimyope from Optimum
- Imperium from Caledonian Optical
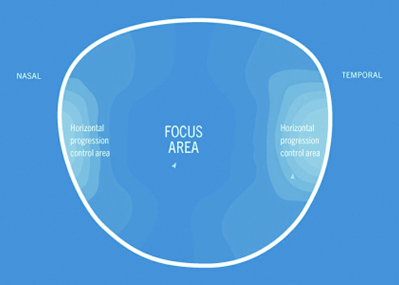
Although the authors have not yet experienced these lenses, they are reported to work similarly to Rodenstock and Norville options with temporal and nasal peripheral defocus zones rather than 360 degrees and a comprehensive range of lens materials.
As Optician went to press we learned of a new My-O-Sense lens exclusively for independent opticians from Waterside Optical and will update readers in due course. Learn more at waterside-labs.co.uk/blog/new-myopia-control-solutionavailable-now.
Peripheral defocus (myopia control) lenses
Relative peripheral refraction role in driving eye growth.22 See figure 1 and figure 2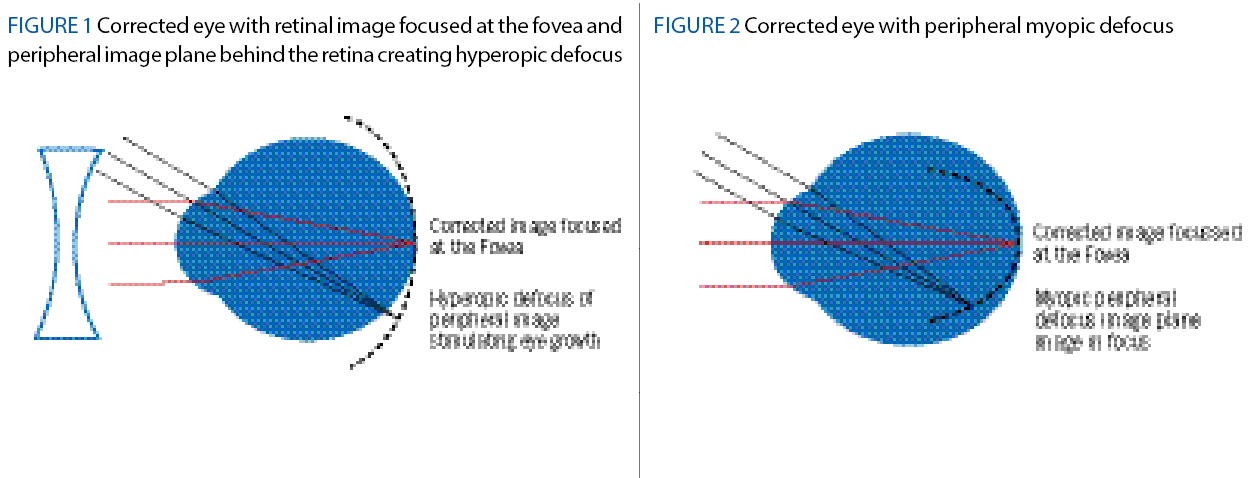
The previous Optician article (July 28, 2023) has already provided detailed information on commercially available spectacle lens designs but as the authors want to stress the importance of fitting accuracy, which ensures optimum efficacy and patient comfort, the following detail has been included in this article.
The simultaneous vision design means that compared to myopia management contact lenses the patient can experience poorer optical performance, when not looking close to straight ahead in the primary position and therefore depends on head movement rather than eye movement to look up, down or to the left or right.23
Nevertheless, children seem to easily adapt to this providing the lenses have been dispensed optimally and the importance of accurately fitting these lens designs in accordance with manufacturers guidelines cannot be stressed enough, as poorly fitted spectacle frames and inaccurate centration will impact efficacy of the treatment.
It should also be noted that treatment is dose-dependent and when these optical appliances suffer breakage, which is a normal occurrence for children, time taken for repairs or replacement spectacles can be an issue.
It goes without saying that poorly fitted spectacles will be less comfortable to the child and will most certainly lead to reduced compliance.
For optimal performance a well-fitting frame with as close a vertex distance as possible (without touching the lashes) to maximise field of view through the optic zone is essential. All manufacturers recommend a 10mm BVD or less.
The frame needs to be deep enough that the child cannot look over the top or under the bottom rim (without resting on cheeks) and should also fit the manufacturer’s recommended A and B measurement criteria.
As with all spectacle lenses to avoid unwanted aberrational astigmatism the centre of rotation condition must be satisfied (figure 3), and vertical centration matched to pantoscopic tilt (figure 4).
Figure 3: The centre of rotation condition Figure 4: Measuring Pantoscopic angle
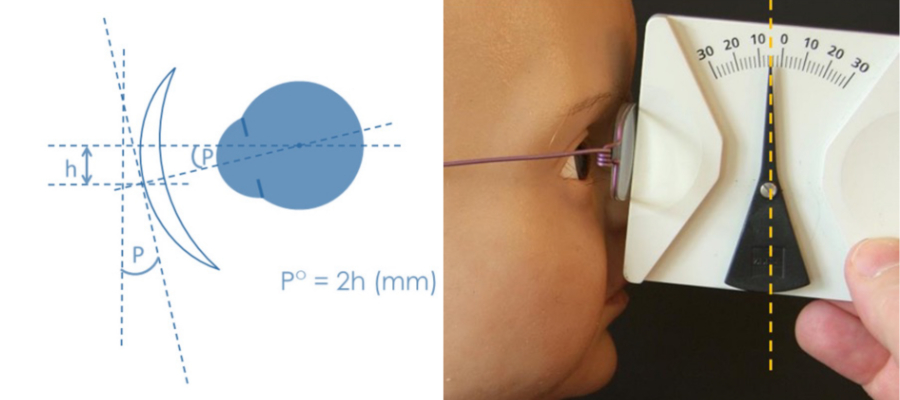
Normally vertical centres are dropped 1mm for every 2º of tilt, however the need to look through the centre of optic zone of the lens when the eye is in the primary position means that it is essential to place the vertical centres on pupil centre (+/-1mm), which in turn means the frame must fit with a pantoscopic angle of 0º (+/-2º).
Failure to heed these manufacturer’s instructions will result in unnecessary remakes, retests and refunds in optical practice.
Communicating myopia risks to patients/parents should be conducted at the earliest opportunity as myopia has a faster progression in younger age groups.24
Young adults especially those undertaking higher education should not be overlooked as adult-onset myopia accounts for at least one third of all myopes in western populations and myopic progression can continue into early adulthood and can average 1.00D between the ages of 20-30 years.25
Contact lens options
Coopervision MiSight 1-day
MiSight 1-day is a dual-focus soft daily disposable contact lens design, which has the longest running research providing supporting data over six years. Beginning as a three-year multi-centre double blind RCT (control group wearing Proclear 1-day lenses) achieving results in refraction of 59% less myopic progression and 52% less mean change in axial length.8
Children aged eight to 12 years, average wearing times 13 hours over 6.5 days per week.
For the second part of this study over the following three years the control group switched to the MiSight 1 day lens forming T3 group receiving three years of the MiSight treatment lens, and the T6 group which had six years of the treatment lens.
T3 group over six years progressed by an average of -1.55D axial length by an average of 0.81mm.
T6 group over six years progressed by an average of -0.92D with 23% of eyes showing no clinically meaningful change in SER (-0.25D or less) over the six years, axial length progressed by an average of 0.49mm.
Key points: starting treatment at an earlier age offers a greater effect but beneficial effects were still found even when treatment is started at a later age. The study concluded that eye growth in T3 over the final three years after switching to the treatment Misight lens was slowed by 71%.
Visioneering Technologies NaturalVue Multifocal 1 day
This simultaneous vision centre distance, extended depth of focus lens has supporting evidence from Cooper et al,26 a retrospective cases series analysis that provided real world data, showing for 75% of children myopic progression stopped.
A total of 90.6% of children showed a 70% decrease or greater in myopic progression, and 6.25% showed refraction had regressed.
The authors themselves acknowledge this research method lacked the scrutiny of an RCT as there was no control group, and a lack of full baseline data. An RCT known as Protect is currently being undertaken by Visioneering Technologies, which expects to publish one-year follow up data towards the end of 2023.27
Mark’ennovy Mylo
Partnered with the Brien Holden Vision Institute (BHVI) using the patented BHVI extended depth of focus (EDOF) technology to slow myopic progression.
There is an extensive range of powers available -0.25D to -15.00D (0.25D steps) with diameters from 13.50mm to 15.50mm (0.5mm steps), which is also available in toric form with cylinders from -0.75DC to -8.00DC (0.25DC steps) in a silicon hydrogel material.
Results from an efficacy study by Sergio Diaz was reported recently in Optician, this two-year study involving children aged six to 13 years found axial length data 0.37mm vs 0.66mm treatment lens to control with efficacy of 45%.28
Safilens Delivery Tyro
This is a daily disposable contact lens that delivers tyrosine a semi-essential amino acid designed to ‘normalise ocular development’ as it metabolises to dopamine, supporting evidence for this lens is expected to be published at the end of the year once peer review has been completed.29
This lens utilises a different mechanism to slow myopic progression, which provides ECPs with an exciting new addition for myopia management.
Safety in Contact lens Wear
Safety is the most important consideration for ECPs when prescribing contact lens wear for children.
Woods et al,30 a prospective six-year study following MiSight study participants, found no serious adverse incidents (microbial keratitis) and that contact lens wear was successful confirming that children as young as eight years of age can successfully wear daily disposable contact lenses.
MiSight 1 day contact lenses were found to be a safe method for myopia management with minimal impact on ocular physiology.
Bullimore et al31 found the incidence of microbial keratitis in soft contact lens wear (2.7 per 10,000 patient years) in children was no higher than in adults and that the incidence of corneal infiltrative events (CIEs) was notably lower, but emphasised the importance of consistent patient education on wearing and caring for contact lenses and highlighting modifiable risk factors like swimming or sleeping in lenses.
Pharmacological interventions
Licensed low dose atropine appears will take more time to become available in the UK as the approval process takes time and there are still questions surrounding exactly which dose is best.29
Results of the Champ study recently published show that low dose atropine 0.01% may provide a safe and effective treatment for myopia progression.32
A recent review by Jawaid et al33 concluded that atropine was safe and effective as a treatment option for myopia with concentrations of 0.025% and 0.05% but 0.01% in East Asian populations did not slow axial elongation.
Combination treatments are often prescribed in medicine to improve effectiveness and would seem a logical approach to myopia management interestingly earlier this year Nucci et al31 published results from a one-year non-randomised study comparing efficacy of atropine 0.01%, DIMS (Hoya Miyosmart) and combined DIMS and atropine.
Results found relative to the control group the following percentage reduction in myopic progression; atropine 0.01% group 57% in SER and 62% in axial length; DIMS 57% in SER and 57% in axial length; combined atropine +DIMS group 70% in SER and 77% in axial length.
Combined orthokeratology + atropine (0.01%-1%)32 also found a synergistic effect of the combination treatment although, the combined treatment of atropine 0.01% and a soft multifocal contact lens did not produce a better myopia control effect.33
Orthokeratology
Orthokeratology has been used for many years as a method for myopia correction enabling wearers freedom from daytime lens wear, meaning for those active patients that take part in sporting activities especially swimming as no contact lenses are worn during the day, and environmental dry eye issues are less of a concern.
Orthokeratology is also an effective treatment for myopia slowing its progression from 32% to 63% compared to single vision spectacles.34
These lenses do require exact fitting and more monitoring also, wear should be continued until after age 14 years to avoid rebound and rapid axial length increase35 although in the authors opinion if this method of myopia management is successful acknowledging the benefits orthokeratology offers it is unlikely the patient will discontinue wear.
Time outdoors
This is free. Advice regarding maximising outdoor time should always be part of myopia discussion as this improves mental health36 as well as affording a protective element against myopia onset,37 40 minutes per school day of outdoor time can reduce the incidence of myopia.34
Conclusion
ECPs are now expected to stay abreast of a rapidly changing marketplace and research situation with regards to myopia management. It is clear that no intervention, or combination of interventions can halt myopia progression completely, or indeed prevent it occurring in the first place.
Nevertheless, there are now a multitude of safe and effective spectacle and contact lens treatment options to slow the progression of myopia to between half and two-thirds of its typical expected rate through the creation of relative peripheral myopic defocus using products that are licenced/approved for this purpose.
With licenced products now offering increased prescription ranges, a wide range of materials, and a variety of treatment methods it should only rarely be necessary for patients to be treated off licence using products with lower rates of efficacy.
As was discussed by Richard Edwards (Optician, July 27, 2023) it is without doubt the legal and ethical responsibility of ECPs to inform patients/parents of the known typical progression of myopia, the risks of sight loss later in life, and the importance of time outdoors in limiting progression.
ECPs also have a duty to inform patients of the availability of evidence based treatments in the form of spectacles and contact lenses. It is not the ECP’s role to prejudge the ability of the patient to afford the treatment merely to provide information so the family can make an informed choice and provide valid consent to whatever option is chosen.
Patients/parents must also be made aware that not all patients will respond as expected to an intervention and this may take time to become apparent and it may be necessary to try an alternative treatment option.
As with all spectacles and contact lenses there are a number of competing options and often there is a compromise to be reached, where for example a less effective product is selected because it is offered in a more suitable material, or at a price that is more affordable.
Additionally, opticians have preferred suppliers that they would rather do business with for commercial reasons.
It is, however, likely that the evidence will suggest that certain products have a greater treatment effect in different age groups, and in the future this may sway the choice of treatment, which may change according to the age of the child or the degree of myopia.
That said, just as many adult patients who wear varifcoal spectacle lenses prefer a specific design and find adaption to a different product design difficult, there may be a similar effect with changing myopia management designs even if the research suggests a greater treatment effect.
Finally, all discussions, advice, and recommendations should be fully documented within the patient record and as usual the ECP must be careful to always act in the best interests of the patient, to balance commercial considerations with the need to always provide informed choice and gain valid consent based on staying up to date with the latest research.
- Peter Black MBA FBDO FEAOO PGCAP FHEA is a registered dispensing optician, award-winning CPD author and presenter, past president of the Association of British Dispensing Opticians (ABDO), and course lead for the accelerated blended learning BSc (Hons) Ophthalmic Dispensing programme at the University of Central Lancashire, Preston.
- Tina Arbon Black GOC is an experienced CPD author and presenter and is one of the clinical editors for Optician Magazine as well as a director of OrbitaBlack Limited, an approved CPD provider that works with customers to produce CPD programmes. She is an ABDO College tutor, theory script marker and former ABDO practical examiner and frequently authors and delivers CPD for ABDO.
References
- General Optical Council, “3 Obtain Valid Consent,” in Standards of Practice for Optometrists and Dispensing Opticians, London, General Optical Council, 2016, p. 8.
- Moore M, Flitcroft DI, and Loughman J, “Prescribing patterns of myopia control contact lenses among optometrists in Ireland,” Ophthalmic and Physiological Optics, vol. 43, no. 3, pp. 377-378, 2023.
- General Optical council, “Obtain valid consent,” in Standards of Practice for Optometrists and Dispensing Opticians, London, General Optical Council, 2016, p. 3.
- TS, Regulation and UK Optometry, London: World Scientific Publishing CO. Pte. Ltd, 2023, pp. 279-282.
- General Optical Council, “Keep your knowledge and skills up to date,” in Standards of Practice for Optometrists and Dispensing Opticians, London, GOC, 2016, p. 10.
- Wolffsohn JS, Whayeb Y, Logan NS, Weng R and IMI Ambassador Group, “IMI-Global Trends in Myopia Management Attitudes and Strategies in clinical Practie-2022 update,” Investigative Ophthalmology & Visual Science, vol. 64, no. 6, 2023.
- Flitcroft DI, M He, JB Jonas, M Jong, K Naidoo, K Ohno-Matsui, J Rahi, S Resnikoff, S Vitale and L Yannuzzi, “IMI-Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies,” Investigative Ophthalmology & Visual Science, vol. 60, no. 3, 2019.
- P Chamberlain , S Peixotopde-Matos, N Logan, D Jones and G Young , “a 3-year Randomised Clinical Trial of MiSight Lenses for Myopia control,” Journal of the American Academy of Optometry, vol. 96, no. 8, pp. 556-567, 2019.
- CS Lam, WC Tang, DY Tse, RP Lee, RK Chun, K Hasegawa, H Qi, T Hatanaka and CH To, “Defocus Incorporated Muliptle Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial,” vol. 104, pp. 363-368, 2019.
- JS Wolffsohn, PS Kollbaum, DA Berntsen, DA Atchison, A Benavente, A Bradley, H Buckhurst, M Collins, T Fujikado, T Hiraoka, M Hirota, D Jones, NS Logan, L Lundstrom, T Hidemasa, SA Read and K Naidoo, “IMI - Clinical Myopia Control Trials and Instrumentation Report,” Investigative Ophthalmology & Visual Science, vol. 60, no. 3, pp. 132-160, 2019.
- BA Holden, TR Fricke, DA Wilson, M Jong, KS Naidoo, P Sankaridurg, TY Wong, TJ Naduvilath and S Resnikoff, “Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050,” Ophthalmology, vol. 123, no. 5, pp. 1036-1042, May 2016.
- MA Bullimore and N Brennan, “Myopia Control: Why Each Diopter Matters,” Optometry and Vision Science, May 2019.
- DI Flitcroft, “The Complex Interactions of Retinal, Optical and Environmental Factors in Myopia Aetiology,” Retinal and Eye Research, vol. 31, no. 6, pp. 622-660, 2012.
- The College of Optometrists, “Myopia management guidance for optometrists,” 2022. [Online]. Available: https://www.college-optometrists.org/category-landing-pages/clinical-topics/myopia/myopia-management-%E2%80%93-guidance-for-optometrists.
- The Association of British Dispesning Opticians, “Myopia management overview,” [Online]. Available: https://www.abdo.org.uk/dashboard/clinical-hub/focuson-2/myopia-management-overview/introduction/.
- LA Jones, LT Sinnott, DO Mutti, GL Mitchell, ML Moeschberger and K Zadnik, “Parental History of Myopia, Sports and Outdoor Activities, and future Myopia,” Investigative Ophthalmology & Visual Science, vol. 48, no. 8, pp. 3524-3532, 2007.
- Z. Zhu, Y Chen, Z Tan, R Xiong, MB McGuinness and A Muller, “Inerventions recommended for myopia prevention and control among children and adolescents in China: A systematic review,” British Journal of Ophthalmology, vol. 107, no. 2, 2021.
- AR Rudnicka, VV Kapetanakis, AK Wathern, DG Cook and C G Owen, “Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention,” British Journal of Ophhalmology, vol. 100, pp. 882-890, 2015.
- L Donovan, P Sankaridurg, A Ho, T Naduvailath, EL Smith and BA Holden, “Myopia Progression Rates inUrban Children Wearing Single-Vision Spectacles,” Optometry and Vision Science, vol. 89, no. 1, pp. 27-32, 2012.
- K. Zadnik, LT Sinnott , SA Cotter and et al, “Prediction of Juvenile-Onset Myopia,” JAMMA Ophthalmology, vol. 133, no. 6, pp. 683-689, 2015.
- IG Morgan, P Wu, LA Ostrin , WL Tideman, JC Yam and et al, “IMI Risk Factors for Myopia,” Investigative Ophthalmology & Visual Science, vol. 62, no. 3, 2021.
- R Leighton, K Breslin, P Richardson, L Doyle, S McCullough and K. Saunders, “Relative peripheral hyperopia leads to greater short-term axial length growth in white children with myopia,” Ophthalmic and Physiological Optics, vol. 43, no. 5, pp. 985-996, 2023.
- Y Gao, EW Lim, A Yang, B Drobe and M Bullimore, “The Impact of spectacle lenses for myopia control on visual functions,” Ophthalmic & Physiological optics, vol. 41, no. 6, pp. 1320-1331, 2021.
- D Tricard, S Marrillet, P Ingrand, MA Bullimore, RR Bourne and N Leveziel, “Progression of myopia in children and teenagers: a nationwide longitudinal study,” British Journal of Ophthalmology, vol. 106, pp. 1104-1109, 2022.
- MA Bullimore, SS Lee, KL Schmid, J Rozema, N Leveziel, E Mallen, N Jacobsen, R Iribarren, PK Verkicharla, JR Polling and P Chamberlain, “IMI-Onset and Progression of Myopia in Young Adults,” Investigative Ophthalmology & visual Science, vol. 64, no. 3, 2023.
- J Cooper, B O’Connor, R Watanabe , F Randall, S. Berger, N Eisenberg and S Dillehay, “Case series analysis of myopic progression control with a unique extended depth of focus multifocal contact lens,” Eye & contact Lens, vol. 44, no. 5, pp. e16-e24, 2018.
- V Technologies, “Visioneering Achieves 50% Enrollment Milestone in its PROTECT International Clinical Study for Myopia Progression Control,” 2022. [Online]. Available: https://vtivision.com/wp-content/uploads/2022/07/ASX-Release-PROTECT-50-Enrollment-FINAL-VTI-IR-ASX62-1-1.pdf. [Accessed 25th September 2023].
- J Dickson, “Expanding Options for myopia,” Optician, vol. 268, pp. 29-31, 2023.
- Optician, “Safilens: Dopamine lens Design,” May 2022. [Online]. Available: https://www.opticianonline.net/content/news/safilens-dopamine-design/.
- J Woods, D Jones, L Jones, S Jones, C Hunt, P Chamberlain and J McNally, “Ocular health of children wearing dispasable contact lenses over a 6-year period,” Contact Lens and Anterior Eye, vol. 44, no. 4, 2021.
- MA Bullimore and K Richdale, “Incidence of corneal adverse events in children wearing soft contact lenses,” Eye & Contact Lens, vol. 49, no. 5, pp. 204-211, 2023.
- Optician, “Atropine and the Goldilocks Problem,” July 2023. [Online]. Available: https://www.opticianonline.net/content/features/atropine-and-the-goldilocksproblem#:~:text=Atropine’s%20Goldilocks%20problem&text=Currently%2C%20that%20leaves%20us%20with,be%20somewhere%20in%20the%20middle..
- I Jawaid, K Saunders, CJ Hammond, A Dahlmann-Noor and MA Bullimore, “Low Concentration atropine and myopia: a narrative review of the evidence for United Kingdom based practitioners,” Eye, 2023.
- M He, F Xiang, Y Zeng, J Mai, Q Chen, J Zhang, W Smith, K Rose and I Morgan, “Effect of Time Spent Outdoors at School on the Development of Myopia Among Children in China,” JAMMA Network, vol. 314, no. 11, pp. 1142-1148, 2015.
- S Vik, J Seidel and DA Marshall, “Breaking the 80:20 rule in health research using large administrative data sets,” Sage Journals, vol. 29, no. 2, 2023.
- K Zadnik, E Schulman, I Flitcroft, J Fogt, C Blumenfeld, T Fong, E Lang, H Hemmati, S Chandler and CHAMP GROUP, “Efficacy and Safety of 0.01% and 0.02% atropine for the treatmnt of paediatric myopia progression over 3 years,” JAMMA Ophthalmology, 01 June 2023.
- P Nucci, A Lembo, I Schiavetti, R Shah, DF Edgar and BJ Evans , “A comparison of myopia control in european children and adolescents with defocus incorporated multiple segmnts (DIMS) speectacles, atropine, and combined DIMS/atropine,” PLoS ONE, vol. 18, no. 2, 2023.
- H Tsai, J Wang, H Huang, T Chen and C Chiu, “Efficacy of atropine, orthokeratology, and combined atropine with orthkeratology for childhod myopia: A systematic review and network meta-analysis,” Journal of the Formosan Medical Association, vol. 121, no. 12, pp. 2490-2500, 2022.
- J Jones, D Mutti, L Jones-Jordan and J Walline , “Effect of combining 0.01% atropine with soft multifocal contat lenses on myopia preogression in children,” Optometry and Vision Science, vol. 99, no. 1, pp. 434-442, 2022.
- H Takahiro, “Myopia Control with Orthokeratology: A Review,” Eye & Contact Lens, vol. 48, no. 3, pp. 100-104, 2022.
- P Cho and SW Cheung, “Discontinuation of orthokeratology on eyeball elongation (DOEE),” Cantact Lens and Anterior eye, vol. 40, pp. 82-87, 2017.
- Y Zhang, S Mavoa, J Zhao, D Raphael and M Smith, “The association between Green Space nd Adolescents’ Mental Well-being: A systematic Review,” International Journal of Environmental Research and Public Health, vol. 17, 2020.
- S Xiong, P Sankaridurg, T Naduvilath, J Zang, H Zou, J Zhu, M Ly, X He and X Xu, “Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review,” ACTA Ophthalmologica, vol. 95, no. 6, pp. 551-556, 2017.
