The Tear Film and Ocular Surface Society (TFOS) recently released a series of 10 reports based on the findings from the ‘A Lifestyle Epidemic: Ocular Surface Disease’ workshop, featuring contributions from 158 authors across 38 countries. These reports comprehensively review the impact of various lifestyles and societal factors on the ocular surface.
While the full reports are available for download on the TFOS website,1 this article offers a distilled, evidence-based summary of key clinical insights for eye care professionals (ECPs) with a focus on dry eye and ocular surface disease.
Nutrition
The nutrition report2 explores the influence of micro- and macronutrients on ocular health. Beyond vitamins, it delves into liquid intake, supplementation, and nutrition-associated diseases like diabetes mellitus and gastrointestinal disorders. Noteworthy findings include the correlation between vitamin deficiencies (A, C, B12, and D) and dry eye. The report emphasises that while most Western diets generally meet vitamin A and C requirements, specific groups, such as vegans and vegetarians, may be prone to deficiencies in B12. Vitamin D is mainly produced in the skin via sunlight, UVB, hence a deficiency can occur during the winter season due to the lack of sun and daylight.
Furthermore, the discussion around omega-3 fatty acids highlights their potential as a beneficial supplement for dry eye patients, with a focus on the importance of a balanced omega-3 to omega-6 ratio. Although the intake of omega-3 fatty acids through diet may be sufficient for some, a typical Western diet contains too many omega-6 versus omega-3 fatty acids. Dry eye is frequently observed in conjunction with specific nutrition-related health conditions, such as diabetes mellitus, and gastrointestinal diseases like irritable bowel syndrome, Crohn’s disease, and ulcerative colitis.
Contrary to popular belief, a recent extensive population study indicated that adhering to the Mediterranean diet does not appear to decrease the likelihood of developing dry eye.3 Nonetheless, certain studies have suggested a potential protective effect associated with plant-based nutrients and spices. For example, curcumin in turmeric is an antioxidant and known for its anti-inflammatory properties.
Digital environment
Digital eye strain is the development or exacerbation of recurrent ocular symptoms and/or signs, specifically related to viewing screens of digital devices.4 According to the literature, the average prevalence is 70%, ranging between 32% and 97% globally. Most common symptoms include eye strain and dry eye, as well as headaches, back and neck pain, and fatigue.
Although it is well documented that incorrect viewing distances, poor seating posture and poor lighting are root causes of digital eye strain, uncorrected vision problems including refractive error and binocular vision play a significant role. Digital eye strain affects productivity, due to delays in digital task completion, increase in the number of errors made, or cause the person to pause more often. The chronic nature of the condition affects quality of life and this has been exacerbated by the extra time spent in the digital environment during the pandemic and the resulting changes in working practices.
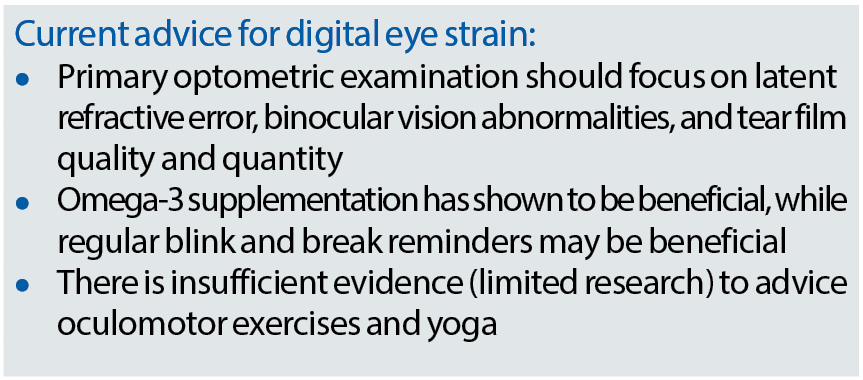
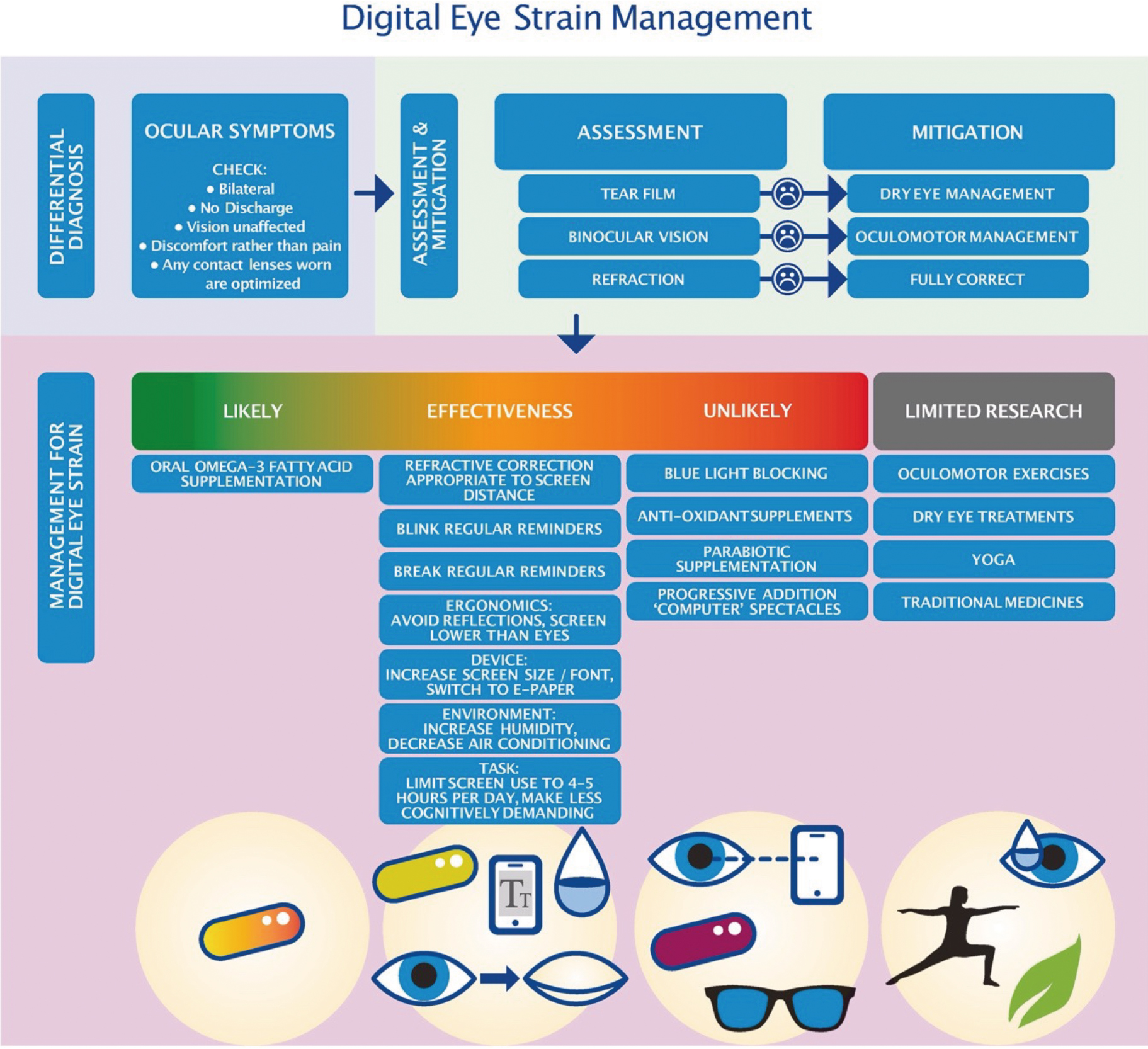
The report provides ECPs with an overview of the diagnosis and management options for digital eye strain, based on the current evidence (see figure 1). Once ocular symptoms including bilateral discomfort without visual fluctuations or ocular discharge have been identified, a standard assessment should include examination of the tear film and ocular surface, binocular vision and refraction. An up-to-date refraction at distance, intermediate and near distances is required, as well as management of oculomotor problems and dry eye disease.
If symptomology still persists while using digital devices, oral omega-3 fatty acid supplementation is most beneficial for the patient. Regular blink and break reminders, probiotic supplements, eyelid warming, increasing humidity, and using alternative reading formats (e-paper) all have shown some favourable effect and could be considered. There is currently no evidence that blue light blocking lenses, anti-oxidant or parabiotic supplementation, or progressive addition computer spectacles work for those who struggle with digital eye strain.
Figure 1: Schematic overview of the evidence-based management of digital eye strain4
Environmental conditions
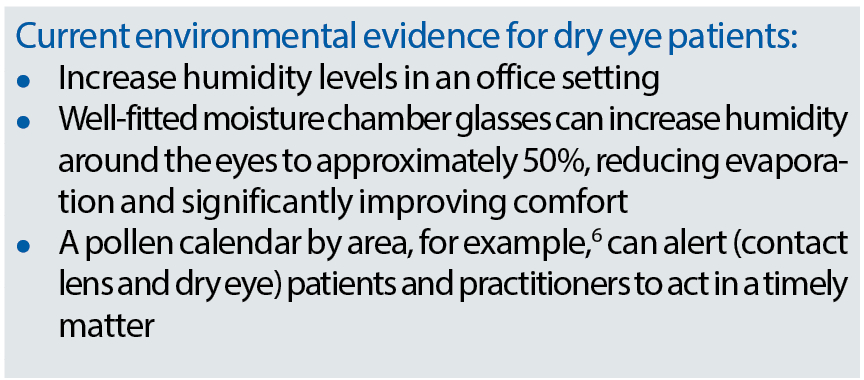
This report explored how environmental factors, including pollutants, allergens and climate conditions such as sunlight, temperature and humidity, affect the ocular surface.5 Both low and high temperatures have been associated with dry eyes. In a controlled study environment, a room temperature of 25°C showed more tear evaporation compared to 5°C. However, this triggered a protective mechanism of the eye and caused a significant increase in the non-invasive break up time and lipid layer thickness.
Population-based studies have reported more dry eye with higher climate temperatures. Higher humidity (30 to 40%) has shown to reduce dry eye symptoms, compared to humidity levels in an average office setting (20 to 30%). It is well documented that higher humidity levels will increase the tear break up time and lipid layer thickness.
Allergic conjunctivitis due to pollen and allergens is often seasonal. For example, allergies for trees like birch and hazel are more common during spring, while allergies for meadow grasses may extend into the summer. This is in contrast to sensitivity towards pet dander and dust mites, which can occur throughout the year.
Air quality, or air pollution, has been studied widely, but the only gas-like pollution significantly linked to ocular surface disease so far is nitrogen dioxide. People living among heavy traffic have therefore more chance to complain of ocular irritation and show a reduced tear break up time. There is strong evidence that particulate matter (PM10) is not associated with dry eye diagnosis or symptoms.
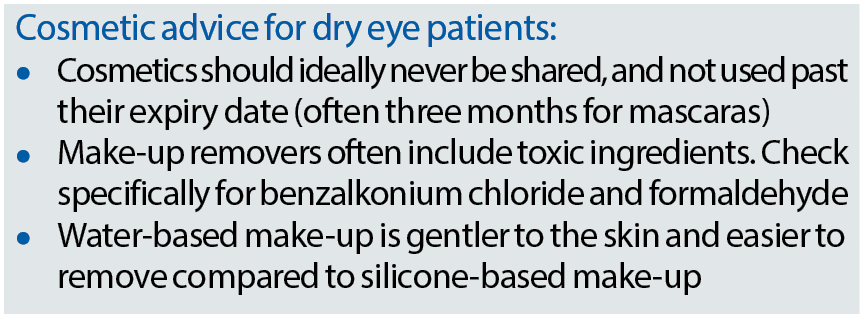
Cosmetics
ECPs should not underestimate the impact of cosmetics on the ocular surface.7 Certain ingredients in make-up, removers, anti-aging creams, eyelash extensions, but also treatments like chemical peels, micro-needling, eyelid tattooing, and eyelash curling/dying/tinting may all present potential adverse effects to the ocular surface and adnexa. It is widely known that benzalkonium chloride, an antiseptic or preservative, can cause significant ocular irritation.
Similarly, formaldehyde-releasing compounds used as a preservative in make-up and make-up cleansers, are toxic to corneal epithelial cells, conjunctiva and meibomian glands in quantities that are 2,000 times lower than the European Union limits for cosmetics.8 Certain ingredients used in skin treatments can also cause irritation to the eyes. Salicylic acid, which is used to treat conditions such as acne, dandruff and psoriasis, as well as tea tree oil for Demodex are harmful to the ocular surface in higher concentrations.
Sharing cosmetics can be a source of bacteria, viruses, and Demodex transmission. This depends on the frequency of use, the age of the product, and the number of users. Ideally, cosmetics should never be shared. Over time, the repeated use of a single cosmetic product can introduce microbes into the container. It was found that following three months of use, microbial presence was found in over one-third of tested mascaras that were given to participants for their own use.9 Another study collected used mascaras and reported that 79% tested positive for Staphylococcus aureus and 13% were contaminated with Pseudomonasaeruginosa.10
Temporary complications following botulinum toxin injections, such as blepharoptosis, reduced lacrimal function, incomplete closure of the eyelids, ectropion or diplopia, are less common in case it is administered by a trained medical professional. Reports of adverse reactions to eyelash extensions include allergic contact dermatitis, eyelash loss, eyelash base calcification, blepharitis, conjunctivitis, corneal abrasions and keratitis. The patient is more at risk of dry eye-related complications if the health of the eyelids and lashes are not considered before application.
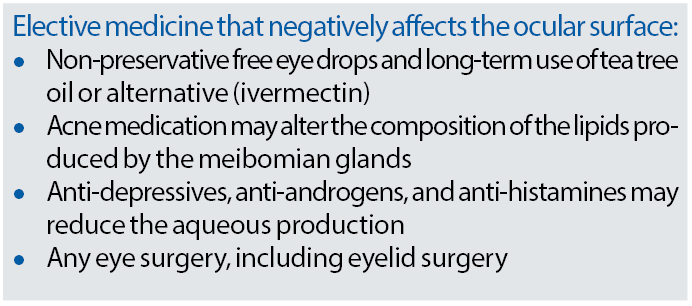
Elective medications
The term ‘elective’ relates to medications and procedures chosen voluntarily or with a lesser level of urgency, excluding those deemed medically necessary. Patients may opt for elective medications or procedures for medical or cosmetic reasons, aiming to positively impact their lifestyle and enhance their overall quality of life. The report11 comprehensively examines the impact on ocular surface health resulting from the use of the most commonly prescribed (peri-) ocular topical and systemic medications. It reveals that half of these medications have been linked to the occurrence of dry eyes.
Preservatives play a pivotal role in the immunologic response, triggering allergic, chemical or toxic reactions that lead to increased inflammation. The response to preservative toxicity from eyedrops may manifest in the lipid layer of the tear film, potentially reducing aqueous secretion or adversely affecting conjunctival goblet cells, conjunctival and corneal epithelia, as well as the eyelids, including the skin and the meibomian glands. Benzalkonium chloride has been identified as a substance capable of increasing tear film osmolarity and inducing a pro-inflammatory response. The well-documented solution to mitigate these issues involves transitioning to preservative-free eye drops, resulting in a significant reduction of both subjective and objective symptoms and signs.
Any form of ocular surgery escalates the risk of developing dry eye. Procedures such as cataract, glaucoma or laser eye surgery are associated with a notable two to five times increase in the occurrence of dry eye symptoms and signs.12 While a majority of patients experience a significant reduction in dry eye symptoms three months post-surgery, some individuals are left grappling with a severe decline in their quality of life due to persistent dry eyes. A proactive approach, including a specialised dry eye assessment before these procedures, has shown promise in enhancing post-surgical outcomes. Additionally, the preventive use of preservative-free artificial tears before surgery offers protection against surgery-induced dry eyes.
Eyelid surgery introduces its own set of challenges, potentially causing an incomplete blink. This not only affects the evaporation rate and results in inferior corneal epithelial cell damage but also diminishes the release of meibum from the meibomian glands. This reduction occurs due to a lesser ability to squeeze the lids during blinking. Patients suffering from obstructive sleep apnoea and utilising a poorly fitted face or CPAP mask report significantly more dry eyes.
Moreover, floppy eyelid syndrome is more prevalent in individuals with sleep apnoea, causing the upper eyelids to evert with upward traction or spontaneously during sleep. The report also explores the use of heat masks in managing dry eye. When prescribing heat therapy, selecting an appropriate mask with a sufficient heat profile and correct heat transmission, clear usage instructions (including expiry date), and patient compliance are crucial considerations.
Lifestyle challenges
The most recent findings highlighted in this report13 indicate that there is no conclusive evidence linking smoking to an increased prevalence of dry eyes. While smoking does result in poorer tear film quality by reducing tear break up time, heavy smokers may exhibit a decrease in corneal sensitivity, offering a protective effect. Consequently, quitting smoking can paradoxically lead to a reduction in objective dry eye indicators but an increase in subjective dry eye symptoms.
The report further underscores the strong association between poor sleeping patterns and dry eye. Disruptions in sleep, including diminished duration, increased latency, compromised quality, and efficiency, significantly contribute to the onset of sleep disorders and daytime dysfunction. This establishes a cyclic relationship, as sleep deprivation has been demonstrated to decrease tear production and induce corneal epithelial injury in mouse models.
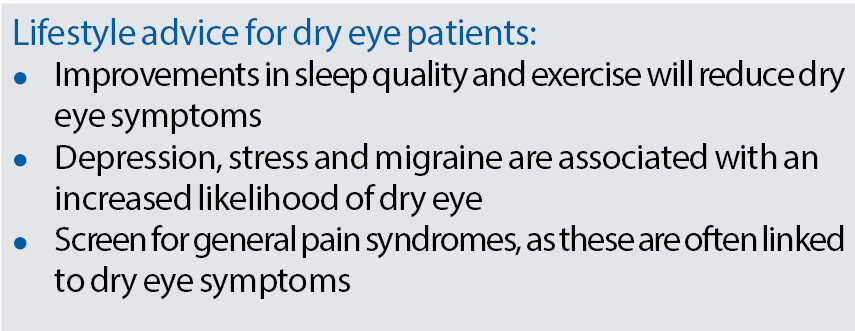
The impact of obesity on dry eye remains less clear. While larger population studies suggest a potential positive effect, associating increased BMI with a reduced risk of dry eye, smaller studies indicate a lower tear break-up time and heightened variations in meibomian gland tortuosity in individuals with obesity compared to those without. The repercussions of weight loss on dry eye are yet to be fully understood.
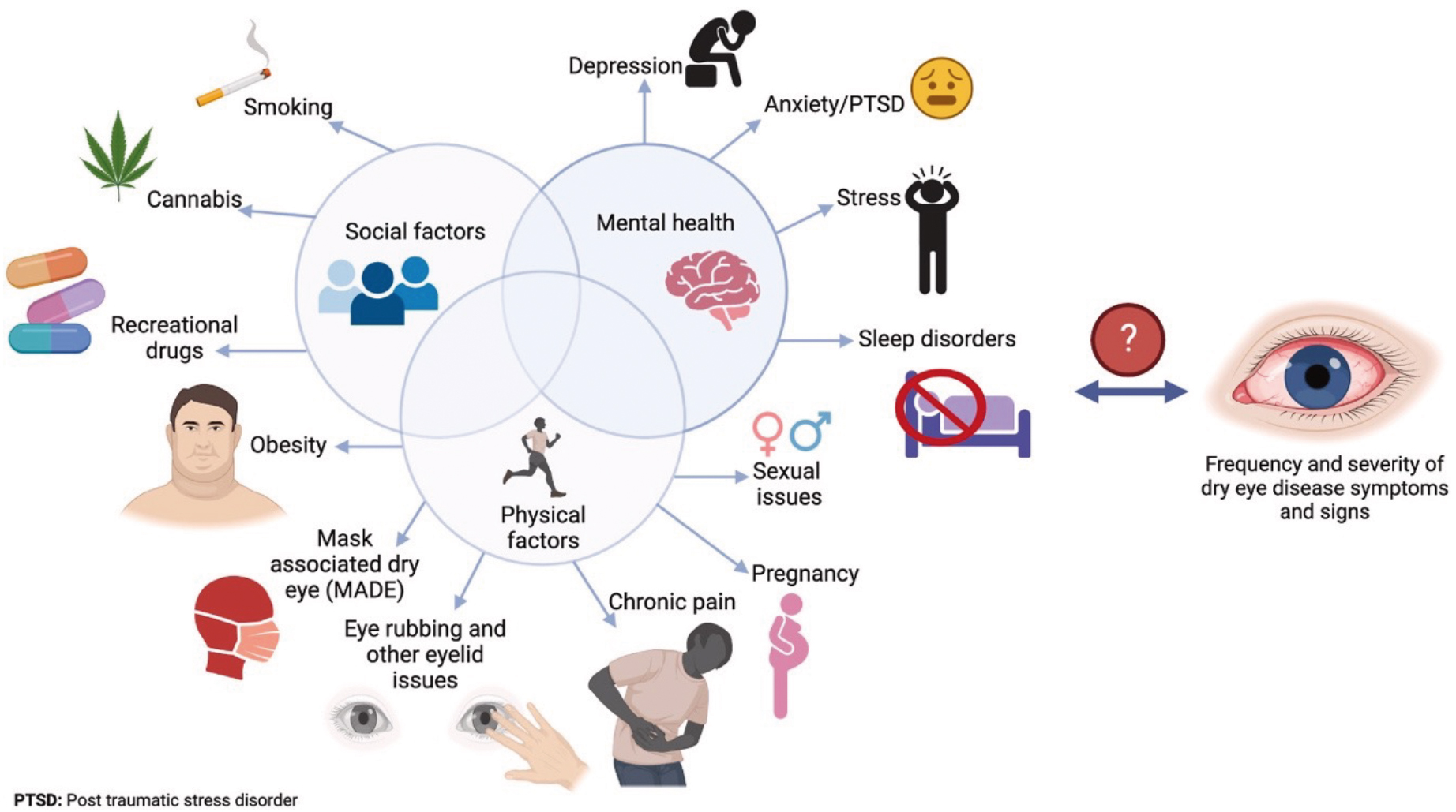
Exercise emerges as a beneficial factor in improving dry eye symptoms. Conversely, dry eye conditions can contribute to stress and depression, and vice versa. Additionally, migraines and back pain are both individually linked to a 1.6x increased likelihood of experiencing dry eye symptoms. These interconnections underscore the intricate web of factors influencing ocular health and symptoms and the need for a holistic approach in managing dry eye conditions (see figure 2).
Figure 2: Lifestyle decisions related to the severity of symptoms and signs of dry eye and other ocular surface
diseases13
Contact lenses
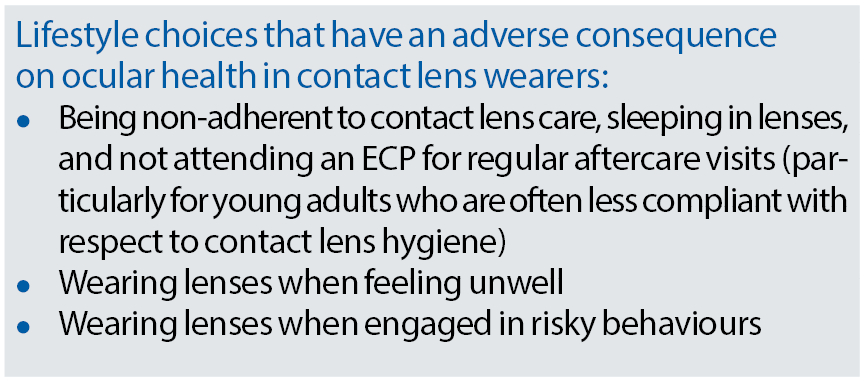
This report delves into the impact of contact lens safety and performance on the ocular surface, as well as how lifestyle choices influence contact lens efficacy.14 While summarising the entire report is impractical, key highlights are described below.
The primary risk factor for microbial keratitis is overnight lens wear. Additional risk factors include topping off contact lens solutions, infrequent cleaning or replacement of the lens case, and contamination with tap water. Daily disposables stand out as the most convenient contact lenses, exhibiting the highest adherence to replacement schedules and demonstrating the lowest rates of complications.
Regarding lifestyle choices, it is established that increased age and prolonged contact lens wear negatively impact the ocular surface and ongoing contact lens success. Systemic diseases such as diabetes mellitus and thyroid conditions, along with medications for these ailments, can complicate successful contact lens wear. Evidence suggests that individuals with ocular allergies can safely wear lenses, potentially offering protection through a novel treatment option involving anti-allergy, drug-delivering contact lenses.
Managing contact lens wearers with viral upper respiratory tract infections remains less clear, with recent reviews presenting inconclusive evidence on the risk of microbial keratitis in unwell wearers. However, a clear correlation exists between being unwell and an increased incidence of corneal inflammatory events associated with contact lens wear.
Higher risk-taking personalities among lens wearers have been associated with poorer compliance. Interestingly, this appears to be a better predictor of compliance than age, gender and practitioner perception. The use of accessory devices like tweezers, plungers and suction cups somewhat increase the risk of complications. While washing these supplementary devices with soap and water and replacing them frequently are recommended, data on the optimal frequency is lacking.
Tobacco, cannabis and vaping can affect tear film quality in contact lens wearers. Smokers experience increased tear evaporation, altered lipid layers, and a 3x higher risk of developing microbial keratitis, along with a 1.5 to 3x greater risk of corneal infiltrative events compared to non-smoking contact lens wearers. The use of cosmetics and cleansers in conjunction with contact lenses also raises the likelihood of complications, particularly due to the toxic ingredients designed to prevent microbial growth, as discussed earlier.
Summary
In conclusion, the 10 TFOS Lifestyle Workshop reports have meticulously outlined the direct and indirect effects of everyday lifestyle choices and challenges on ocular surface health, providing substantial evidence.
While seven of the articles have been briefly summarised here, a more comprehensive overview of each TFOS report has been commissioned by Optician and is expected in 2024.
- Dr Byki Huntjens: Optometrist, contact lens and dry eye educator and researcher, and TFOS author
- Dr Jelle Vehof: Ophthalmologist, epidemiologist, and TFOS ambassador and author
- Dave Block: Contact lens optician, and Professional Education & Development at Alcon
• The content of this article is derived from a presentation delivered by Drs Huntjens and Vehof during an Alcon-sponsored live webinar in the Netherlands on October 3, 2023.
References
- TFOS - Tear Film & ocular surface society [Internet]. [cited 2023 Nov 9]. Available from: http://www.tearfilm.org/
- Markoulli M, Ahmad S, Arcot J, Arita R, Benitez-Del-Castillo J, Caffery B, et al. TFOS Lifestyle: Impact of nutrition on the ocular surface. Ocul Surf. 2023 Jul;29:226–71.
- Magno MS, Moschowits E, Morthen MK, Beining MW, Jansonius NM, Hammond CJ, et al. Greater adherence to a mediterranean diet is associated with lower C-reactive protein (CRP) levels, but not to lower odds of having dry eye disease. Ocul Surf. 2023 Oct 1;30:196–203.
- Wolffsohn JS, Lingham G, Downie LE, Huntjens B, Inomata T, Jivraj S, et al. TFOS Lifestyle: Impact of the digital environment on the ocular surface. Ocul Surf. 2023 Apr;28:213–52.
- Alves M, Asbell P, Dogru M, Giannaccare G, Grau A, Gregory D, et al. TFOS Lifestyle Report: Impact of environmental conditions on the ocular surface. Ocul Surf. 2023 Jul;29:1–52.
- Pollen calendars by area [Internet]. [cited 2023 Nov 9]. Available from: https://www.worcester.ac.uk/about/academic-schools/school-of-science-and-the-environment/science-and-the-environment-research/national-pollen-and-aerobiology-research-unit/pollen-calendar.aspx
- Sullivan DA, da Costa AX, Del Duca E, Doll T, Grupcheva CN, Lazreg S, et al. TFOS Lifestyle: Impact of cosmetics on the ocular surface. Ocul Surf. 2023 Jul;29:77–130.
- Chen X, Sullivan DA, Sullivan AG, Kam WR, Liu Y. Toxicity of cosmetic preservatives on human ocular surface and adnexal cells. Exp Eye Res. 2018 May;170:188–97.
- Pack LD, Wickham MG, Enloe RA, Hill DN. Microbial contamination associated with mascara use. Optometry. 2008 Oct;79(10):587–93.
- Giacomel CB, Dartora G, Dienfethaeler HS, Haas SE. Investigation on the use of expired make-up and microbiological contamination of mascaras. Int J Cosmet Sci. 2013 Aug;35(4):375–80.
- Gomes JAP, Azar DT, Baudouin C, Bitton E, Chen W, Hafezi F, et al. TFOS Lifestyle: Impact of elective medications and procedures on the ocular surface. Ocul Surf. 2023 Jul;29:331–85.
- Vehof J, Snieder H, Jansonius N, Hammond CJ. Prevalence and risk factors of dry eye in 79,866 participants of the population-based Lifelines cohort study in the Netherlands. Ocul Surf. 2021 Jan;19:83–93.
- Galor A, Britten-Jones AC, Feng Y, Ferrari G, Goldblum D, Gupta PK, et al. TFOS Lifestyle: Impact of lifestyle challenges on the ocular surface. Ocul Surf. 2023 Apr;28:262–303.
- Jones L, Efron N, Bandamwar K, Barnett M, Jacobs DS, Jalbert I, et al. TFOS Lifestyle: Impact of contact lenses on the ocular surface. Ocul Surf. 2023 Jul;29:175–219.
