Regulation and Supervision
Poorly fitted children’s spectacles can impact both visual and anatomical facial development1 and for this reason spectacle dispensing to children under 16 years of age is a restricted category within the Opticians Act (1989)2 and can only be undertaken by or under the supervision of registered dispensing opticians, optometrists and ophthalmic medical practitioners.
Professional guidance by the Association of British Dispensing Opticians3 (ABDO) and College of Optometrists also sets out clear guidance for eye care practitioners (ECPs) relating to paediatric dispensing and responsibilities when supervising unregistered staff members and registered optical students.4,5 The patient record should also be updated providing clarity as to the registrant with responsibility and details of what task has been supervised.
As part of supervision the child’s interpupillary distance (PD), fit of the frame including vertex distance, bridge fitting, splay and frontal angles of pads and pantoscopic angle should be checked to ensure the selected frame fits appropriately and does not touch the cheeks or brows. The head width and sides must also be checked, paying attention to the length to bend, length of drop and both inward angle of drop and downward angle of drop.
In the past, the greatest challenge when fitting children with spectacles was overcoming their fear of being different, as spectacles were a stigma resisted by both the parents and the child. Fortunately eyewear has now become a fashion accessory, making children both brand-conscious and style-conscious; and possibly more demanding.1 Parents will often select the best for their child’s health, happiness, and safety; however challenging situations arise when the parent’s, patient’s and practitioner’s choices conflict.
Communication is key
It is vital to remember that the parent/guardian’s anxieties need to be dealt with when dispensing very small children. The ECP is required to be understanding and sympathetic as parents are often upset when their child is prescribed spectacles at any age. Although the child is the most important individual during the dispensing, the parents must be involved in the decision-making process; however, they can often be domineering and may demonstrate negative feelings regarding frame choice and the need for a spectacle correction.
Griffiths6 refers to balancing the interactions between the patient and parents/carers as the ‘duality of the patient’ and that a clear communication strategy is essential with the dispensing optician or optometrist providing guidance regarding a suitable frame fit and if necessary resolving any conflict that can arise due to disagreement on frame choice.
Discussion regarding modality of wear, when spectacles should be worn and risks of non-compliance are topics that should also always be communicated to parents/carers as well as checking the information has been clearly understood, particularly as the critical period for visual development is up to around eight years of age7 although recent evidence supports some improvement is still possible after this period.8
If the child fails to meet full visual potential then this could have implications for career options later in life emphasising the importance of accurately fitting spectacles and patient education. All patient/parent discussions should also be fully detailed in the patient record as this is important for all practitioners that follow and are involved in the patient’s care. Maintaining clear and contemporaneous records is part of the General Optical Council (GOC) Standards of Practice for Optometrists and Dispensing Opticians.9
To communicate effectively with children, use age appropriate language starting conversations by using the child’s first name in a friendly manner with words that are likely to be familiar, also simplifying terms and avoiding technical jargon. Finding out what activities or hobbies the child is interested in can help to improve communication and tailoring information for each individual child can help the child to identify their need for spectacles.
For example, in the case of myopia, advise their vision will be clearer and movies or player numbers on football shirts will appear sharper. For hyperopic children relate the improvement in vision to clarity of the screen when using iPads, laptops, or games. Children are generally fascinated by facts so never assume the child is uninterested or will have heard it all before, particularly when related to themselves (see figure 1).
Figure 1: Communication skills

Actively involve and engage the child by asking direct questions and listening to their concerns. This helps to understand the child’s personality, likes and dislikes regarding colours and styles thereby allowing some independence of choice during frame selection. Communication at the child’s eye level is recommended as we appear to be imposing and formidable, strange giants to youngsters.
The practitioner needs to work quickly and efficiently as children have a short attention span, therefore any administration should be kept to a minimum. It may be advisable to dispense away from the dispensing desk in a quiet area where there are fewer distractions. It is essential to pre-dispense, particularly if cycloplegic drops have been used, which can result in the child becoming irritable due to the stinging sensation, mild photophobia and blurred vision.1
The following facial measurements provide the dispensing optician or optometrist with invaluable facial anthropometric information (see figure 2). Compliance of the child during any examination is essential and there are times when using a ruler may not be a safest option especially for very young children (three to 12 months of age) here experience, patience and good observational skills are critical in order to estimate key fitting dimensions. This does require understanding of both frame and facial measurements and the effects on fit when specific frame measurements are altered.
Figure 2: Facial measurements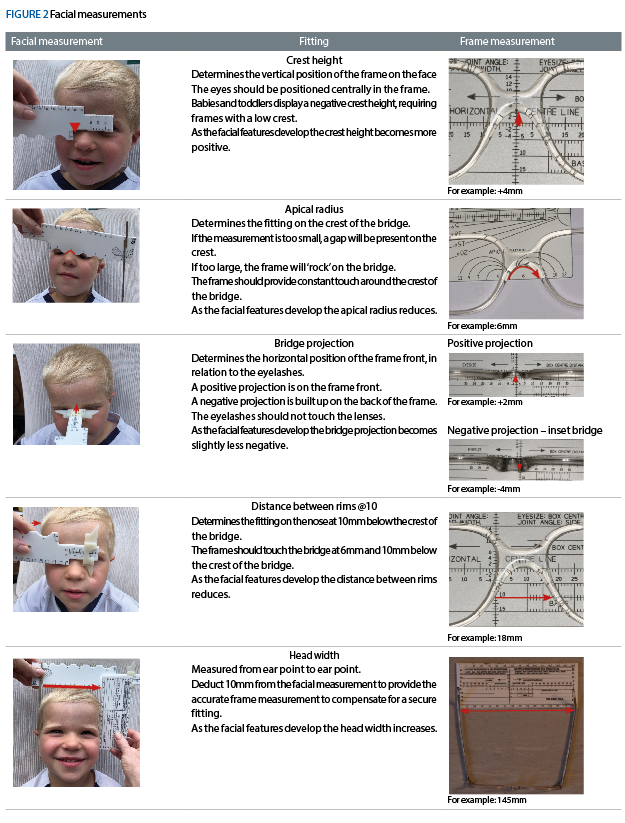
Making measurements matter
As the child’s facial features are constantly developing it is of utmost importance to dispense the most suitable fitting frames thus providing the best comfort as well as promoting compliance of wear. Sit down with the parent/guardian and the child at eye level to ask which type of frames they like, their favourite colours, or favourite superheroes and Disney characters. This gives you time to assess the size of the child’s face and appraise their facial features and the required bridge fitting.
Ideally select five or six suitable fitting frames – having a selection empowers the child so they feel they are making decisions. This method also prevents the child from trying frames that are totally unsuitable for fitting.10 The frame size should be appropriate to the child’s development.11 The frame width should ideally match the child’s face allowing a straight path from the temples to the ear point.
Frames that are too wide can lead to sides being excessively bowed and difficult to keep in shape. Dispensing oversized frames with ‘room for the child to grow’ will inevitably be uncomfortable and unwearable, the same applies to scaled down versions of adult frames. Occlusion treatment or eye patching is prescribed in cases of amblyopia, a ‘sticky’ patch is worn on the face and spectacles over the top, the frame must be of sufficient size so that the child will not look over the top rim also fitting as close as possible to the eye without the lashes touching the back surface of the lens. Type of sides should be carefully considered to ensure a close fit with options for curl sides, ear locks or a head strap (figure 3).
Figure 3: Ear locks

A good nasal fitting should be of critical concern as 90% of the total weight of the spectacles is supported by the bridge; the main factor differentiating a good and a bad fitting is the amount of bridge surface resting flush upon the nose.1 Any digression from this balance is likely to cause discomfort. A good fitting bridge distributes the weight of the spectacles over a larger area of the nasal surface, creating less pressure and therefore providing more comfort.11 Ideally, the eyes should be positioned centrally in the frame.
The vertical eye position is determined by the frame crest height; therefore, the frame measurement should be low to match the facial measurement both right and left facial measurements are taken with the average of these used, typical crest height values for white British females aged four to six years range from 0.58mm to 7.95mm and males 2.13mm to 7.06mm.12 Knowledge of available frames that correlate to the child’s facial measurements is essential. Ideally the frame box centre distance should match the patient’s PD, resulting in minimum decentration, and even thickness at the nasal and temporal lens edges.
If an excessive amount of decentration is required for positive powered lenses, the nasal edge thickness will be increased, and conversely for minus powered lenses, the temporal edge thickness will be increased. When dispensing positive powered lenses ideally the minimum size uncut should be ordered to reduce centre thickness and spectacle magnification. A large apical radius is required to match the young child’s anatomical facial features. Ideally, the frame should provide constant touch around the bridge and more support at the bottom of the nose pad area.
The bridge should supply a larger splay angle to increase the distribution of weight over the bearing surface and provide a comfortable fitting.1 If the frame apical radius is too small, there will be a gap on the child’s bridge, resulting in red marks and soreness on the sides of the nose (see figures 4 and 5).
Figure 4: Apical radius too small (left) and Figure 5: Apical radius too small (right)

As the facial features develop, the crest height increases, the apical radius decreases, and the bridge projection increases to become slightly more positive.13 It is encouraging to note there are new ranges of frames available to meet the requirements of younger children’s facial features, they include Centro Style, Exeter Eyewear, Stepper, Millmead Optical and Tomato.
Pads may be changed to improve the bridge fitting; the size and shape vary. Larger pads distribute the weight of the spectacles, whereas small pads can be used to avoid the canthus, whereas saddle bridges provide support over the patient’s bridge. Hard acetate pads should be changed to the silicone variety, providing the benefit of being nonslip and hypoallergenic. Silicone insert bridges can be fitted to plastic frames to raise the position of the frame on the child’s face. This ensures the frame horizontal centre line (HCL) is correctly positioned at the lower limbus, preventing the child from looking over the top rims.
Adaptions can be made to both plastic and metal frames to improve fitting. When dispensing children’s sunglasses, the ideal balance is required between selecting large frames that fit close to provide light protection, and frames that do not rest on the cheeks or touch the eyelashes. At around nine years of age, the bridge starts to form the facial characteristics of the child’s adolescence; by the age of 13 years the bridge is almost fully formed.14 For fashion conscious youngsters there are now a variety of frames available including designers such as Chloe, Lacoste, Ray-Ban Junior, and Ted Baker. For sporty youngsters Nike, Oakley Junior, football team favourites and Flexon are ideal.
Sizing the sides
These days side lengths are often only available in one total length, which inevitably for young children are too long therefore some adjustment will always be required to improve the fitting. Various types are available, including loop end for babies and very young children, curl sides are useful for toddlers and older children, and for school age, curl or drop end are appropriate15 (see figure 6). The sides should rest comfortably from the ear point and over the back of the ear as well as against the head; following assessment, the sides invariably require shortening to provide the ideal fitting. Metal sides can be easily reduced, firstly measuring the length to bend from the dowel point to the ear point,14 generally allowing a drop of 30 to 35mm for a comfortable fitting depending upon the size of the child. To reduce the length of side remove the end tip then safely using an appropriate pair of side cutters trim to desired length.
Figure 6: Sides too long, pantoscopic angle zero and frame touches brow

The end of the side now needs to filed to a smooth round finish before the end tip is re-fitted. Plastic sides can be shortened by two different methods. Firstly, by cutting the end tip, filing to an even finish and buffing. If dispensing acetate or propionate materials, acetone can be used to smooth the tip. This method may prove unattractive, particularly if the sides are thick or the drop is slightly triangular/pyramid shaped or the reinforcing wire then comes right to the end of the side potentially creating a sharp dangerous protrusion. Alternatively, if possible, the side can be cut at the joint and the half joint re-sunk or re-pinned, however this method is unsuitable if the half joint is soldered to the reinforcing wire.
Although this results in a better finish, it is not advisable if the side has a designer logo, as this may be reduced or cut off completely. Fitting standard ‘ready-made’ curls in practice is a task easily completed by a dispensing optician. They simply push-fit onto a cut side, ensuring the correct internal diameter to match the diameter of the side wire, and allowing for the depth of the core, which is usually 10mm. Often applying a small amount of glue can be used but parents and patients should be warned that if the curl is pulled off, a sharp metal side remains, which results in a potential hazard. A basic method of measuring the correct required length for a curl side is to use a piece of ribbon, string or, alternatively, supra cord, to gauge the total length of side.
The ribbon, string or supra cord should be measured from the dowel point (side screw), extending around the back of the ear, and stopping short of the lobe.11 This provides the measurement of the total length of side, the other measurement required when ordering a curl sides is length to tangent (figure 7) shows an example of too long length to tangent and to long total length. Tomato frames provide simple adaption options for tailoring side lengths to a child’s individual requirements (figure 8). Frame repairers will be able to cut the side and attach a curl by soldering. Curl sides are now generally supplied with silicone covers to provide durability and comfort it is suggested they should be checked and re-adjusted every three months.
Figure 7: Curl side too long and Figure 8:Tomato frame easily adjustable curl side
Opinion among peers advocates that children under two years of age should not be fitted with a curl side as the cartilage of the ear has not yet fully developed. Incorrectly fitted curl sides could result in the child’s ears protruding in a cosmetically unattractive manner. The ideal dispensing solution for this age group is to fit loop end sides with elastic or silicone ribbon threaded through the loops, thus enabling a secure frame fitting. Sports bands are also available to keep drop end sided frames in place and are obviously useful if the child is required to wear their correction for sports.
Anthropometric data shows that young children have flatter faces and longer eyelashes compared to adolescents and teenagers.12 Their pantoscopic tilt is typically zero degrees, which is also a requirement for children dispensed with myopia management spectacles. It should be remembered that this is an ‘as worn measurement’16 and not confused with angle of side. Regular adjustments to the frame will be required as the child grows, therefore it is advisable that the frame fitting on the patient should ideally be checked every month.
Frame materials matter
Lightweight flexible injection moulded plastics materials such as silicone and Grilamid (TR90) are hypoallergenic and offer strength and durability (figure 9), for example, Centro Style, Stepper, and Tomato frames although most frames sold today are still acetate and plated metal. A newer introduction to the market Flexon (memory metal), is ideal for active children and those with a tendency to frame breakages.
Figure 9: Tomato frame, TR90 material with adjustable pads on arms ensures a comfortable fitting

Flexon sides cannot be shortened as it renders them impossible to adjust to a drop, therefore specific shorter sides should be ordered. Titanium and stainless steel provide hypoallergenic options for metal frame materials and improved alloys and construction of modern metal frames provides strength, flexibility, and corrosion resistance as well as reduced breakages. Due to the zero nickel content they provide an option for active children or those with sensitive skin.
Shrink-wrapping silicone tubing to plated metal sides consisting of a copper and nickel alloy does afford some protection for those with skin allergies and contact dermatitis. Exposing copper to the oils or salts secreted from the skin causes oxidation turning the metal frames and nose pads green (verdigris). It is important to gauge the child’s activities against the type of frame being chosen, evaluating their history of breakages, repairs and current eyewear, to provide an indication to their handling and wear.
Small glasses supplement (SGS) and Special facial characteristics (SFC)
Claiming SGS or SFC provides additional funding for parents/carers on top of the spectacle voucher GOS3 and there is no longer a maximum age applied for this supplement further details can be found within Making accurate claims in England 2022, which can be found at abdo.org.uk/wp-content/uploads/2022/05/MACE-guide-2022.pdf. When applying either SGS or SFS it is essential that all details are recorded within the patient’s record and the orders for the frame, lenses or modification retained.
Supervision of Supply
Verification of paediatric prescriptions still falls within the criteria of a restricted category and so must be carried out by or under the supervision of a registered optometrist, dispensing optician or ophthalmic medical practitioner. The spectacles must correspond to the written prescription/specification and should be set up to match the information recorded on the patient’s records. The collection visit is also subject to the same regulation and the practitioner must ensure the spectacles fit the patient and deliver the intended visual correction.
Information regarding modality of wear should be again given to the patient, parent/carer along with advice on adaption and the importance of returning to the practice regularly for adjustments to ensure correct fitting is maintained. At collection the child should be made to feel special – involve them in the choice of spectacle case and cloth and compliment them on their new spectacles. Use phrases that the child will remember, for example, ‘when they’re not on your face, place them in the case.’
Most children who attend for an eye examination require spectacles to be dispensed. As with adults, one pair of spectacles often does not meet the child’s lifestyle requirements; for example, sports, hobbies, light protection, safety and use of digital devices – all should be considered, and the appropriate frames and lenses recommended. If we fit a child incorrectly, in some cases we can cause permanent harm. However, if we get it right, the practice-building opportunities from paediatric dispensing are vast.
- Sally Bates BSc (Hons) FBDO Cert Ed is a registered dispensing optician and proprietor of Identity Optical Training, which provides training and CPD for optical assistants, dispensing opticians and optometrists including bespoke training for independent practices. Her website Specs Education with Sally, specseducation.com, provides targeted support for student dispensing opticians prior to sitting their ABDO Practical Final Qualifying Examinations. Sally has more than 30 years of experience in writing, designing, developing and presenting optical learning including the dispensing related content for the OT Skills Guide series on YouTube. She regularly presents at industry leading CPD events including 100% Optical, Specsavers PAC, and the annual conference of the Irish Association of Dispensing Opticians.
References
- Keirl A. Paediatric Eyecare part 2, Anthropometry and spectacle frames for children, Dispensing Optics. 2010, October.
- Great Britain. Opticians Act 1989. Chapter 44, Part IV. Section 27. London. Stationery Office. 1989. Available from : https://www.legislation.gov.uk/ukpga/1989/44/part/IV
- Association of British Dispensing Opticians. Pathway for Dispensing to Children. Available from: https://www.abdo.org.uk/wp-content/uploads/2019/04/Pathway-for-dispensing-to-children-0617.pdf
- College of Optometrists. Clinical guidance Supervising The Sale and Supply of Spectacles. Available from: https://www.college-optometrists.org/clinical-guidance/guidance/knowledge,-skills-and-performance/sale-and-supply-of-spectacles/supervising-the-sale-and-supply-of-spectacles
- College of Optometrists. Clinical guidance working with colleagues supervision. Available from: https://www.college-optometrists.org/clinical-guidance/guidance/communication,-partnership-and-teamwork/working-with-colleagues/supervision
- Griffiths AI. Practical Dispensing (3rd Edition), ABDO, London, UK, 2000; pp 77-85.
- Daw NW. Critical Periods and Amblyopia. JAMMA Ophthalmology. 1998; 116(4): 502-505. Available from: https://jamanetwork.com/journals/jamaophthalmology/fullarticle/262202
- Wu C, Gaier ED, Nihalani BR, Whitecross S, et al. Durable Recovery Form Amblyopia with Donepezil. Scientific Reports. 2023;13, 10161. https://doi.org/10.1038/s41598-023-34891-5
- General Optical Council. 8. Maintain adequate patients records in Standards of Practice for Optometrist and Dispensing Opticians. London. General Optical Council. P.13
- Millington A. It’s as easy as ABC, Dispensing Optics. 2017, June.
- Schramm KD. Dispensing Paediatric Eyewear. Butterworth Heinemann, Boston, USA. 2000.
- Thompson A. Paediatric Facial Anthropometry Applied to spectacle Frame Design. {Online}. https://publications.aston.ac.uk/id/eprint/43749/1/THOMPSON_ALICIA_JANE_2021.pdf
- Obstfeld H. Spectacle Frames and their Dispensing. WB Saunders Ltd, London, UK. . 1997.
- Keirl, AW. Anthropometry and spectacle frames for children part 1. Dispensing Optics. 2009; vol.10, pp.4-12. 5.
- British Standards Institution. BS EN ISO 8624:2020. Ophthalmic optics. Spectacle frames. Measuring system and vocabulary. London: BSI; 2020.
- British Standards Institution. BS EN IS0 13666 : 2019. Ophthalmic Optics. Spectacle Lenses. Vocabulary. London : BSI ; 2019.
