Dry eye disease has a significant and well-documented impact on quality of life for patients. Wonderfully, nowadays, thanks to significant global innovation and investment, and an ever-growing interest from practitioners, we have a growing armoury of treatments available. As practitioners we cannot, however, always quantify the impact of intrinsic lifestyle choices or external factors when attempting holistic management of this chronic condition.
Patients frequently have a desire to understand what else they can do alongside their prescribed regime to maximise their comfort and minimise the impact of the disease on their day-to-day lives. For many years, as clinicians, we have doled out advice regarding certain presumed beneficial lifestyle modifications such as avoiding fans, blinking and 20-20-20 screen use rules, without necessarily having robust consensus on what is appropriate or likely to yield the best outcomes in each individual clinical case.
The Tear Film & Ocular Surface Society (TFOS) Workshop, ‘A Lifestyle Epidemic: Ocular Surface Disease’, was initiated to answer this very element. The workshop was brought about by the work of global charity, TFOS. Their latest united global venture was guided by this common desire to better comprehend the direct and indirect impact of modern life on the ocular surface. The global panel of experts (a total of 158 members from 38 countries around the world) were the first to undertake a comprehensive evidence-based review of the literature on how lifestyle and societal factors impact the ocular surface.
Eight reports – contact lens (CL) wear; cosmetics; digital screen usage; elective medications and procedures; climate; lifestyle; nutrition; and societal challenges – were published (www.tearfilm.org).1 As well as these, three further subcommittees reviewed and worked on evidence quality, industry liaising and public awareness. The quality of evidence was assessed using the American Academy’s three-level Preferred Practice Pattern guidelines for evidence grading. Alongside these reviews, each subcommittee worked to answer a key question using systematic review methodology.
In collating the reports, there often was not enough high-quality evidence to draw definitive conclusions about a given factor’s effect. Hopefully, these reports will inspire others to further research to plug the gaps. This series of eight Optician articles will summarise the key findings from each subcommittee report and expand on how this is relevant to good evidence-led clinical practice in each topic area. All references can be found in the full TFOS reports.
TFOS Optician series: The Contact Lens Report
The TFOS Lifestyle: Impact of contact lenses on the ocular surface report investigates the CL choices that may impact the ocular surface and the lifestyle choices made by wearers that ultimately affect CL wear and success. The key findings of the report and its clinical implications will be outlined in this
article.
CL choices and their impact on the ocular surface
CLs have the capacity to enhance the lifestyle of individuals, primarily for the correction of refractive errors, but also for many other reasons, including medical indications. It is estimated that approximately 150 million (2%) of people wear CLs globally.2 For those wearing CLs, numerous factors will govern wearer success. CL wearers are primarily young and female, and most lenses fitted in 2021 were still single vision lenses. In 2021, soft CLs accounted for 86% of all lens fits.3 Of those, 45% were spherical lenses, 32% toric and 14% multifocal CLs.
When considering presbyopic CL wearers only, in 2021, 49% were fitted with multifocal lenses, 11% with monovision and 40% with single vision lenses. In 2021, nearly 50% of all CLs prescribed worldwide were daily disposable lenses, although there are significant differences between countries. The benefits of daily disposable lenses include:
- Convenience
- Absence of a solution-based care system thus reduced risk of solution toxicity
- Easy access to spare lenses
- Potentially better vision satisfaction
- Improved comfort
- Lower incidence of inflammatory complications
Originally introduced for overnight wear, due to their high oxygen transmissibility, silicone hydrogel lenses account for 75% all soft lens fits worldwide in 2021. On average, lens wearers wear their lenses approximately six days per week, but frequency is dependent on age, sex, lens type and design. Approximately 3% of all lens fits in 2021 were orthokeratology designs, with considerable differences between countries. In recent years, many soft CLs for myopia control have been brought to market and in 2021, 2% of all soft CLs were prescribed for myopia control.3
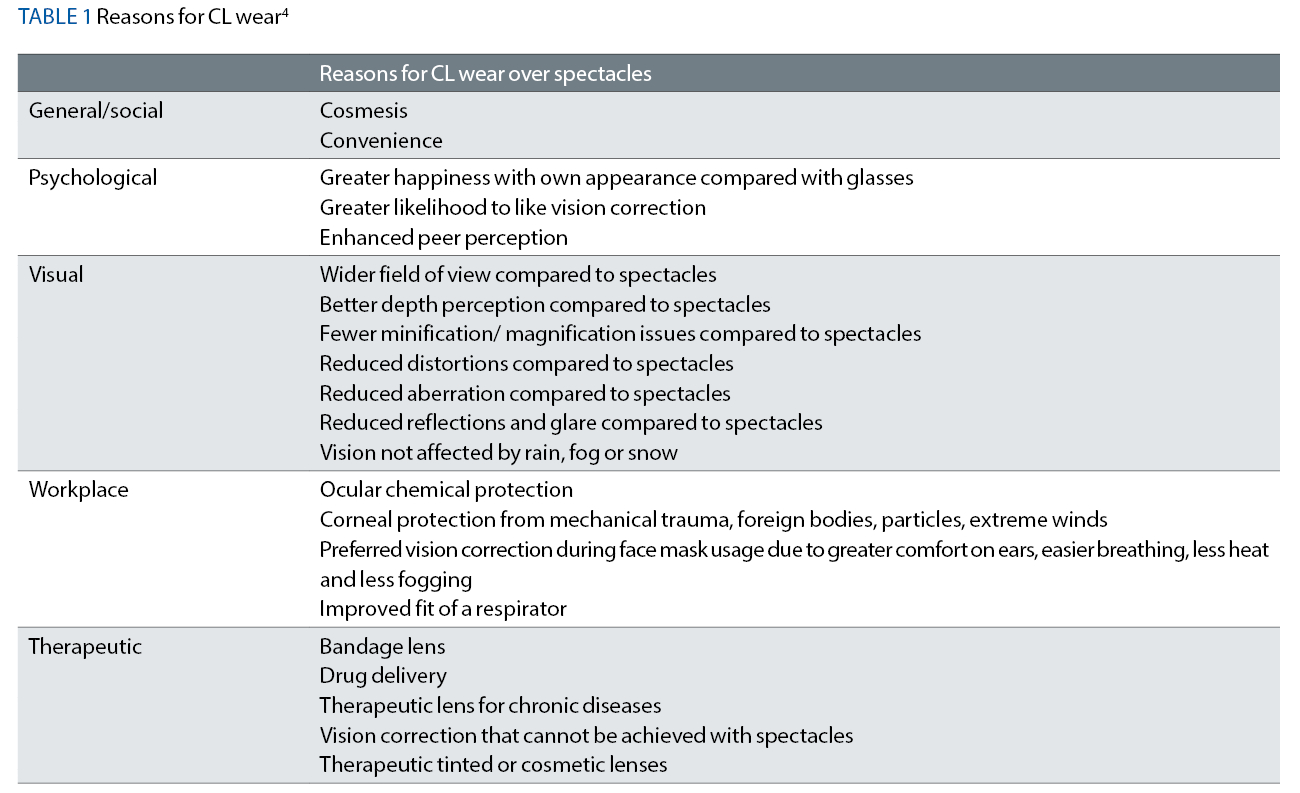
There are many current reasons why individuals choose to wear CLs, these are summarised in table 1.
Discontinuation
CLs differ in their performance, and patient success is linked to a myriad of factors relating to the surface and bulk properties of the lens material, their design, fit and frequency of replacement. CL wear discontinuation rates remain at around 25%, although this estimate varies depending on the definition of ‘discontinuation’ and the country being considered. Ocular discomfort is the most cited reason for lens discontinuation in established CL wearers.
Other reasons include inconvenience, cost, and poor vision. Shorter tear film break-up time after three months of lens wear discontinuation, greater likelihood of dry eye diagnosis, meibomian gland plugging and worse meibum quality have been observed in CL dropouts when compared to age and sex-matched successful lens wearers. Driven by cosmesis, convenience and resolution of discomfort, most lapsed wearers will attempt to resume CL wear.5
Ocular surface impact
Placement of a CL onto the cornea leads to compartmentalisation of the tear film into a pre-lens and post-lens tear film, thereby disrupting its structure and stability. A reduction in tear film break-up time, thinning of the lipid layer, and increase in tear evaporation rate have been associated with ocular discomfort during CL wear. There has been debate about the impact of CLs on meibomian gland structure, atrophy and function. Recent reviews have concluded that CL wear may impact certain aspects of meibomian gland function. As a result, a proactive approach should be taken to facilitate specific early management of meibomian gland dysfunction in wearers.
Non-adherence
Non-adherence to advice from practitioners on appropriate lens wear and care is rife among lens wearers, with some publications suggesting that over 80% of patients will be non-adherent with a behaviour that will put them at risk of developing a serious complication. Non-adherence may include:
- Reusing lenses inappropriately
- Using solutions or cases incorrectly
- Poor hygiene
- Overwear
- Sleeping in CLs
Almost 100% of CL wearers will, at some point in time, exhibit at least one CL hygiene risk behaviour. It is important as practitioners that we understand these numbers and proactively address issues with patients.
Lens deposition
Interaction between a CL material and the tear film occurs rapidly, and deposition of both protein and lipid can be demonstrated within minutes to a few hours of exposure to tear film components. The uptake of these various tear film proteins and lipids are complex, vary depending upon the charge, size and hydrophobicity of the tear film component and the chemical composition, water content, ionic charge, pore size and hydrophobicity of the CL material.
To date there is little supporting evidence regarding less deposition being a better aim, rather the actual state of the tear film contaminant may be the more significant factor. Increased subjective CL comfort has been correlated with a higher proportion of active, rather than denatured, lysozyme deposited in daily disposable wear of etafilcon A lenses, with the quantity of lysozyme being unrelated to lens performance. Lipid deposition has been reported to be higher in asymptomatic wearers of silicone hydrogel senofilcon A lenses compared to symptomatic wearers, suggesting that deposition of certain lipids may actually have a positive impact on lens comfort.
CL solutions
In past studies, patients using hydrogen peroxide-based CL disinfection systems have reported significantly better comfort compared with those using multipurpose solution systems, with other studies showing a similar incidence of complications between the two disinfection systems. Since the hydrogen peroxide-based systems do not typically contain preservatives, which have been implicated in dry eye disease and CL associated dry eye, it may be that the increased comfort was the result of the lack of preservatives in the system.
As a result of these reports, peroxide-based systems are sometimes preferred among some eye care practitioners when managing CL wearers with dry eye disease. However, it is worth remembering that the stability of the tear film can decrease with the use of any CL cleaning system. In general, there is little reported difference in the extent of lid wiper epitheliopathy or comfort between the use of different multipurpose solution or peroxide solutions. There does not seem to be a relationship between solution compliance, including rub versus no rub protocols and ‘topping off’ solutions, and the incidence or development of dry eye disease.4
Lifestyle choices that impact CL performance
Access to CL and aftercare
The way in which consumers access CLs and aftercare varies. Unregulated supply occurs from sources such as internet sales or ‘over the counter’ outlets. CLs can be acquired without a valid prescription from many of these sources, and therefore wear and CL care is often undertaken without adequate supervision. Access to CLs through such unregulated supply outlets varies round the world.
Reports indicate that up to 23% of CL wearers purchase from the internet. CL purchase from unregulated outlets, particularly internet purchase of lenses, has been shown to carry increased risk of CL-related eye problems, including significant sight-threatening adverse events. This may be due to the lack of verification of acceptable CL fitting, and education regarding general hygiene practices and lens disinfection.
In addition, the frequency of eye examinations is lower among those who purchase CLs online or in retail stores. Face-to-face consultations offer the advantage of tailoring advice to individual CL wearers and potentially preventing severe complications from occurring. Therefore, it is worthwhile educating CL wearers as to the benefits and safeguards when lenses are dispensed and followed up by trained professionals.
Health and ageing
There are many factors involved regarding how poor health or increasing age can influence the ocular surface and CL wear.
Illness
The prevalence of ocular manifestation in Covid-19 patients was estimated to be 11.03%, with the most common manifestation being conjunctivitis or dry eye/foreign body sensation. There is emerging evidence that so-called ‘long Covid’ is associated with a loss of corneal epithelial nerves and an increased density of immune cells in the cornea, which may have implications for CL wear in the longer term.
An understudied area of CL wear involves what to do when a wearer is ill with a viral upper respiratory infection, such as the common cold or influenza. The evidence related to the risk of developing microbial keratitis in those who are unwell was determined to be inconclusive in a review, but in contrast, evidence exists of a potential link between being unwell and occurrences of corneal inflammatory events associated with CL wear.
Allergy
Several studies have demonstrated the potential benefits of daily disposable CLs in patients with allergic conjunctivitis. Studies showed that during wear of daily disposable lenses, participants experienced fewer ocular symptoms, better comfort, and showed improved clinical signs. Recent work has focused on antihistamine (ketotifen) releasing CLs which have been reported to lead to significantly lower ocular short and long-term itch scores.
Topical drops
In the presence of soft CLs, interaction of topical drop formulations with the ocular surface is unpredictable, with resultant uncertain therapeutic efficacy. Other concerns are the risk of development of CL surface deposits or discoloration, particularly with soft lenses. Therefore, patients are advised to instil therapeutic eye drops before the CL is applied, or after it is removed for the day, a concept that also holds true for scleral lenses.
Younger age
As the field of myopia control grows, the impact of starting CL wear at a younger age on the ocular surface and cornea is of increasing interest. The incidence of corneal inflammatory events from studies is approximately equal to that seen in studies of adult CL wearers. The eyelid and conjunctival microbiota of children (aged eight to 14 years) wearing soft hydrogel lenses for two years comprised what is considered a normal ocular microbiota, did not change over time and was similar to other reports of the microbes from CLs of adults, suggesting that children can successfully wear daily disposable hydrogel CLs with minimal impact on ocular surface physiology.
Older age
Meibomian gland atrophy increases with age, and prolonged duration of CL wear has also been associated with a decrease in the number of functional meibomian glands. It has also been suggested that CL wear accelerates age-related changes in the meibomian glands. It is generally appreciated that with increasing age, the function of the ocular surface declines in association with a reduction in secretions of the various tear film components, reduction in sensation, and altered mucosal immune responses.
Ocular Demodex mite infestation is frequently observed in the eyelashes of older age patients, and is a possible causative agent of blepharitis. What might be considered a clinically significant infestation with Demodex when found in eyelashes of CL wearers remains uncertain.
Impact of co-existing ocular surface disease on CL wear
CL wearers with ocular surface disease may face additional challenges. They may have problems with eye discomfort, ocular redness, and/or deposits on the CLs, interfering with both comfort and vision. CL discomfort was defined by the 2013 TFOS International Workshop on Contact Lens Discomfort as ‘a condition characterised by episodic or persistent adverse ocular sensations related to lens wear, either with or without visual disturbance, resulting from reduced compatibility between the CL and the ocular environment, which can lead to decreased wearing time and discontinuation.’
More research is needed to determine whether CLs can induce dry eye (both signs and symptoms) in CL wearers who had no ocular surface disease prior to wear, and if so, what is the timescale and risk factors for this process. Common sense suggests that pre-existing ocular surface disease should be treated to minimise any signs and symptoms that might be confounded with problems associated with CL wear itself. This strategy is elucidated in the 2013 TFOS International Workshop on Contact Lens Discomfort. This report advised that options for patients who have CL discomfort or intolerance include:
- Modifications by way of lens choice, mode of wear, and care
- Addressing modifiable patient risk factors
- Treating underlying disease
- Improving the ocular environment
- Modifying the general environment
The report also concluded the use of topical artificial tears and lubricating agents, oral essential fatty acids, punctal occlusion and topical medications (eg azithromycin, cyclosporin A) may be beneficial, along with avoiding adverse environments (eg aircraft cabins) and altering blinking behaviour. There is some evidence that CL discomfort is attenuated by oral long-chain omega-3 supplementation. All these approaches have been used in the treatment of patients with dry eye disease or MGD and may be useful adjuncts in reducing CL discomfort, although evidence of their specific efficacy in the context of CL wear is still lacking.
Environmental factors and air quality
The predominant factor in many environmental impact studies may be CL dehydration due to low humidity, which is also further impacted by increasing airflow and decreasing temperature. Lifestyle choices resulting in changed environmental conditions may impact CL comfort, but further research is required. Air pollution can have a wide range of effects, from no symptoms to chronic eye discomfort and irritation. It has been suggested that the effects of air pollution in many indoor and outdoor environments are often overlooked.
Ocular discomfort could be an indicator of poor indoor air quality. A recent study reported that the least comfortable environments, as related to CL wear, are those that are dusty, polluted or smoky. Limited studies have observed the impact of pollution on CL wear. An evaluation of the influence of air pollution on tear film pH found a negative correlation between sulphur dioxide and tear pH, suggesting that an atmosphere with a high concentration of oxidizing agents exerts an appreciable influence on tear pH changes.
Office employees can suffer from ocular discomfort as a potential component of so-called ‘sick-building syndrome’. This term has been used to describe an increasingly common pattern of symptoms seen in workers in modern office buildings. The main cause of sick-building syndrome may be due to the recycling of air in rooms, traffic noise, poor lighting and the effects of buildings located in polluted metropolitan areas.
Blinking
CL wearers are more predisposed to incomplete blinking when using digital devices or reading, and the frequency and completeness of the blink are altered. Adequate CL wettability requires an adequate blink rate to be maintained. During CL wear, blinking promotes the even spread of the tear film over the lens surface, aiding lens surface wettability. Tasks that require high cognitive demand, computer use, and reading on smart phones may be associated with a decline in the blink rate and completeness, and thus an anticipated reduction in tear film stability. It is important therefore as clinicians we give good blinking advice to all CL wearers and keep this important but often overlooked element in mind for our patients.
Occupation, sports and recreation
Certain occupations and hobbies can influence the success of CLs. CLs have been shown to help protect eyes from projectiles and particulates found in certain occupations. Divers can face trapping liberated dissolved gas bubbles under lenses as they resurface, high altitude climbers can end up with reduced oxygen transmissibility through the lens leading to corneal dysfunction as well as the risk of the CLs freezing. Astronauts need a squeezable vial to obtain a solution globule as weightlessness prevents drop formation.
Risky behaviours
Higher risk-taking personalities among lens wearers are associated with poorer compliance and appear to be a better predictor of compliance than age, gender and practitioner perception. Sleeping or napping in CLs was a frequently reported behaviour and results in a heightened risk of corneal infection.
Exposure (direct or passive) to tobacco or marijuana smoke has been shown to cause unwanted and adverse ocular surface changes, as evidenced by an increase in tear film evaporation, oxidation of tear lipids, slowing of tear film spread time, increase of tear interleukin-6 concentration, and damage to the ocular surface epithelium.
Heavy alcohol intake alters tear film function, with an increase in osmolarity measures and disturbed cytokine production. Clinical evidence suggests that the use of soaps, lotions, and cosmetics can affect CL comfort and contribute to CL-related dryness. Deformation and CL swell of silicone hydrogel materials can also occur with the use of cosmetic and cleansing products.
Future prospects
Potential future uses of CLs include further widespread drug-delivery by CLs. Lenses are modified to carry the therapeutic dose in various potential ways: including the incorporation of polymeric nanoparticles, microemulsions, micelles, liposomes diffusion barriers (eg vitamin E) and sophisticated loading techniques such as molecular imprinting. Given less conjunctival vessel absorption occurs, less systemic effects may also be a benefit from this form of delivery.
Smart CLs may potentially be used in the diagnosis and treatment of various ocular and systemic conditions. They could potentially sense and monitor biochemical or biophysical changes in tear fluid, ocular surface temperature, intraocular pressure and/or pH value. These sensors may have a future role in detecting ocular diseases, optimising pharmaceutical treatments, and monitoring treatment efficacy in point-of-care settings.
Environmental impact of CL wear
CLs are medical plastics, and plastics are known to pose significant ecological and human health risks. The increased popularity of daily disposable CLs has resulted in more CLs and blister-packs being used and discarded. Flushing of CLs down the drain was reported to render them dangerous for the environment, since biological wastewater treatment was ineffective in breaking down these polymers.
The industry has taken steps towards aiming for greater sustainability across all areas. At the time of fitting, eye care practitioners may play an important role in informing patients about proper disposal and recycling options available locally for CLs and associated care products.
Potential Management Strategies for CL Discomfort
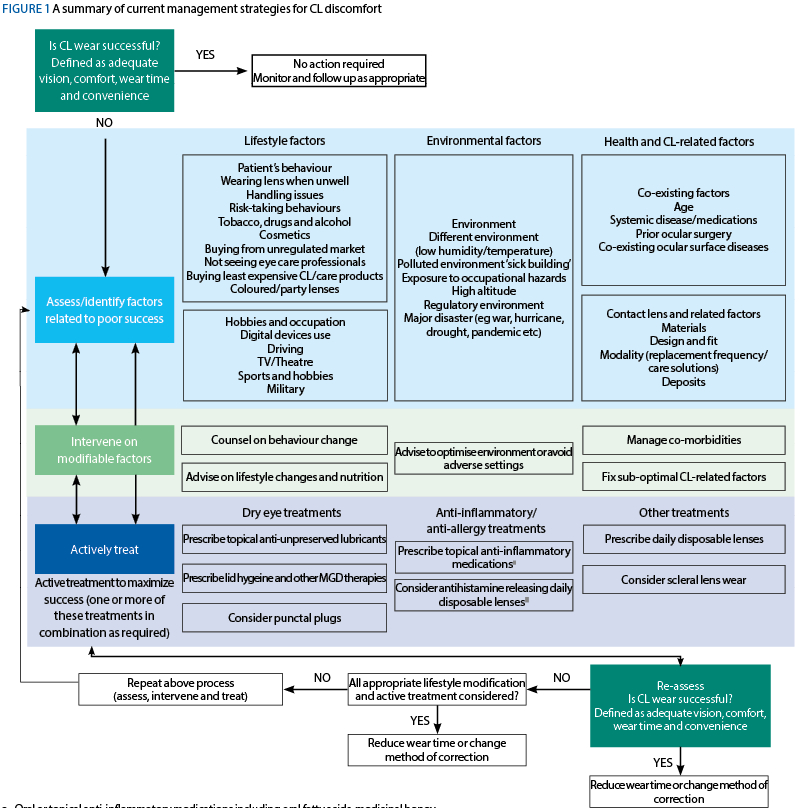
The subcommittee of the present report created a summary of current management strategies for CL discomfort (figure 1), which they considered a reasonable approach to addressing problems with CL wear in the setting of ocular surface disease, dry eye disease, or CL intolerance, based on currently available evidence.
Systematic review
The systematic review explored by the subcommittee examined the association of lifestyle factors and soft CL dropout. They found that further high-quality data is needed to provide information on the lifestyle factors that can lead to discontinuation of lens wear, which continues to occur in approximately 25% of wearers over a two-to-three-year period.
Unsurprisingly, the review found the most common reason for CL wearer dropout was lens discomfort. Yet, the most common reason for dropout among presbyopes using multifocal CL correction was vision quality. The most common general reason does indeed suggest that CLs are contributing to concerns of dry eye symptoms in a substantial number of patients.
Summary
The findings from the report allow us, as clinicians, to operate in the most current evidence-based way we can. The current consensus findings in this subcommittee are informative and allow us to confirm and establish best evidenced practice advice and techniques for helping to manage these patients get the best possible from their lenses. We can conclude that some lifestyle choices stress successful CL wear so it is important to make appropriate lifestyle choices in order to enhance the quality of life of CL wearers.
- Sarah Farrant is a director at Earlam and Christopher Optometrists, an optometrist and dry eye specialist and acts as a consultant and key opinion leader for a number of national and global companies. Farrant has a great passion for her work which is reflected in the wide variety of different interests she has within the profession. She has undertaken a number of additional qualifications and is a leading national expert in therapeutics and dry eye management and represents the UK as an Ambassador for TFOS. She is currently president elect for the BCLA and sat for 12 years on the executive and council boards for the College of Optometrists. She has been instrumental in a number of local and national initiatives in order to improve access to education amongst the profession and access to eye care for patients. She is also a keen lecturer and regularly teaches other optometrists both nationally and internationally.
- Ms Nikolina Budimlija graduated from the School of Medicine, University of Zagreb and gained a Masters in health management. She was a Fellow of the European Masters Program in Health Promotion. Budimlija trained in ophthalmic surgery at the Clinical Hospital Centre, Sestre Milosrdnice Zagreb. She was additionally trained in Austria, Slovenia, Spain and Switzerland and she brings more than 14 years of ophthalmic experience. Budimlija spent four years working as lead ophthalmic consultant at Health Centre in Zagreb. She joined Institute of Eye Surgery (IoES) in 2019 as ocular surface specialist and oculoplastic surgeon and she is running only dedicated ocular surface clinic in Ireland. She is a member of Scientific Committee at Irish College of Ophthalmologists, Member of Public Awareness Committee at Tear Film & Ocular Surface Society (TFOS), European Dry Eye Society (EuDES), European Society of Cornea & Ocular Surface Disease Specialists (EuCornea), Croatian Ophthalmological Society and the European Society of Cataract & Refractive Surgeons (ESCRS). She has participated as invited lecturer in numerous medical conferences worldwide.
• Further information can be accessed at tearfilm.org
Jones L, Efron N, Bandamwar K, Barnett M, Jacobs DS, Jalbert I, Pult H, Rhee MK, Sheardown H, Shovlin JP, Stahl U, Stanila A, Tan J, Tavazzi S, Ucakhan OO, Willcox MDP, Downie LE. TFOS Lifestyle: Impact of contact lenses on the ocular surface. Ocul Surf. 2023 Jul;29:175-219. doi: 10.1016/j.jtos.2023.04.010. Epub 2023 May 4. PMID: 37149139.
Acknowledgements
Lyndon Jones, Nathan Efron, Kalika Bandamwar, Melissa Barnett, Deborah S Jacobs, Isabelle Jalbert, Heiko Pult, Michelle K Rhee, Heather Sheardown, Joseph P Shovlin, Ulli Stahl, Adriana Stanila, Jacqueline Tan, Silvia Tavazzi, Omur O Ucakhan, Mark D P Willcox and Laura E Downie
References
- TFOS - Tear Film & ocular surface society [Internet]. [cited 2023 Nov 1]. Available from tearfilm.org/
- Nichols JJ, Willcox MDP, Bron AJ, Belmonte C, Ciolino JB, Craig JP, et al. The TFOS International Workshop on Contact Lens Discomfort: executive summary. Invest Ophthalmol Vis Sci. 2013 Oct 18;54(11):TFOS7–13.
- International contact lens prescribing in 2021 Contact Lens Spectrum. page; 2022.
- Jones L, Efron N, Bandamwar K, Barnett M, Jacobs DS, Jalbert I, et al. TFOS Lifestyle: Impact of contact lenses on the ocular surface. Ocul Surf. 2023 Jul;29:175–219.
- Dumbleton K, Caffery B, Dogru M, Hickson-Curran S, Kern J, Kojima T, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the subcommittee on epidemiology. Invest Ophthalmol Vis Sci. 2013 Oct 18;54(11):TFOS20-36.
