Dispensing opticians are highly skilled professionals, who work in various settings throughout the optical sector, the vast majority being in high street practice working as part of a multidisciplinary team dispensing spectacles to their patients. Of course, in today’s fast paced optical industry many patients will be seen by non-registrant colleagues, or even buy their eyewear online using their own judgment when selecting a new pair of spectacles.
The role of the dispensing optician (DO) is stated to be:
'A dispensing optician is a registered healthcare professional and plays various roles within an optical practice to meet the dispensing and clinical needs of patients. The core role of a dispensing optician is to advise on, fit and supply the spectacle frames and lenses most appropriate for each patient’s visual, lifestyle and vocational needs.'1
So, how can we guarantee that prescription eyewear is fit for purpose? I would suggest that seeing a dispensing optician may be the best way to ensure that any eyewear purchase is suitable, comfortable and achieve the best possible vision. The core role of a DO is, after all, to advise on, fit and supply the spectacle frames and lenses most appropriate to each patient’s visual, lifestyle and vocational needs.
The UK regulator, the General Optical Council (GOC), maintains a register of opticians, both dispensing opticians and optometrists, both bound by the same standards of practice. The standards relate to behaviour and professional performance. Additionally, the regulator states that:
'As a healthcare professional you have a responsibility to ensure the care and safety of your patients and the public and to uphold professional standards. You are professionally accountable and personally responsible for your practice and for what you do or do not
do, no matter what direction or guidance you are given by an employer or colleague. This means you must always be able to justify your decisions and actions.'2
This is important because many eye care professionals (ECPs) work in an environment, often with lots of standard operating procedures and commercial pressures, which may impact on decisions made relating to the care of their patients, it is however, important to note that the overarching duty of care is to the patient and the public, not the employer. The regulator has the power to take away the right to practise if a registrant optician falls short of the standard expected of them.
Best Practice
The dispensing of spectacles or any other optical appliance is best carried out by or under the supervision of a registered practitioner. ECPs will have the patients’ best interests at the heart of all that they do and to this end deliver patient-centred care.
The dispensing process may follow a series of steps to enable clear communication between all involved in the care of the patient and the patient themselves. Often the dispensing process may start within the consulting room at the conclusion of the eye examination. Many practitioners adopt the concept of a ‘three-way handover’.
This practice enables the optometrist to pass on vital information gained during the eye examination to the dispensing optician while within earshot of the patient and ensures continuity of care and affords the patient time to ask any questions or seek clarification on any issues that may have arisen during the eye examination.
There are also benefits in conducting this handover in the consulting room – any potentially sensitive issues are conducted in a more private area, and it also highlights the importance of treating each patient as an individual and tailoring any advice specifically to them and their needs.
At this point, the patient record should be fully updated, in case the patient wishes to return for the dispense at a later date or simply to ensure a seamless continuity of care that maintains clear contemporaneous patient records.3
Sarah Morgan, in an interview with Selina Powell,4 highlights key issues and tips locum optometrists might consider employing to ensure a smooth and successful handover. It is worth stating that the recommendations within this article are not only applicable to locum optometrists but also to employed and resident optometrists too. Sarah states: ‘A good handover is really essential to ensure full satisfaction.’
On leaving the consulting room, the dispensing process continues with the DO taking a more detailed history with regard to the dispensing than the optometrist would normally do. In addition to confirming driving status and screen use, all patients should be asked about potentially risky activities such as DIY or sports.
It is good practice to ask an open question like ‘what does your job involve?’ rather than presuming to know from its title. This is completed alongside analysing the prescription provided by the optometrist, which at this point is just numbers written on a piece of paper or on a neatly laminated card and does not constitute an optical appliance delivering best possible vision.
It is the DO who will interpret, then advise on suitable products after careful consultation with the patient considering their needs; vocation, lifestyle to enable the best optical solution for each patient. Sometimes it is impossible to address all issues in a single pair of spectacles, and multiple pairs may be required to meet the patients’ needs.
The Opticians Act (1989) S275 and the Sale of Optical appliances order of Council 19846 apply to both registered and unregistered sellers of optical appliances and clearly state that it is the seller’s responsibility to verify the appliance is in accordance with the prescription and where it is ≥ ±5.00D includes a vertex distance (measured from the corneal apex to the back surface of the lens)7 and when the dispensed vertex distance differs to that of the sight test adjust for effectivity error.
The measurement of the frame vertex distance on a prescription ≥ ±5.00D in the highest meridian including the reading addition is a legal requirement and therefore retailers that sell spectacles ≥ ±5.00D without making this check are acting illegally; this includes a number of online retailers.5,6
An unregistered seller can only effect a sale if there is a valid prescription, dated within two years, whereas a qualified registered DO does not require a prescription to dispense, they can take the prescription from an existing pair of spectacles using a focimeter. A DO or optometrist can also access information from their respective professional bodies’ advice and guidance. Both ABDO8 and the College of Optometrists9 have comprehensive sections on this on their websites.
I really want that one
Many patients at the conclusion of the eye examination leave the consulting room and head straight to the frame bars and begin the task of choosing their new eyewear. For many patients it is the frame choice that excites them the most, the latest fashion, or colour, or designer name is the driver for many people however, as ECPs, for us the frames and lenses are a medical device, which is more important.
We will, of course, be judged on the frame fit and suitability to hold the lenses and the overall feel and comfort of the finished spectacles, but how the patient actually sees through them is what is of utmost importance to us – indeed the whole fit, clarity of vision and comfort of the finished spectacles is what we as practitioners are ultimately judged on.
It can be a difficult balancing act to steer the patient away from the frame bars and to discuss with them their work habits, lifestyle and what they expect from their spectacles when all they want to do is try on the lovely shiny new frames.
Lens led dispensing has been employed by ECPs for many years, often discussing lens options first and ascertaining exactly what the patient requires of their eyewear makes it easier to direct them to appropriate frames to hold the lenses. It also means that if an appropriate frame is found after discussing the lenses, we almost never have to say no which is better for all ECPs and their patients.
While it would not be impossible to glaze a high plus prescription in a progressive lens design into a lightweight titanium rimless mount – careful discussion may uncover that a full rim plastics or metal frame in a lightweight material may yield a better result. Many other prescription anomalies are best addressed before frames are chosen to ensure the best possible, most aesthetically pleasing job can be produced.
Common prescription fails
Many prescriptions when written down seem innocuous and straightforward, however, their true idiosyncrasies may only be revealed after you receive a call from the lab asking you to confirm the order or advise that it is not possible to make. Or even worse the lab does not query the order, steams ahead, makes up the spectacles and, at best, they look cosmetically unappealing or, at worst, your patient cannot see through them.
Consider this prescription (Rx):
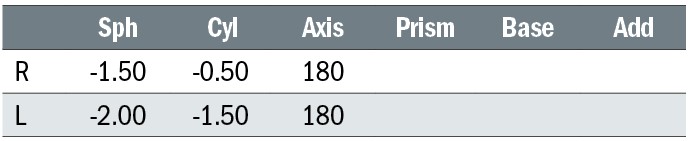
At first glance the prescription looks straightforward. A simple compound astigmatism single vision prescription. However, the wearer may complain of fatigue, and asthenopia – not all the time, but after prolonged bouts of reading. What might be the cause?
The above prescription is anisometropic – if we consider the near visual point (NVP) to be 10mm below the distance optical centre (the point we will assume the patient uses when reading), then we can calculate the differential prismatic effect at the NVP due to the Rx.
RE: Principal powers of the lens are -1.50D along 180 and -2.00D along 90
LE: Principal powers of the lens are -2.00 along 180 and -3.50D along 90
Using Prentice rule: P=cF we can calculate the prismatic effect in the vertical meridian for each eye.
RE: P = 1 x 2.00 = 2Δ Base down
LE: P = 1 x 3.50 = 3.5Δ Base down
So, the differential prismatic effect is 1.5Δ base down LE. We know that in general a differential prismatic effect of ≥1Δ can cause problems10 although this will vary depending on individual patient’s fusional reserves.
As previously stated, the patient may complain of general discomfort or fatigue, or even say that their binocular vision is not as good as each eye individually. Careful consideration should be given to alleviate these issues, perhaps a separate pair of spectacles with the centres lowered for near vision tasks or ask the patient to drop their chin when reading may be helpful.
Another option could be a compromise, position the optical centres 5mm below the pupil (which is likely to be on the horizontal centre line (HCL)) so task dependent the differential effect is halved. We could also remove the differential prism using a slab-off lens with the prism being ‘slabbed off’ the bottom half of the most minus or least positive lens. The author would recommend a conversation with the lab prior to ordering.
Consider another prescription (Rx):
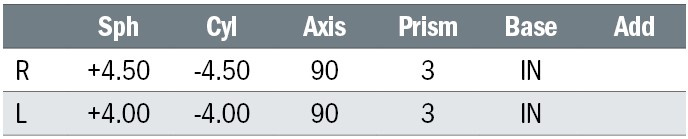
At first glance the prescription looks complex as there are significant cylinders and prescribed prism (base in) [perhaps as an aid to convergence in an older patient].
Again, if we consider Prentice rule and calculate this time the decentration required to produce the 3Δ Base in each eye, we see that there is in fact no power in the horizontal meridian, so we cannot achieve the prism by decentration and will require the lab to add the prism to the lens.
A moderate plus prescription in conjunction with base in prism could make for significant weight and thickness in the spectacle lenses, therefore frame options should be considered to minimise the size, weight and spectacle magnification of the lenses. Other more basic fails include not considering the prescription and how it will sit within a frame.
Consider a high minus prescription, conventional wisdom would suggest that choosing a thicker plastics frame to fully enclose the lens edges would be a good choice, however, sometimes we end up with a less than satisfactory result.
Consider this prescription (Rx):
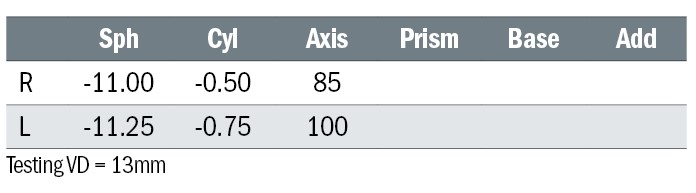
We fit the lenses to a full rim plastics rim frame, using standard CR39 s/v lenses. The frame size is 45 x 15, so BCD of frame is 60mm and OCs set at 46mm this results in each lens being decentred by 7mm each eye to ensure the OC is sitting on pupil centre. The resultant lens is thinner nasally, but thicker temporally, so closing the sides is virtually impossible (figure 2).
Figure 2: Poor example of dispensing high minus prescription

Solutions for this is to match the frame PD (boxed centre distance BCD) with the patient’s PD to minimise decentration which could be achieved with specialist children’s frames that offer a variety of sizes like Tomato frames or by ensuring high index or lenticular lenses are used enabling the sides to close and look more cosmetically appealing.
Consider a high hypermetropic prescription (Rx).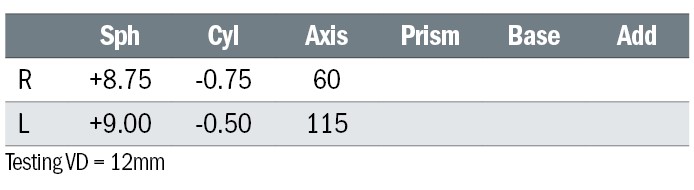
We fit these lenses into a full rim metal frame and ask the lab to surface the CR39 material to its minimum substance and use the smallest blank they have in stock. The frame size is 45x15, so BCD of frame is 60mm and OCs are set at 48mm, this results in each lens being decentred by 6mm each eye to ensure the OC is sitting on pupil centre.
The resultant lens is thicker nasally and thinner temporally, which makes adjusting the nose pads to fit almost impossible (figure 3). The only way to adjust these pads would be by using pliers pull the pads backwards before increasing the splay and/or frontal angle but this would increase the vertex distance substantially and the effective power. This dispense would need high index low base aspheric with consideration given to match frame PD (BCD) with the patient’s PD and minimise decentration.
Figure 3: Poor example of dispensing a moderate plus prescription

These four examples only highlight a small number of potential pitfalls of ophthalmic dispensing, sadly there are many more ECPs could fall foul of, so, it is therefore extremely important to take time to appraise the prescription, look for any anomalies or potential pitfalls before discussing eyewear solutions with patients.
It is also vital to look beyond the prescription and consider how the frame will sit on the face, where the lenses will be positioned within the frame, do you need to adjust the prescription for a difference in vertex distance or if dispensing an intermediate prescription for computer use or for reading music, do you need to compensate the prescription for working distance.
Similarly with more bespoke progressive lens fitting, do we need to take any additional measurements to ensure the lens is fitted correctly within the frame and have a note of frame fitting adjustments been recorded if not sending the frame to the lab for glazing? How can we even hope to get the best possible vision from a bespoke lens if it is not sitting in the position it was measured in?
The slightest deviation from the ‘as worn position’ or ‘as measured position’ will reduce the performance of the lens, and subsequently the patient will not achieve the best possible vision.
Best frame fit
Ensuring a perfect frame fit today is not an easy task. Many frames are mass produced and do not even come in different sizes – like so many other items, it either fits or it does not. A skilled DO can, of course, modify the fit to make it fit better, but the old adage – ‘you can’t make a silk purse from a sow’s ear’ – seems apt here.
Patients will often have a strong opinion of what type of frames they would like – often they prefer something similar to what they have had before, or sometimes, they fancy a complete change and would prefer to go for something completely different.
DOs can also suggest that the patient, should they want a perfectly fitting frame that they could opt for a handmade frame. This would employ the skill, and expertise of the DO taking all the appropriate facial measurements to produce a bespoke product for them. The measurements required are core a competence for DOs and while facial measurements are examined in both the Preliminary and Final Qualifying Examinations, many DOs never make a handmade frame in their entire career despite having the requisite skills to do so.
What patients find satisfying about wearing a handmade frame is that it is a ‘one off’ totally tailor made for them. Many companies will offer a fully bespoke option or can offer to change the parameters of existing stock models to fit a patient’s unique features, ensuring the best possible fit.
Figure 4: Example of a handmade frame

A quick internet search returns many companies who offer handmade and bespoke spectacle frames, which can be further enhanced by seeking out a competent and confident DO who is capable and willing to take on such a commission. Companies such as Cubitts11 manufactures its bespoke frames in Kings Cross, London, and Tom Davies12 manufactures bespoke frames from its facility in Brentford, London.
This article has served as a very short introduction to the common skills and expertise required when attempting the science and art of ophthalmic dispensing. Seldom is it straightforward, especially since it concerns dealing with individual people who have diverse and specific requirements and have different refractive errors and differences in achieved visual acuity, not to mention different hopes and aspirations from their spectacles.
Subsequent articles in ophthalmic dispensing will attempt to delve deeper into frame choice, lens selection and meeting and exceeding your patients’ expectations.
- Fiona Anderson BSc(Hons) FBDO R SMC(Tech) FEAOO is past president of the International Opticians Association, ABDO past president, past chair Optical Confederation, Optometry Scotland member, past Grampian AOC member, EAOO – co-opted trustee, ECOO European Qualifications board member, Renter Warden: Worshipful Company of Spectacle Makers, Worshipful Company of Spectacle Makers Liveryman & Fellow of the European Academy of Optometry & Optics.
References
- The Association of British Dispensing Opticians. The role of the dispensing optician. Available from: https://www.abdo.org.uk/about-us/dorole/Accessed [20th January 2024].
- General Optical Council. Standards of Practice for Optometrists and Dispensing Opticians. London. General Optical Council: 2016.
- General Optical Council. 8. Maintain adequate patient records, Standards of Practice for Optometrists and Dispensing Optician. London. General Optical Council: 2016. P.13
- Optometry Today. The how-to of handovers. Available from: https://www.aop.org.uk/ot/life-in-practice/business-management/2023/04/14/the-how-to-of-handovers Accessed [20th January 2024].
- Great Britain. Opticians Act 1989: Elizabeth II. Chapter 44. London. The Stationery Office;1989.
- The Sale of Optical appliances Order of Council 1984. SI 1778. London. The Stationery Office; 1984.
- British Standards Institution.Spectacle lenses – part 3: Specification for the presentation of prescriptions and prescription orders for ophthalmic lenses. London: BSI; 2008.
- Association of British Dispensing Opticians. Sale and Supply of Spectacles. Available from: https://www.abdo.org.uk/regulation-and-policy/advice-and-guidelines/clinical/sale-and-supply-of-spectacles/ [20th January 2024].
- College of optometrists. Sale and supply of Spectacles. Available from: https://www.college-optometrists.org/clinical-guidance/guidance/knowledge,-skills-and-performance/sale-and-supply-of-spectacles#Regulation [20th January 2024].
- Jalie M. The Principles of Ophthalmic Lenses 6th edn. Kent: Association of British dispensing Opticians; 2021 p.77
- Cubitts.Spectacles. Available from: https://cubitts.com/collections/spectacles?TN [20th January 2024].
- Tom Davies. Bespoke. Available from: https://www.tdtomdavies.com/bespoke [20th January 2024].
