In modern optical practices, it is common for healthcare professionals to take advantage of the wide range of ophthalmic lens materials available to support the best optical and cosmetic solution for the patient. While higher index lenses typically allow a greater choice of lenses to address cosmetic and weight concerns, eye care professionals should not be complacent in their dispensing decisions.
As with all dispensing solutions, a critical eye should be cast over all the products that we have at our disposal so that we can consider potentially negative aspects in relation to the product that may cause dissatisfaction and even intolerance.
Refractive index
The most referenced lens property in practice, including by some patients, is refractive index. It may be recalled that the absolute refractive index (n) of an optical media can be calculated by dividing the speed of light in a vacuum by the speed of light in the material.
Thus, higher index materials will cause light travelling within the media to slow down more than lower index materials.1,2 This change in speed directly influences the angle of refraction, as governed by Snell’s Law, with higher index lenses refracting light at greater angles compared to lower index lenses.
From an ophthalmic lens perspective, the refractive index directly influences the surface power of a lens3,4 (based on the surface power formula). As such, we can use higher index materials to reduce the curvature of lens surfaces, without compromising the surface powers, to produce thinner and potentially lighter lenses.
While the reduction of thickness has both a cosmetic and comfort benefit for a patient, and the dispensing of such lenses generally confers a commercial advantage to the practice, the pitfalls of thinner lenses must be considered.
Case study 1
Consider the following:
RE: +3.75 / +0.50 × 90 Add: +3.50 VAs: 6/18 N12
LE: +4.50 DS Add: +3.50 VAs: 6/12 N12
Patient wants to update their single-vision reading glasses, and is concerned about the thickness of the lenses. They have been previously dispensed CR39 single-vision plastic lenses in the past. This time the patient is considering a 1.67 index lenses. At first glance, this prescription lends itself well to the use of high-index lenses.
Indeed, alongside the use of minimum blank size surfacing by the lens manufacturer, the finished lens will certainly be thinner and lighter than the previous CR39 lenses. From the change in refractive index alone, this will equate to a reduction of approximately 27% in the surface sags.4
In addition, many high-index lenses in practice utilise aspheric surfaces to further decrease lens thickness. Although the use of high-index lens materials is recommended for generic patients presenting with such prescriptions, the impact on magnification should be evaluated in the context of low-vision patients. It can be recalled that the spectacle magnification (SM) is based on the power factor and shape factor of the lens:1,3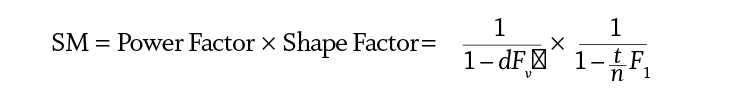
Increasing the index of the lens, which subsequently reduces the centre thickness, can result in a reduction in magnification (this reduction in magnification can be further enhanced with the use of aspheric lens surfaces and knife-edge surfacing).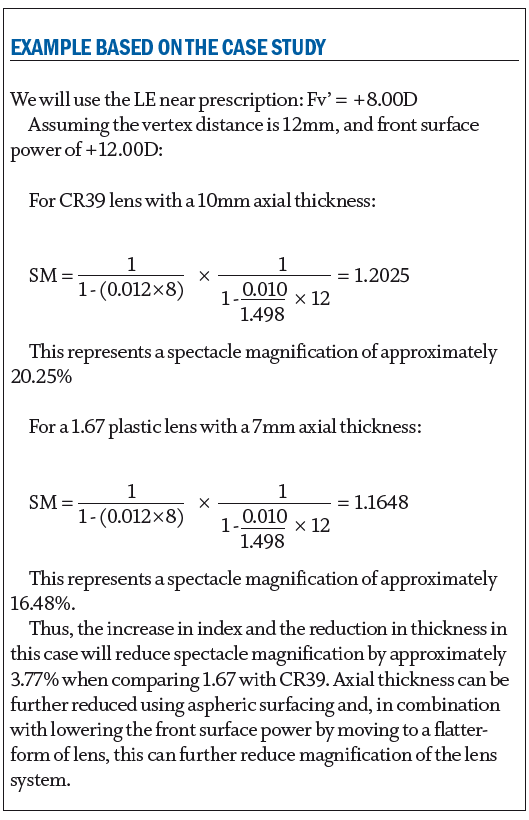
Although this reduction in magnification is generally desirable among the general ametropic population, in this case it may impact on the patient’s limited near-vision acuities and, as such, staying with a thicker lens may be a better low-vision corrective option (though communicating the justification to the patient and managing their expectations and frame choice will be required in such cases).
Aniseikonia (retinal image size disparity), typically related to gross anisometropic prescriptions, can also be reduced to a certain extent by potentially using different lenses in the right and left eyes.3 As observed in the above formula, altering the centre-thickness, form, and even refractive indices of the lens pair combination can offer some balance in the magnifications to help reduce aniseikonic disparity.
Constringence
Another property of spectacle lenses that should be considered when dispensing, especially in relation to higher lens powers and indices, is the Abbe number (or ‘V’ value) of a lens material, named after the physicist Ernst Abbe.5 Most light sources in our environment emit polychromatic light, which is light comprising of more than one wavelength (or colour).
As polychromatic light passes through a prismatic element, encountered when the patient looks off-axis or through prescribed prism, the different wavelengths (colours) making up the polychromatic light will pass through the lens material at different speeds. Longer wavelengths (red light) will travel more quickly than shorter wavelengths (blue light).1
As a result of these differing velocities, the material will have different refractive indices depending on the wavelength of light. From Snell’s law, if the refractive index changes, then the angles of refraction change and, thus, when polychromatic light passes through a prism it will be dispersed into its individual colours (figure 1).
Figure 1: Dispersion of polychromatic light (sunlight in this case) through a prism

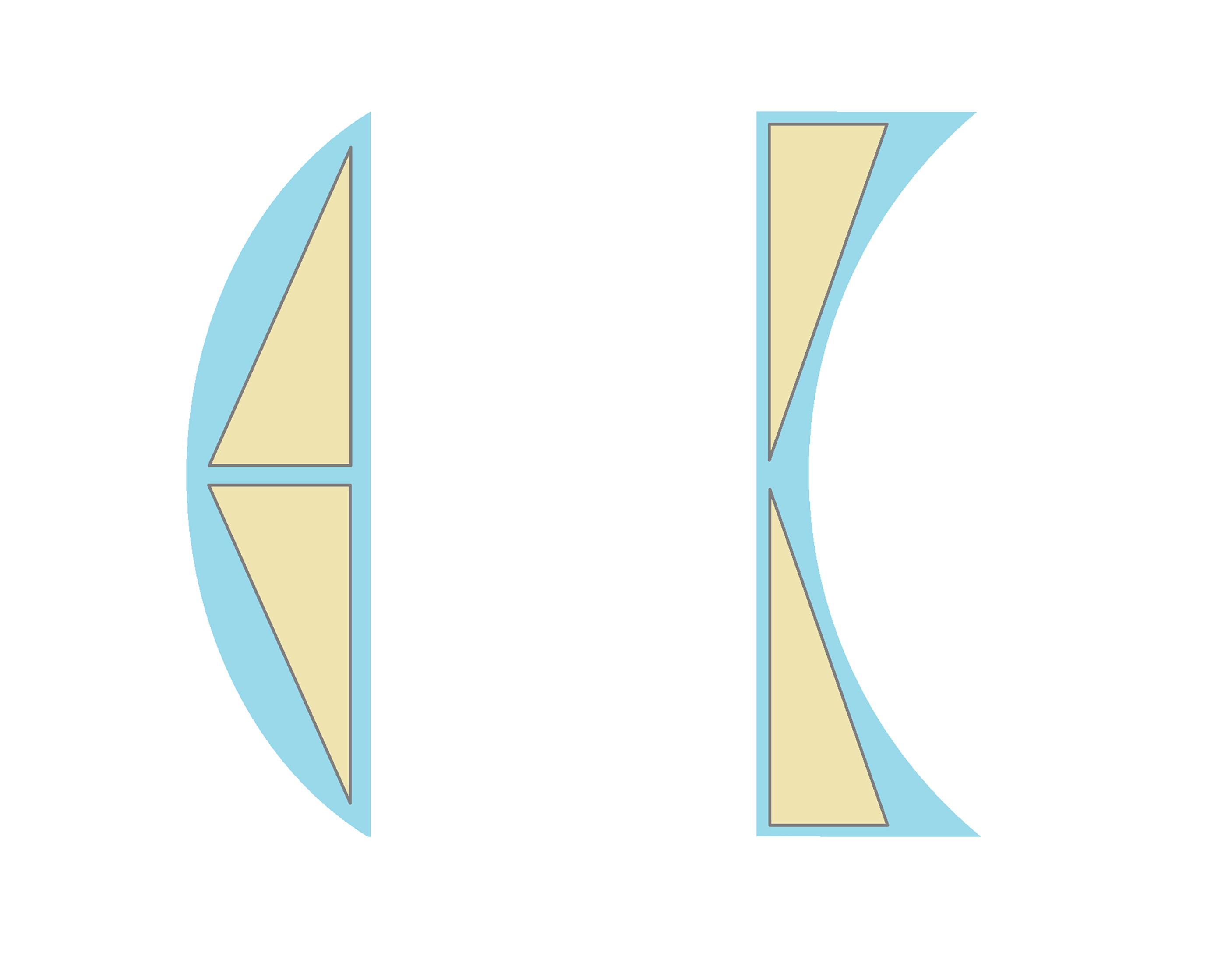
Different optical media disperse light to a greater or lesser extent, and this can be described as dispersive power within a physics context. In ophthalmic optics, the reciprocal of dispersive power is used, and describes the optical media’s constringence or Abbe number; the higher a material’s constringence, the less polychromatic light is dispersed into its individual colours (figure 2).
Figure 2: An optical media showing dispersion of polychromatic light (left), and dispersion with an optical media of lower constringence (right)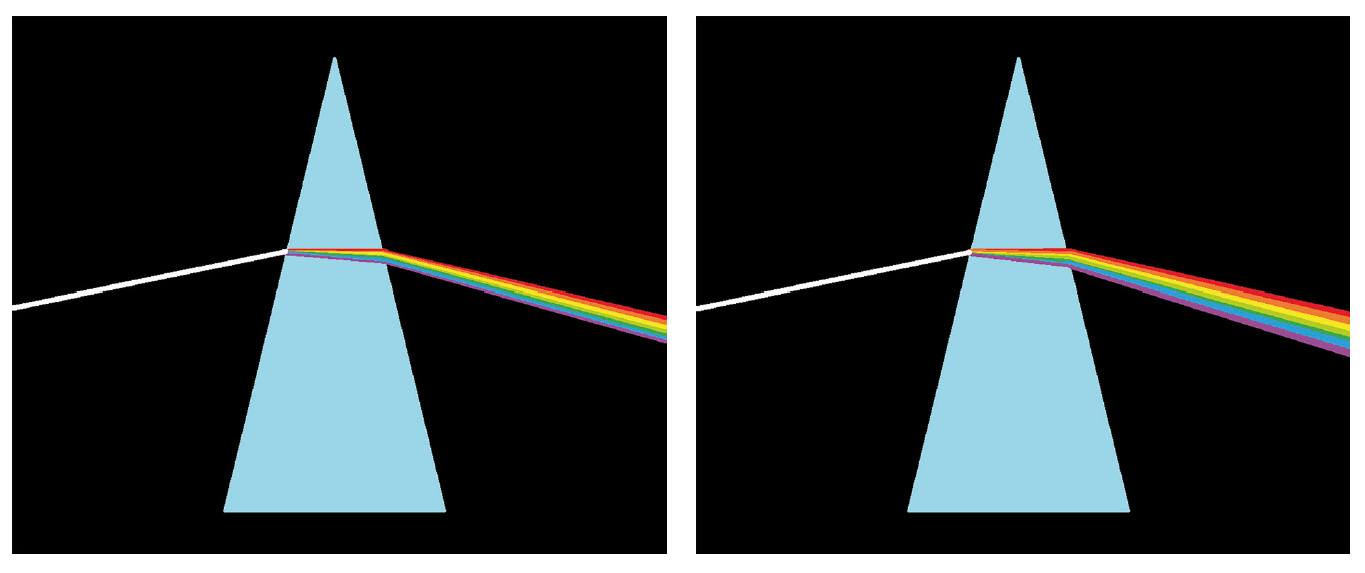
When developing any rigorous empirical measurement system, it should be designed in such a way that the system uses accessible constants to allow accurate replication anywhere in the world.
The Abbe number of an optical media is determined by utilising three Fraunhofer spectral lines from elemental emission spectra: a long-wavelength red F-line and a short-wavelength blue C-line from the Hydrogen spectra, and a medium-wavelength yellow d line from the Helium spectra.
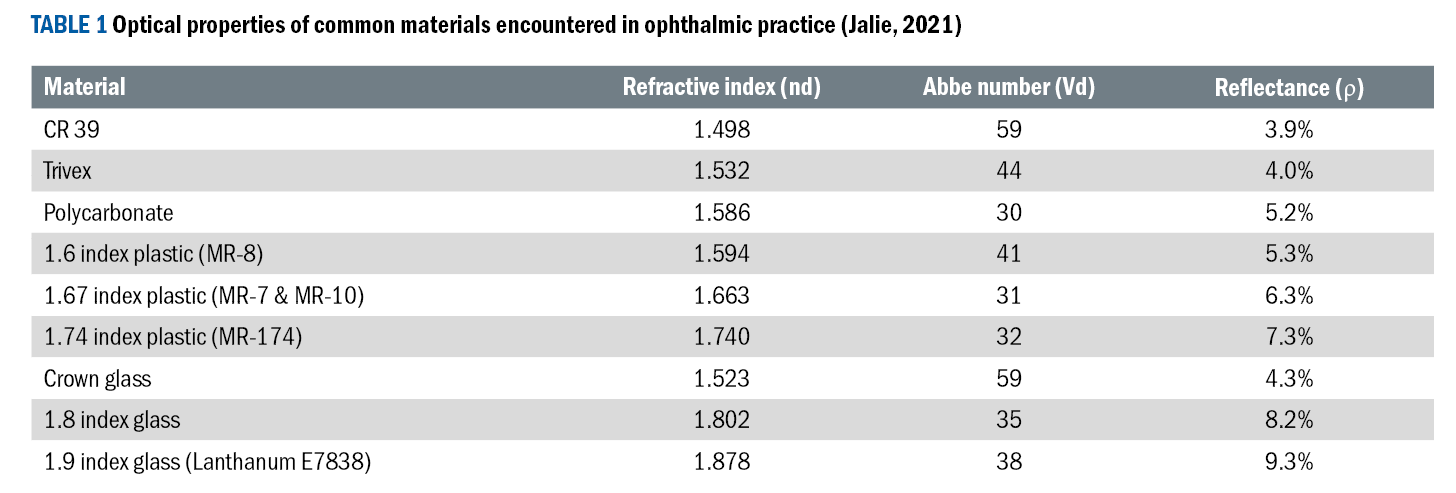
With the refractive indices derived from observed refraction of these wavelengths, a media’s constringence (Abbe-number/V-value) can be determined by:
 It should be noted that the ‘d’ line refractive index is also used to label the various lens materials within lens manufacturer’s catalogues and optical practices in the UK. Outside the UK, care must be taken when comparing lens material indices, as other countries use the green ‘e’ line from a Mercury spectrum as the mid-wavelength light for the purposes of labelling lenses and determining constringence, instead of the yellow helium line.
It should be noted that the ‘d’ line refractive index is also used to label the various lens materials within lens manufacturer’s catalogues and optical practices in the UK. Outside the UK, care must be taken when comparing lens material indices, as other countries use the green ‘e’ line from a Mercury spectrum as the mid-wavelength light for the purposes of labelling lenses and determining constringence, instead of the yellow helium line.
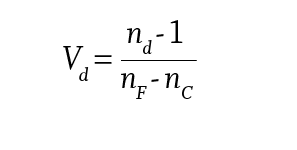
Within an ophthalmic lens context, the Abbe number tends to range from 30 to 60, representing lens materials with low constringence to high constringence respectively. Table 1 shows the Abbe-numbers of some of the commonly encountered lens materials.
Case study 2
Materials with low Abbe values have the potential to generate issues in relation to the patient’s visual experience and satisfaction which may require management of expectations. For example, consider the following situation:
RE: -8.00 / -1.00 × 100
LE: -8.50 / -0.50 × 75
This patient requires first-time prescription safety spectacles for high-velocity ballistic protection in their workplace. Polycarbonate lenses have been recommended by their employer.
Within an ophthalmic lens setting, high and very high refractive index lens materials typically have lower Abbe numbers, and hence less constringence, compared to standard index lens.6 As can be seen in table 1, one notable outlier is polycarbonate; although this is a mid-index material, polycarbonate typically has the lowest Abbe number compared to current ophthalmic lens materials.
Due to the safety rationale in this case-study, polycarbonate is an ideal material for ballistic protection due to its high tensile strength; however, we should consider potential optical issues linked with increased dispersion that may raise concerns with the patient. For the patient, dispersion of light can manifest as undesirable chromatic aberration when viewing through any prismatic element of the lens.
Prismatic effect is typically encountered as the patient’s gaze moves off-axis away from the optical centre and towards the periphery of a lens (figure 3), including when looking through the near-vision point (NVP) of a bifocal or varifocal lens.
Figure 3: A simple representation of off-axis prismatic elements with a convex and concave lens
 Care should also be taken when dispensing patients with significant amount of prescribed prism. Because there will be a prismatic element positioned in-line with the patient’s gaze, this can result in more noticeable chromatic aberration issues in the central field of view in these cases.
Care should also be taken when dispensing patients with significant amount of prescribed prism. Because there will be a prismatic element positioned in-line with the patient’s gaze, this can result in more noticeable chromatic aberration issues in the central field of view in these cases.
Patients troubled with this aberration often report the presence of ‘coloured lines’ or ‘colour-fringes’ when looking at high-contrast stimuli (figure 4), or they may state that their vision is not as sharp through the prismatic elements when viewing low-contrast stimuli. Dispersion of polychromatic light from stimuli can create two issues with the image.
Figure 4: Colour fringing as a result of dispersion of light. Note that the chromatic aberration increases as we look further to the edge of the lens, due to the greater prismatic effect
Firstly, as the constringence decreases, the image size is distorted due to the dispersive spread of light through the prismatic element of the lens, and this is known as transverse chromatic aberration. Additionally, as shorter wavelengths are refracted more than longer wavelengths, light from a polychromatic source passing through a lens will not form an exact point focus when it is refracted through a lens.
Instead, shorter wavelength light (ie blue) will come to focus before longer wavelength light (ie red); this is known as longitudinal chromatic aberration (or axial chromatic aberration), and can result in defocusing of the image. Longitudinal chromatic aberrations are not as perceptually noticeable compared to transverse chromatic aberrations, and this is partly supported by the absence of short-wavelength photoreceptors in the foveal region of the retina.7,8
Although chromatic aberrations are generally undesirable for the patient’s viewing experience, the principles behind longitudinal chromatic aberration are utilised in the duochrome test to help refine refractive prescribing,9,10 with the use of red/green stimuli which will come to focus at different focal lengths with a dioptric difference of approximately 0.44 dioptres.10
There are lens combinations used in optical systems, such as cameras and telescopes, that will help minimise chromatic aberrations, utilising multiple lenses in the form of achromatic doublets or apochromatic lens systems.2,3 Due to weight and thickness considerations, these solutions are typically impractical for spectacle lenses.
In the above case-study, managing the patient’s optical expectations should be addressed during the dispense. To reduce the impact of chromatic aberrations, a change of lens material to one with a better Abbe number could be considered. However, with the safety consideration being the priority in this case, it may be that polycarbonate is the only viable option to meet the protection demands, and therefore the potential aberrations should be discussed with the patient beforehand.
It should be noted that the ophthalmic lens material Trivex also possesses very high tensile strength for safety considerations,11 and has a better Abbe-number than polycarbonate, though the availability of this material currently remains commercially limited within the domain of safety spectacles.
Reflectance
Increasing the refractive index of a material also has implications when considering the reflectance of an optical material. Reflected light from lens surfaces is not only troubling cosmetically, but also enhances the visibility of ghost images for the spectacle wearer (figure 5).
Figure 5: Ghost images (circled) when viewing through an uncoated lens
Ghost images form because of one or more reflections at either surface of the spectacle lens, which can affect contrast and clarity of the observed image and even result in the creation of a double image due to internal reflection within the lens.6
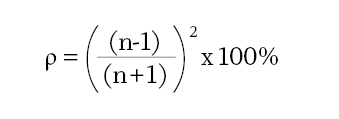
The reflectance (expressed as a percentage) of an optical material can be determined using:
Case study 3
A highly myopic patient has worn 1.9 index glass lenses, with anti-reflection coatings, in the past. They are frustrated that the lenses ‘get dirty too easily’ and are ‘difficult to clean’. They are happy with the reduced thickness of the 1.9 lenses, but would like to order their next glasses without the anti-reflection coatings.
In the modern practice, the majority of high-index lenses are generally provided with anti-reflection coatings from the outset. The rationale for this is clearly demonstrated when we consider the reflectance of uncoated high-index lenses. In this case, using the above formula, 1.9 index glass will have a reflectance of 9.6%;3 this is over twice the reflectance of a CR39 plastic lens (with a reflectance of 4%).
This is likely to result in poorer cosmetics for the wearer, and the perception of more distracting ghost images produced by primary reflections at the front and rear surfaces of the lens, or secondary reflections from further internal reflections within the lens media. As modern anti-reflection coatings typically utilise anti-static and oleophobic technologies, this case-study is less commonly experienced in practice.
However, should a patient raise concerns about the need of such coatings, the practitioner should consider the reflectance issues with increasing index and manage the expectations of the patient accordingly.
Density
The density of a spectacle lens, normally recorded in grammes per cubic centimetre, may also require consideration during the dispensing of spectacle lenses, as this directly affects the weight of the lenses and therefore the comfort of the spectacles. Density is sometimes referred to as specific gravity when comparing the density of a spectacle lens material with the density of water.
Thus, if you are comparing two materials with the same thickness and volume, the lens with the higher density will be heavier for the patient. This is certainly a disadvantage with the older crown-glass lenses compared to CR-39 plastics; the specific gravity of crown-glass (2.54g.cm-3) is almost twice that of and CR-39 (1.32g.cm-3).3
With plastic lens materials currently dominating the market compared to glass mineral lenses, the overall lens weight is perhaps less of an issue in relation to modern ophthalmic lens availability. Despite this prevalence of plastic lenses in modern practice, hi-index glass lenses still offer an alternative for thinner lenses, and it should not be forgotten that toughened glass safety lenses are still advised in certain hazardous environments (particularly when chemical or radiation protection is required).
Figure 6: A heat-toughened glass lens under a strain tester. Toughened glass safety lenses are still utilised in modern safety dispensing
Although very-high index glass materials, such as 1.9 index glass, are still used to provide a thinner lens for patients with high levels of ametropia, the weight of the lenses can still be a significant factor even though the thickness (and thus the volume) of the lens can be greatly reduced. Rare earth metals, such as titanium and lanthanum, are typically added to increase the refractive index when producing high-index glass materials.6
While this can provide us with refractive indices higher than current ophthalmic plastics and potentially thinner lenses*, the density of such materials shows a significant increase from that of crown glass (for example, the density of 1.9 index glass is around 5.04g/cm3, which is almost twice that of crown glass3).
Patients with high levels of ametropia considering glass lenses, or those rare patients that still request conventional crown-glass lenses, should therefore be advised of the potential drawbacks in terms of weight and comfort.
Those patients that desire lightweight lens solutions may wish to consider low-density materials, such as polycarbonate or Trivex lenses, for their eyewear despite the constringence drawback mentioned earlier.
(*Though minimum centre and edge thicknesses with glass lenses may be slightly thicker than plastic from a safety
perspective.)
Summary
As with most things in life, there are always pros and cons. This article reinforces the need for critical thinking when considering the lens type to be dispensed, in order to help reduce potential patient intolerances.
The future will no doubt present new materials and designs to the optical market, and practitioners should review and familiarise themselves with the properties of such materials to inform their clinical decisions.
A patient-centred approach, together with the consideration of any negative aspects of lens materials on the patient’s expectations and lifestyle, will help maintain patient satisfaction and trust in their eye care provider.
- Mark Hickton BSc (Hons), Cert Ed, FBDO, FHEA is a dispensing optician and lecturer in ophthalmic dispensing, with over 25 years’ experience within the optical industry. He has been teaching at Bradford College for the past 15 years and is the module leader for the optics, visual optics, and ophthalmic lenses modules. His college scholarly activity revolves around the area of visual and audio-visual perception. Hickton is an ABDO Fellow and a Fellow of the Higher Education Academy.
References
- Schwartz SH. Geometrical and Visual Optics: A Clinical Introduction. 3rd ed. New York:McGraw Hill Education, 2019.
- Hecht E. Optics. 5th ed. Global edition. London: Pearson Education, 2016.
- Jalie M. The Principles of Ophthalmic Lenses. 6th ed. ABDO, London. 2021.
- Fowler C and Petre KL. Spectacle Lenses: Theory and Practice. Oxford: Butterworth-Heinemann, 2001.
- Zeiss. Ernst Abbe – Physicist, inventor, entrepreneur & social reformer. [Online]. Available: https://www.zeiss.com/corporate/en/about-zeiss/past/history/ernst-abbe.html (accessed 13 April 2024), n.d.
- Meslin D. Ophthalmic Optics Files: Materials and Treatments. Paris: Essilor, 2013.
- Carpenter R and Reddi B. Neurophysiology – A conceptual approach. 5th ed. London: CRC Press, 2012.
- Stone JV. Vision and Brain – How we perceive the world. Cambridge: Massachusetts Institute of Technology, 2012.
- Strong S. Introduction to Visual Optics – A Light Approach. Elsevier, 2022
- Elliott DB. Clinical procedures in Primary Eye Care. 5th ed. Elsevier Health Sciences, 2021.
- Brooks CW and Borish IM. System for Ophthalmic Dispensing. 3rd ed. St. Louis: Butterworth Heinemann, 2007.
