Domains and learning outcomes
C109260
• One distance learning CPD point for optometrists and dispensing opticians.
• Clinical practice
Upon completion of this CPD practitioners will be able to describe the potential positive and negative impact nutrition/nutrition related systemic diseases could have on ocular surface health (s5)
Upon completion of this CPD, practitioners will be able to identify the current knowledge gaps in the field of nutrition and ocular health (s5)
Nutrition is a modifiable factor that constitutes a fundamental part of our lifestyle, significantly impacting overall wellbeing and ocular surface health. The Tear Film & Ocular Surface Society (TFOS) conducted a comprehensive workshop titled ‘TFOS Lifestyle: Impact of Nutrition on the Ocular Surface’. The report provided an extensive review of current evidence on the nutritional impact on the ocular surface.
The aim of this article is to summarise the key points discussed in the TFOS nutrition paper and to explore the main nutritional factors that affect ocular surface health. Various aspects of this topic are discussed in the following sections.
Ocular health and nutrition factors
Impact of different diets on ocular surface health
The TFOS Nutrition report assessed the role of various diets on ocular surface health, including the Mediterranean diet and the Western diet.
Mediterranean diet
The TFOS nutrition review suggested a possible positive impact of the Mediterranean diet on ocular surface health. This diet is rich in monounsaturated fats and low in saturated fats, emphasising high consumption of olive oil, legumes, unrefined cereals, fruits and vegetables.
It also includes moderate to high consumption of fish, moderate consumption of dairy products (mainly cheese and yogurt), moderate wine consumption, and low consumption of red and processed meat and sugar.
Because of its antioxidant and anti-inflammatory properties, the Mediterranean diet has been reported to be beneficial in chronic inflammatory diseases. Therefore, it can potentially offer benefits in treating inflammatory diseases of the ocular surface, such as dry eye disease.
Additionally, the Mediterranean diet has been linked to a reduced risk of developing primary Sjögren’s syndrome. In a randomised study of participants with ocular discomfort, those on a calorie-restricted Mediterranean diet combined with physical activity showed greater improvements in dry eye symptoms after six months compared to those on a standard Mediterranean diet.
Western diet
The TFOS report highlighted the possible negative impact of the Western diet on ocular health. This diet is characterised by high-fat and high-sugar content and is associated with obesity and systemic low-grade inflammation.
It has been suggested that a high-fat diet is linked to the incidence of meibomian gland dysfunction (MGD), pathophysiological changes and functional decompensation of the lacrimal gland in mice models.
Other diets
The TFOS report also reviewed other diets, including African diets, Asian diets, intermittent fasting, vegetarianism, kosher and halal diets, and the Paleolithic (Paleo) diet.
However, these diets had no or limited studies suggesting their effects on ocular surface health. Further research is needed to examine the impact of these diets on the ocular surface.
Hydration and ocular surface health
Water has been recommended to improve dry eye symptoms. While hydration is critical for general health, its role in ocular surface health is not fully established. Some studies suggest a connection between plasma osmolarity and ocular osmolarity, as well as dry eye disease signs.
However, more longitudinal studies are needed to confirm these findings and better understand the relationship between hydration and ocular surface health.
Dietary supplements and ocular surface health
Omega-3 and 6
Omega-3 (n-3) and omega-6 (n-6) are polyunsaturated fatty acids. Both are essential for the body and must be consumed in the diet as the human body is incapable of producing them. They can be obtained from food or commercial supplements.
Fish, seafood, and seeds such as flaxseeds and chia seeds are sources of omega-3. Omega-6 can be found in vegetable oils such as corn, soybean and sunflower oil. Omega-3 has an anti-inflammatory role, which means it can help reduce inflammation in the body, while omega-6 has a pro-inflammatory role, which means it can help the body fight infections and harmful pathogens by promoting inflammation.
However, high levels of omega-6 in the long term can lead to chronic inflammatory diseases. Balancing pro-inflammatory and anti-inflammatory responses is crucial for maintaining health, therefore, a balanced ratio of omega-3 to omega-6 in the diet is important to prevent low-grade inflammation in the body.
Omega-3 and omega-6 supplements are the most investigated supplements for ocular surface health, particularly in relation to dry eye disease. The TFOS Nutrition report assessed meta-analyses, systematic reviews and individual clinical trials in this regard.
Although the outcomes of these reviews sometimes differ or conflict, overall, there is enough evidence to draw a conclusive conclusion about the positive impact of omega-3 supplements on ocular health, reducing the prevalence of dry eye disease and helping manage dry eye and meibomian gland dysfunction (MGD).
In dry eye disease, omega-3 supplements can improve symptoms, corneal fluorescein staining, tear stability and volume as measured by tear breakup time and the Schirmer test. Omega-3 can positively impact modulating peripheral nerve and corneal nerve features such as branch density and length. Omega-3 can also reduce the level of inflammatory mediators in tears.
Another condition that can benefit from omega-3 supplementation is allergic conjunctivitis. Omega-3 is a relatively safe supplement but may potentially reduce platelet activity. The Food and Drug Administration of the USA recommends a daily intake of omega-3 of 500mg/day, with no more than 3,000mg, and a maximum of 2,000mg from supplements.
Vitamins
Vitamins are essential for the maintenance of human health, playing a crucial role in supporting ocular surface health and preventing significant eye disorders. In this section, we discuss the vitamins with evidence of their impact on ocular health. The primary vitamins linked to ocular surface diseases are vitamins A, B12, C, and D.
Vitamin A
Vitamin A is known to have a significant influence on the ocular surface. A deficiency in vitamin A has been reported to cause various ocular surface changes, such as decreased or absent goblet cells, xerophthalmia and corneal punctate keratopathy.
Long-term vitamin A deficiency can lead to epithelial metaplasia and keratinisation, resulting in conditions like xerophthalmia, Bitot’s spots, keratomalacia and even corneal perforation.
Vitamin B12
Vitamin B12, found in food sources such as meat, fish and dairy products, is essential for DNA synthesis, fatty acid and amino acid metabolism. It plays a significant role in immune defence by regulating white blood cells and is crucial for a healthy nervous system. Vitamin B12 deficiency is associated with myelopathy, peripheral neuropathy and optic atrophy.
Vitamin C
Fruits and vegetables are the best sources of vitamin C, which acts as an antioxidant and regenerates other antioxidants, including vitamin E. It plays an essential role in the biosynthesis of collagen, L-carnitine and protein metabolism. Vitamin C has been found in tears and is suggested to provide antioxidant defence and aid in corneal healing after injury.
Vitamin D
Vitamin D is crucial for eye health and essential for calcium homeostasis and cellular functions. It can be obtained from food and synthesised in the skin upon sunlight exposure. Vitamin D levels are higher in tears than in serum.
Deficiency in vitamin D is linked to dry eye disease, specifically causing conjunctival squamous metaplasia and the loss of conjunctival goblet cells. Also, vitamin D modulates systemic calcium absorption, promoting fluid secretion in salivary and lacrimal glands.
Furthermore, serum vitamin D levels correlate with tear production, tear stability and dry eye symptoms.
Minerals
Among the minerals, selenium and lactoferrin have the most important roles in ocular surface health.
Selenium
Selenium is crucial for preventing oxidative damage in the eye. It can be found in foods such as Brazil nuts, meat, fish, seafood, and cereals. Low levels of selenium are linked to dry eye disease.
Lactoferrin
Lactoferrin is an iron-binding glycoprotein found in milk, saliva and tears. It supports ocular health through its anti-inflammatory, antioxidant and antimicrobial properties. Lower levels of tear lactoferrin are associated with dry eye disease and chronic meibomitis.
Other Minerals: Zinc and Copper
Other minerals, including zinc and copper, are involved in antioxidant activity and connective tissue metabolism, influencing oxidative stress, collagen synthesis and breakdown.
These minerals may play a role in the pathogenesis of keratoconus, as lower serum levels of these trace elements have been observed in individuals with the condition compared to healthy individuals.
However, further research is needed to explore the potential therapeutic roles of these minerals in slowing the progression of keratoconus.
Honey
Several randomised clinical trials have suggested the possible positive effects of topically applied Manuka honey (Leptospermum spp) in and around the eye.
These benefits include improvements in tear film evaporation, meibomian gland dysfunction (MGD), blepharitis, eyelid wound healing, corneal ulcers and vernal conjunctivitis. However, the role of oral honey in the management of ocular surface disease is not well established.
Caffeine
Studies suggest that the consumption of caffeine may have beneficial effects on tear production and dry eye symptoms, potentially reducing the prevalence of dry eye disease. It is also suggested that caffeine intake may reduce corneal deformability and increase intraocular pressure, which should be considered when diagnosing and managing corneal disorders. Further long-term investigations are necessary to establish caffeine effects on ocular health conclusively.
Herbs
It has been suggested that using Chinese herbs can improve dry eye disease by enhancing ocular staining and tear stability and reducing inflammatory mediators in the tear film.
However, more studies are needed to provide stronger evidence, using appropriate clinical study designs and different herbal combinations, to draw conclusive conclusions.
Spices
Research on the potential benefits of spices for ocular surface disease has primarily concentrated on curcumin, the principal curcuminoid of turmeric, a plant from the ginger family. Animal and laboratory studies have demonstrated the positive effects of curcumin on preventing corneal neovascularisation, promoting corneal wound healing, and preventing allergic conjunctivitis, pterygium and corneal endothelial dysfunction.
Curcumin has also been suggested to improve dry eye symptoms and signs, including increased tear volume, improved tear breakup time, reduced tear inflammatory markers and enhancements in conditions such as Sjögren’s syndrome and systemic lupus erythematosus. However, further investigations are needed to confirm its role in these conditions.
Impact of excipients, additives and non-nutritional components in food
Food excipients are substances with no bioactivity themselves but are added to enhance the bioactivity of co-ingested active ingredients. Understanding the types and sources of additives and contaminants in processed foods is essential for recognising their potential health impacts, including those on ocular surface health.
Although there is a lack of studies specifically examining different types of excipients and their impacts on ocular surface health, some have been investigated in relation to ocular diseases and suggested to have negative effects. Endocrine-disrupting chemicals (EDCs) are a form of excipients with negative impacts on ocular surface.
Endocrine-disrupting chemicals
EDCs can interfere with hormone receptors, synthesis, secretion, or transport, potentially affecting the actions of various hormones, including sex hormones, which are crucial for ocular surface health.
These compounds are primarily introduced into the body through pesticides in the food chain, leaching from food containers and contamination during food manufacturing or processing. EDCs can also alter gut microbiome diversity, potentially affecting overall health, including ocular health.
Bisphenol-A (BPA)
BPA is a common EDC used in the production of plastics, including food and drink containers, and can bind to estrogen receptors in the body. It has been suggested that BPA may exacerbate conditions like primary Sjögren’s syndrome and has positive correlations with dry eye disease signs.
Mercury
Mercury is another EDC with negative impacts on the ocular surface. This heavy metal is extremely toxic even in small amounts, causing teratogenic, neurotoxic and immunotoxin effects.
Most commonly introduced through mercury-contaminated seafood, studies suggest mercury can increase dry eye symptoms, tear osmolarity, alter tear cytokine levels, corneal sensitivity, and disrupt sub basal corneal nerve morphology. Environmental exposure to lead and mercury has also been linked to the development of pterygium.
Gut microbiome and ocular surface health
The human microbiota comprises all organisms inhabiting the human body and significantly impacts human health and disease. The gut microbiota can be affected by various factors such as environment, diet, genes, disease and nutrition. The gut microbiota influences gut motility, energy extraction, epithelial integrity and mucosal immunity through signalling molecules. These effects extend to various organs, including the brain, skin and ocular surface. Maintaining a healthy balance of gut microbiota is crucial for overall health.
Factors such as antibiotics, artificial sweeteners, vitamin deficiency, cigarette smoke and saturated (versus polyunsaturated) fats can alter the healthy composition of gut microbiota, leading to various chronic diseases.
Impact of Nutrition Factors on Gut Microbiota
Diet
The Western diet, characterised by high energy intake and low fibre, negatively impacts the gut microbiome, contributing to many chronic and inflammatory diseases. In contrast, diets high in fibre, such as the Mediterranean diet, can regulate the gut microbiome.
Alcohol
Alcohol negatively impacts the gut microbiota, adversely altering its diversity. It can also lead to increased production of inflammatory cytokines. However, some studies suggest that certain fermented forms of alcohol, such as beer and wine, may benefit the gut microbiome by enhancing its diversity due to their prebiotics and polyphenols. Distilled alcohols, such as gin and vodka, which have higher alcohol content, do not share these benefits.
Food preparation
Diet includes food production, preparation, preservation and storage. These processes significantly impact the food’s nutritional value when it reaches the table. Changes in soil through soil transfer or fertilisers, herbicides, fungicides and pesticides can disrupt both soil and plant microbiomes, affecting the human gut microbiome and health.
Additives for preserving food shape, flavour and freshness, along with edible nanoparticles used to coat food for shelf-life preservation and inhibition of organic spoilage, can disrupt gut microbiota integrity, leading to gut dysbiosis, which consequently results in immunogenic reactions and chronic inflammatory diseases.
Food refrigeration may enable the overgrowth of pathogenic bacteria that can flourish between -1°C and 10°C, and increased hygiene practices, such as automated dishwashing, can reduce the chance of microbial exposure for gut health in young children, increasing the risk of chronic inflammatory diseases like Crohn’s disease in adulthood.
Other lifestyle factors, such as a sedentary lifestyle and smoking, can negatively impact the gut microbiome, causing gut dysbiosis and increasing systemic inflammation, potentially affecting ocular surface health.
The gut microbiome and ocular surface disease
Gut dysbiosis has been associated with many ocular diseases, such as uveitis, age-related macular degeneration, glaucoma, chalazion, keratitis, and dry eye disease. Although the impact of the gut microbiome on the ocular surface requires further investigation, evidence regarding the role of the gut microbiome in other ocular surface disorders, except dry eye disease, is still limited.
Gut dysbiosis has been reported in dry eye disease, with a correlation between the level of dysbiosis and the severity of dry eye, especially in individuals with Sjögren’s syndrome.
Based on this evidence, modulation of the gut microbiome could be a novel approach for managing inflammatory eye diseases. Here are five main approaches to regulate the gut microbiome:
- Antibiotics: Targeting harmful bacteria with specific antibiotics.
- Probiotics: Beneficial live bacteria that can improve health when consumed in adequate amounts.
- Prebiotics: Dietary fibres that are not digestible by humans but support beneficial bacteria.
- Postbiotics: Non-living bacterial byproducts that provide health benefits by delivering beneficial compounds directly.
- Faecal microbial transplant (FMT): Replacing the entire gut microbiome population with that from a healthy donor.
A few animal model studies suggested the positive effects of postbiotics and faecal transplantation on dry eye disease and Sjögren’s syndrome. Prebiotics and probiotics are more well-studied. Prebiotics can improve tear stability measured by tear breakup time.
Probiotics have been suggested to improve symptoms and clinical signs of redness, chemosis and itching in allergic conjunctivitis, rhinoconjunctivitis and manifestations in children with cow’s milk allergy.
Clinical trials using probiotics combined with prebiotics have shown improvements in dry eye symptoms and some clinical signs, including tear stability and secretion.
All studies used IRT5 probiotics, which combine five known probiotic species: Lactobacillus casei, Lactobacillus acidophilus, Lactobacillus reuteri, Bifidobacterium bifidum, and Streptococcus thermophilus. Larger, randomised controlled clinical trials are necessary to establish the safety and efficacy of these treatments for ocular surface diseases.
Other dietary supplements such as vitamins, selenium, lactoferrin, curcumin and flavonoids has been shown to improve gut health by regulating the gut microbiome. Oral vitamin D supplementation has been shown to increase gut microbiota diversity and improve dry eye disease symptoms. However, no studies have directly correlated gut microbiome changes with these improvements.
Overall, modulating the gut microbiome through dietary changes as a treatment for ocular surface disease is a relatively new area of study and more investigations are needed to fully understand this relationship.
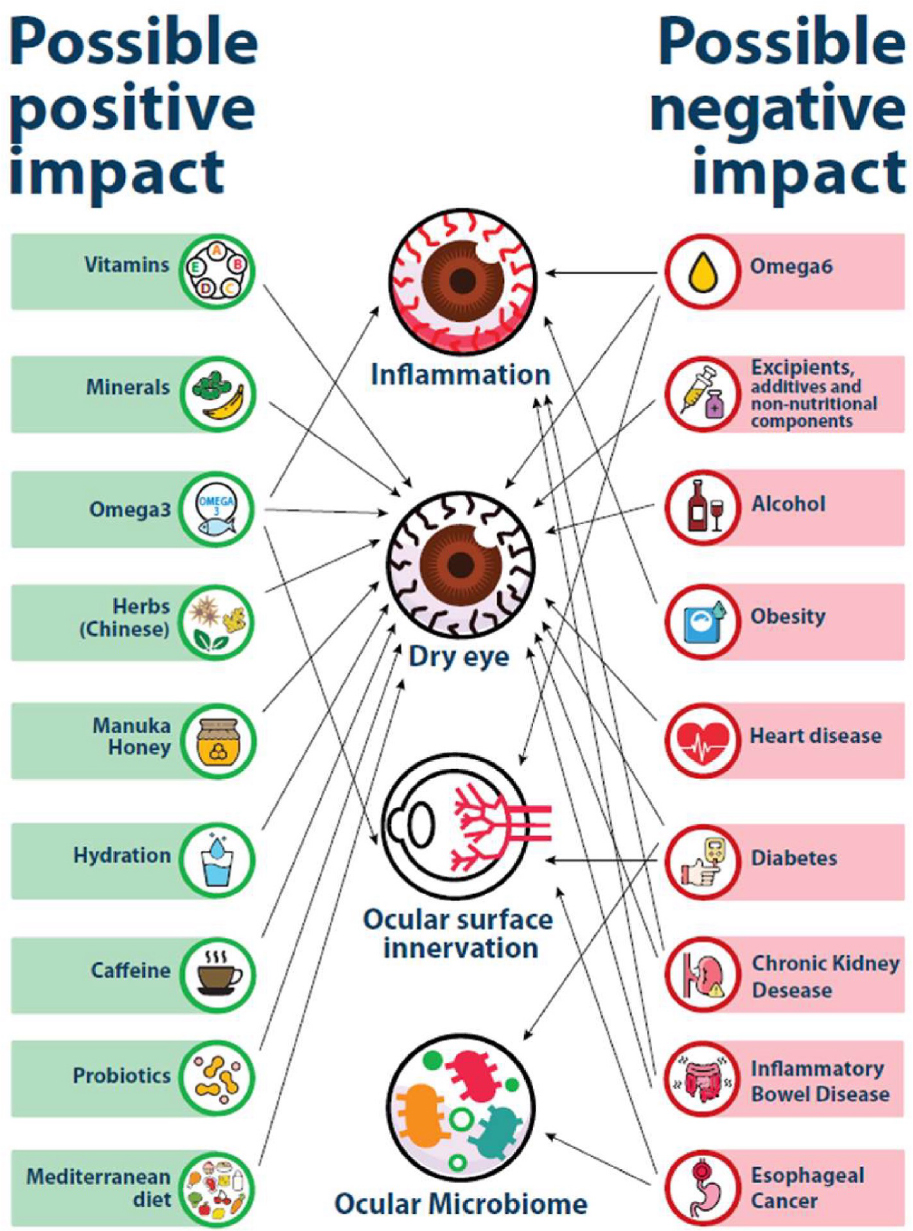
Figure 1: Impact of nutrition on the ocular surface. Summary of the possible positive and negative impacts on the ocular surface. (Figure adapted from Markoulli M, Ahmad S, Arcot J, Arita R, Benitez-del-Castillo J, Caffery B, Downie LE, Edwards K, Flanagan J, Labetoulle M, Misra SL. TFOS Lifestyle: impact of nutrition on the ocular surface. The Ocular Surface. 2023 Jul 1;29:226-71.)
Systemic diseases influenced by nutrition and their impact on the ocular surface
Metabolic disorders
Obesity
Obesity is associated with various eye conditions, including cataracts, age-related maculopathy, diabetic retinopathy, glaucoma, and ocular surface diseases such as floppy eyelid syndrome, blepharoptosis (ptosis) and dry eye disease.
Bariatric surgery, a common weight-loss procedure, can lead to significant nutrient deficiencies, particularly in vitamins A, E, B1 and copper, which can adversely affect ocular surface health.
Vitamin A deficiency is especially prevalent post-surgery and has been reported to cause various ocular complications such as dryness and night vision changes. It is essential to monitor ocular health post-surgery and ensure adequate nutrient supplementation, potentially via parenteral routes, to prevent serious eye conditions.
Dyslipidemia and hypertension
Nutrition is closely linked with systemic diseases such as hypertension, hyperglycemia and hypercholesterolemia. Hypertension has been associated with ocular diseases like dry eye and meibomian gland dysfunction, although further research is needed to establish this connection.
Metabolic syndrome can present with signs and symptoms of dry eye and is associated with peripheral neuropathy and reduced corneal nerve parameters. Artificial sweeteners can alter the gut microbiome, cause glucose intolerance, weight gain and induce metabolic syndrome.
Pre-diabetes and type 2 diabetes
Type 2 diabetes can affect the entire eye, leading to severe complications such as diabetic retinopathy, an increased risk of dry eye disease, meibomian gland dysfunction, Demodex folliculorum, microvascular abnormalities in the conjunctiva, increased limbal and bulbar hyperaemia and conjunctivitis.
Diabetic patients often experience lower corneal sensitivity, potentially reducing blink rates, and eyelid abnormalities are also correlated with type 2 diabetes. Changes in meibum lipid composition, gland dropout, lid margin abnormalities and gland structure alterations are common in diabetic patients.
Diabetic peripheral neuropathy can be the primary cause of lacrimal gland disruption, leading to reduced basal tear production in people with diabetes and dry eye disease. It has been suggested that the ocular surface microbiome is altered in type 2 diabetes, making the eye more prone to bacterial and fungal infections and potentially resulting in different responses to antibiotics.
Furthermore, corneal sensitivity is correlated with corneal nerve function in patients with type 1 and type 2 diabetes. The corneal sensitivity threshold has been shown to be reduced in these patients.
Diabetics exhibit reduced corneal nerve features, including nerve fibre density, nerve fibre length, nerve beading density and inferior whorl length. Subclinical alterations in the corneal nerve plexus are linked to diabetic peripheral neuropathy, indicating that corneal confocal microscopy could play a role in the early detection and timely treatment of neuropathy in at-risk patients.
Cardiovascular disease
Cardiovascular diseases, influenced by various nutritional factors, can lead to acute myocardial infarction and microcirculation dysfunction. These disorders are associated with dry eye disease and changes in conjunctival microcirculation.
Chronic kidney disease (CKD)
CKD, often resulting from diabetes, hypertension and glomerulonephritis, is linked with severe signs and symptoms of dry eye disease. Studies have shown that corneal nerve loss is significantly greater in individuals with both type 2 diabetes and CKD compared to those with diabetes alone.
CKD-related changes in tear protein expression, involving lipid metabolism, inflammation and immune response, may contribute to the signs and symptoms of dry eye disease.
Gastrointestinal disease
Chronic gastrointestinal diseases can lead to malnutrition, further impairing the gut’s ability to digest and absorb nutrients. Conditions such as stomach ulcers, inflammatory bowel disease, Crohn’s disease, ulcerative colitis, celiac disease, lactose intolerance and diverticulosis have been linked to dry eye.
Cancer
Many cancers, especially those affecting the gastrointestinal tract like oesophageal cancer, are highly associated with nutrition. Although metastasis to the eye is rare, reports include eyelid tumours, iris, scleral and orbital metastases.
Ocular infections like panophthalmitis and endophthalmitis have been reported in cancer patients, associated with Clostridium septicum and Candida albicans, respectively. Increased infection risk and reduced corneal nerve fibre length, density and branch density, along with changes in tear protein composition, have been observed in cancer patients, likely due to systemic peripheral neuropathy associated with cancer.
The impact of cancer on the ocular surface may be overshadowed by the side effects of chemotherapy. It is important for eye care practitioners to consider systemic diseases in their assessments.
Effects of intentional food restriction
The TFOS Lifestyle conducted a systematic review on the effects of intentional food restriction on the ocular surface, including 25 studies. These studies included Ramadan fasting (56%), bariatric surgery (16%), and anorexia nervosa (16%).
The primary outcome measured was changes in dry eye symptom scores, using questionnaires or visual analogue scales. Secondary outcomes included tear breakup time, tear osmolarity, meibomian gland atrophy, anterior blepharitis, corneal staining scores, Schirmer scores, conjunctival hyperaemia, quality of life and incidence of ocular adverse events.
While some suggestions indicate negative impacts from anorexia nervosa and bariatric surgery, the poor quality of studies and lack of clinical trials prevent drawing conclusive conclusions on the effects of these factors on ocular surface health.
Conclusion
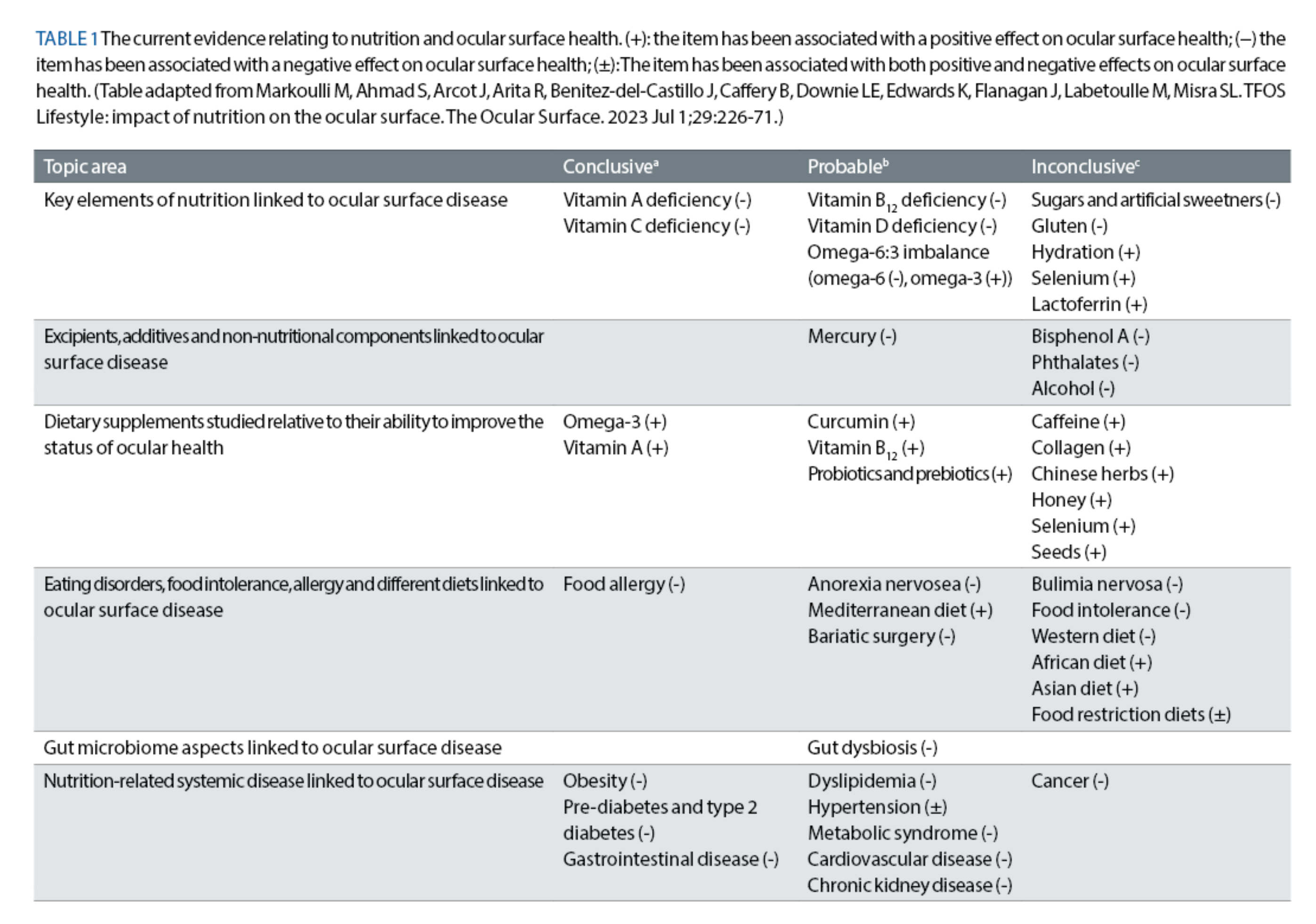
Figure 1 illustrates the possible positive and negative factors that have the most evidence from the literature impacting ocular surface health. Table 1 indicates the certainty of the impact of these factors on the ocular surface.
Nutrition is crucial for maintaining overall health and plays a significant role in the health of the ocular surface. While the understanding of nutrition’s impact on all aspects of ocular surface health is still developing, advances are being made.
As eye care professionals, we should carefully review the available evidence before making nutritional recommendations for the ocular surface health of our patients.
It is also important for clinicians to consider the general dietary habits of their patients, particularly in conditions such as severe dry eye disease, and to collaborate with dietitians to develop more effective management plans.
- Dr Azadeh Tavakoli is an optometrist and postdoctoral research associate at the School of Optometry and Vision Science at UNSW. Her research interests lie within the impact of nutritional factors on ocular surface health and disease, specifically dry eye disease.
- Sarah Farrant is a director at Earlam and Christopher Optometrists, an optometrist and dry eye specialist and acts as a consultant and key opinion leader for a number of national and global companies. Farrant has a great passion for her work, which is reflected in the wide variety of different interests she has within the profession. She has undertaken a number of additional qualifications and is a leading national expert in therapeutics and dry eye management and represents the UK as an Ambassador for TFOS. She is currently president of the BCLA and sat for 12 years on the executive and council boards for the College of Optometrists. She has been instrumental in a number of local and national initiatives to improve access to education amongst the profession and access to eye care for patients. She is also a keen lecturer and regularly teaches other optometrists both nationally and internationally.
Further Information
Further information can be accessed at tearfilm.org: Markoulli M, Ahmad S, Arcot J, Arita R, Benitez-del-Castillo J, Caffery B, Downie LE, Edwards K, Flanagan J, Labetoulle M, Misra SL. TFOS Lifestyle: impact of nutrition on the ocular surface. The Ocular Surface. 2023 Jul 1;29:226-71.
Acknowledgements
Maria Markoulli, Sumayya Ahmad, Jayashree Arcot, Reiko Arita, Jose Benitez-Del-Castillo, Barbara Caffery, Laura E Downie, Katie Edwards, Judith Flanagan, Marc Labetoulle, Stuti L Misra, Malgorzata Mrugacz, Sumeer Singh , John Sheppard, Jelle Vehof , Piera Versura , Mark D P Willcox, Jillian Ziemanski, James S Wolffsohn
