Domains and learning outcomes (C109769)
• One distance learning CPD point for optometrists and dispensing opticians.
• Clinical practice
Upon completion of this CPD, ECPs will be able to describe the physiological mechanisms underlying digital eye strain (s5)
Upon completion of this CPD, ECPs will be able to describe and, depending on their scope of practice, provide effective patient care and/or treatments for digital eye strain (s7)
The TFOS Lifestyle: Impact of the digital environment on the ocular surface report1 investigates the ocular effects associated with digital environments. The technological revolution has reshaped our lives, offering unparalleled communication, information accessibility and mobility. Unlike the past, when computing technology was confined to mainframes accessible to a select few, handheld devices are now used by most of the global population. Consequently, everyday tasks have undergone significant transformation, posing unique challenges to ocular health in the digital era.
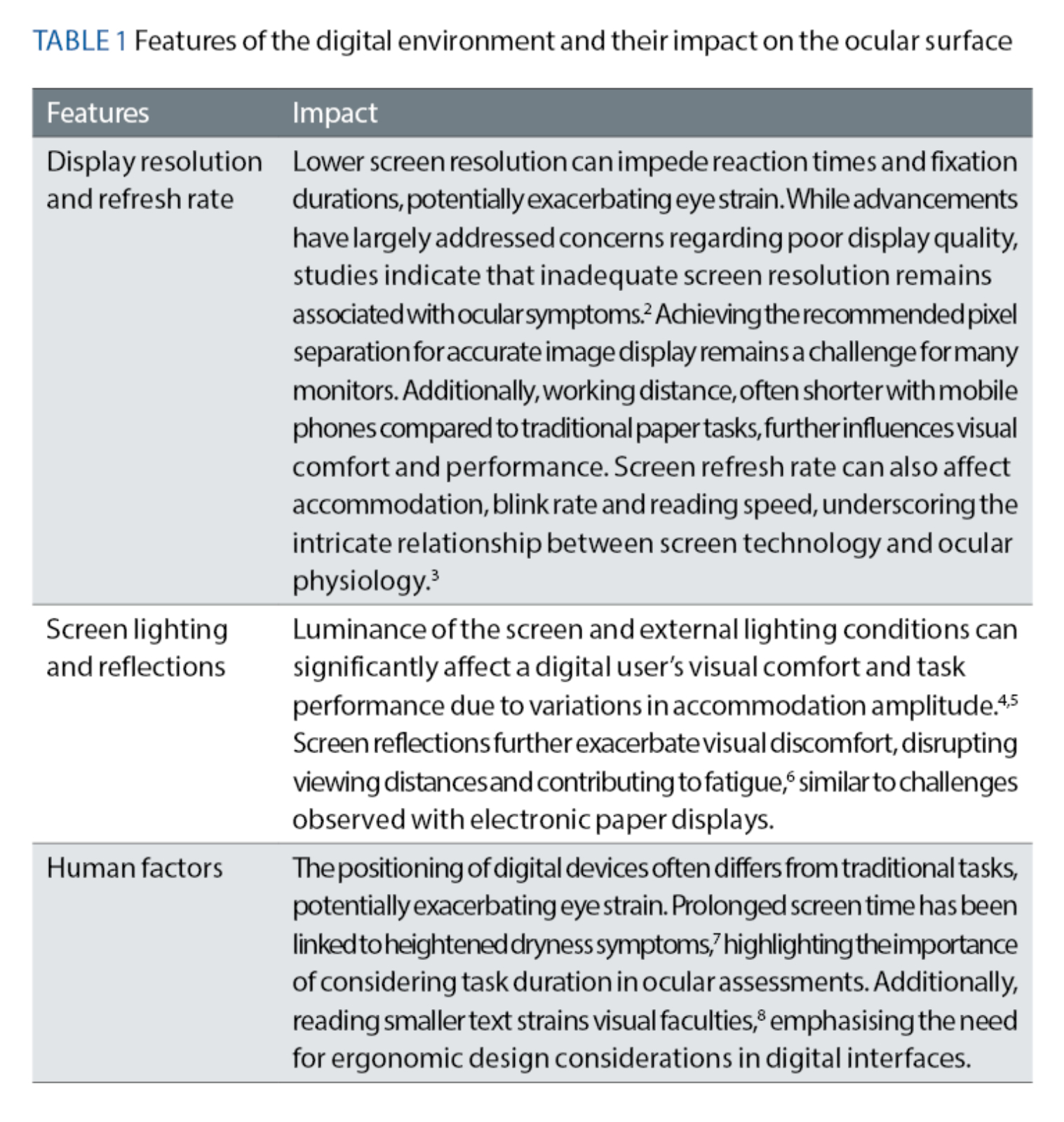
Features of our digital world
The report starts by exploring the distinct features of the digital environment, summarised in table 1. By recognising their impact on visual comfort, eye care professionals (ECPs) can devise tailored strategies to mitigate digital eye strain and optimise patient ocular health.
The global landscape
The prevalence of digital eye strain varies widely across geographical regions, reflecting the complex interplay of cultural, technological and environmental factors. While the global prevalence is estimated to be 70.7%, rates fluctuate significantly across populations, ranging from 31.9% in Italian bank workers to a staggering 97.3% among Saudi Arabian university students. These disparities highlight the multifaceted nature of digital eye strain as well as the urgent need for standardised diagnostic criteria to facilitate meaningful cross-country comparisons.
The Computer Vision Syndrome Questionnaire (CVS-Q) emerges as the most widely used diagnostic tool for digital eye strain, as it has been validated and specifically tailored to this condition.9 Despite its widespread adoption, interpretations of CVS-Q scores warrant some caution due to symptom overlap with dry eye disease and other ocular pathologies.
Moreover, epidemiological studies often fail to account for confounding variables such as age, contact lens wear, systemic comorbidities and environmental factors, as well as population sample limitations and cultural or linguistic differences, which all can hinder accurate epidemiological assessments.
Challenges and recommendations
Standardisation of diagnostic criteria and limiting any confounding factors are important to increase the reliability of epidemiological studies. By proposing a unified definition and diagnostic criteria for digital eye strain, the authors of the report believe that more meaningful cross-country comparisons can be made as well as informed targeted interventions to mitigate the global burden of digital eye strain.
This would also improve our understanding of the complex interplay of cultural, technological and environmental factors shaping its prevalence. Ultimately, through concerted efforts, ECPs globally can use this unified approach to optimise ocular health outcomes in an increasingly digitalised world.
The diagnostic challenge
Digital eye strain, defined as the development or exacerbation of ocular signs and symptoms specific to digital device viewing, is characterised by a complex interplay of symptoms, signs and technological nuances.
However, it is not always clear whether symptoms, including a spectrum of manifestations such as discomfort, dryness, irritation, blurred vision, sensitivity to light, and headaches, are a direct result of digital tasks or non-digital activities.
As such, only when observing a increase in symptoms and/or signs when the digital device(s) are used warrants a differential diagnosis of digital eye strain.1
Diagnostic tools
The diagnostic journey for digital eye strain is challenging, particularly due to its overlap with dry eye disease. It is important to note that the impact of digital devices on dry eye signs and symptoms can differ in the same individual conducting similar tasks.10 A validated questionnaire like CVS-Q offers valuable insights into symptom frequency and severity, but has its limitations as described previously.
Additionally, objective measures such as visual acuity and refractive error, while informative, lack definitive cut-off values or algorithms for diagnostic purposes. Previous attempts to incorporate other clinical signs generated ambiguous outcomes, with parameters like contrast sensitivity, reading performance, discomfort and disability glare, oculomotor functions accommodation facility, critical flicker fusion frequency and multifocal electroretinogram abnormalities all failing to objectively measure eyestrain.
While these measures may provide insights into the impact of digital device use on visual function, there are mixed findings regarding their association with digital eye strain symptoms. For example, blink rate has shown to decrease with digital tasks, although this also seems the case in a similar cognitive intensity paper task.11
For now, to diagnose digital eye strain, the patient must report the development or exacerbation of ocular symptoms (and possibly signs such as slower focusing) related specifically to digital device use.
However, until robust diagnostic algorithms emerge, clinicians should consider a patient-centred approach and exercise caution in attributing ocular symptoms solely to digital device use.
Mechanisms of action
The symptoms of digital eye strain can be broadly divided into those related to ocular surface changes and those associated with visual and accommodative changes:
- Ocular surface changes include dryness symptoms, reduced tear film stability, meibomian gland dysfunction, alterations in tear film lipid and mucin layers, corneal and conjunctival staining, tear hyperosmolarity and increased inflammatory markers.
- Visual symptoms include blurred vision, diplopia, eye strain, sensitivity to light, discomfort, fatigue, tiredness and weakness of the eyes. These symptoms can be exacerbated by prolonged use of digital devices, with studies showing an increased risk of developing digital eye strain symptoms after four to five hours of daily use.
The physiological mechanisms implicated in the development of digital eye strain include blinking abnormalities, reduced tear production, tear film instability, alterations in the tear lipid and mucin layers, and inflammation (figure 1). Reduced blink rate and incomplete blinking during digital device use can lead to tear film instability and dryness symptoms.
Figure 1: Physiological mechanisms of digital eye strain

Other factors such as high cognitive and visual demands, small font sizes, low contrast and increased glare contribute to ocular surface alterations and visual discomfort.
Accommodative and oculomotor alterations also play a role in digital eye strain, with symptoms such as blurred vision, focusing difficulties, asthenopia and headache being associated with reduced binocular accommodative facility, insufficient convergence and reading at a short distance.
Furthermore, the report addresses the relationship between digital device use and refractive development, particularly myopia. While some studies suggest a weak association between digital screen time and myopia development, others report mixed findings.
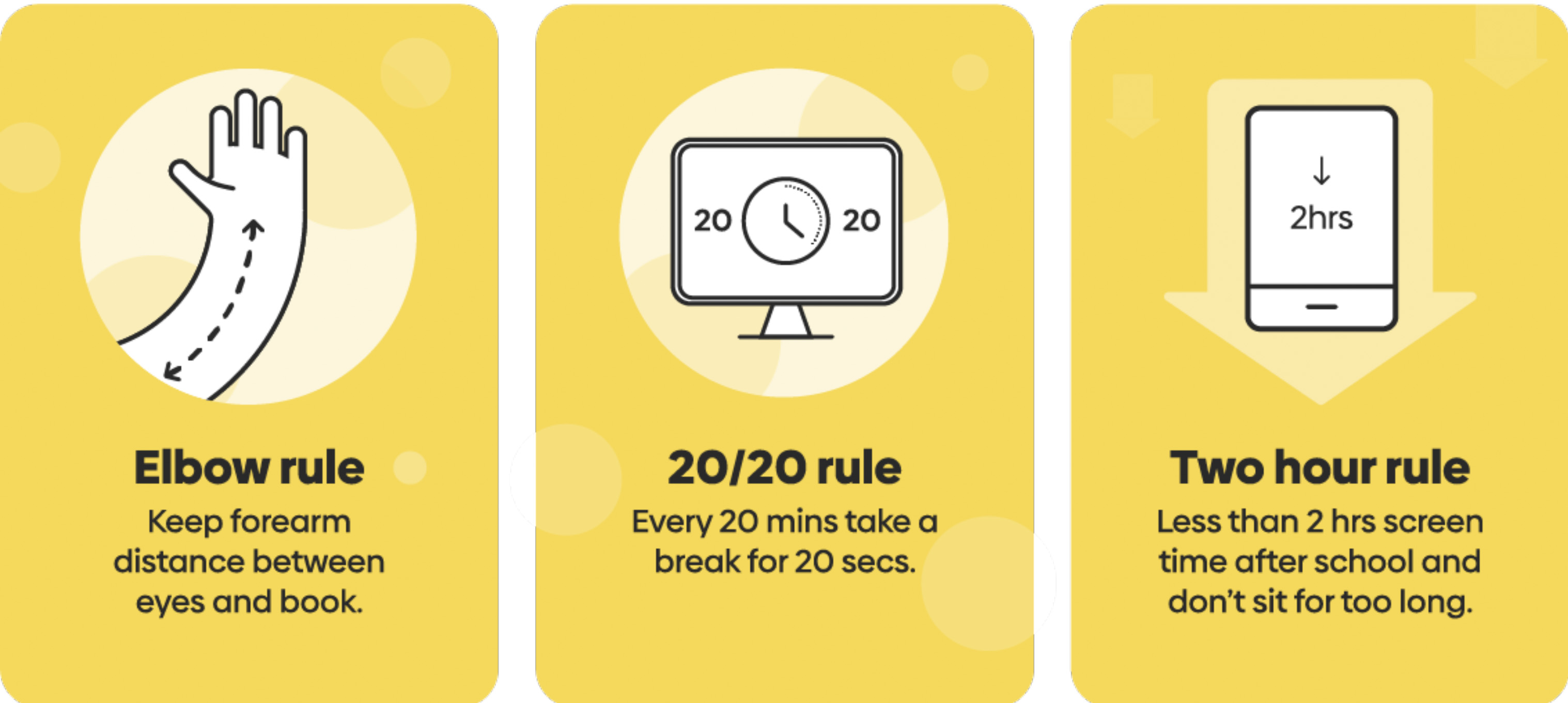
Factors such as increased near-vision work, reduced time spent outdoors and accommodative instability may contribute to myopic risk associated with digital device use, especially handheld devices. Screen time guidelines for children can serve as a valuable tool for clinicians to effectively communicate with parents and guide them on managing their child’s digital device usage (figure 2).
Figure 2: Three easy rules for indoor time to support children’s vision12
Understanding the impact
The emergence of new technologies, enhanced computational capabilities and faster internet speeds have undoubtedly boosted productivity in various fields.
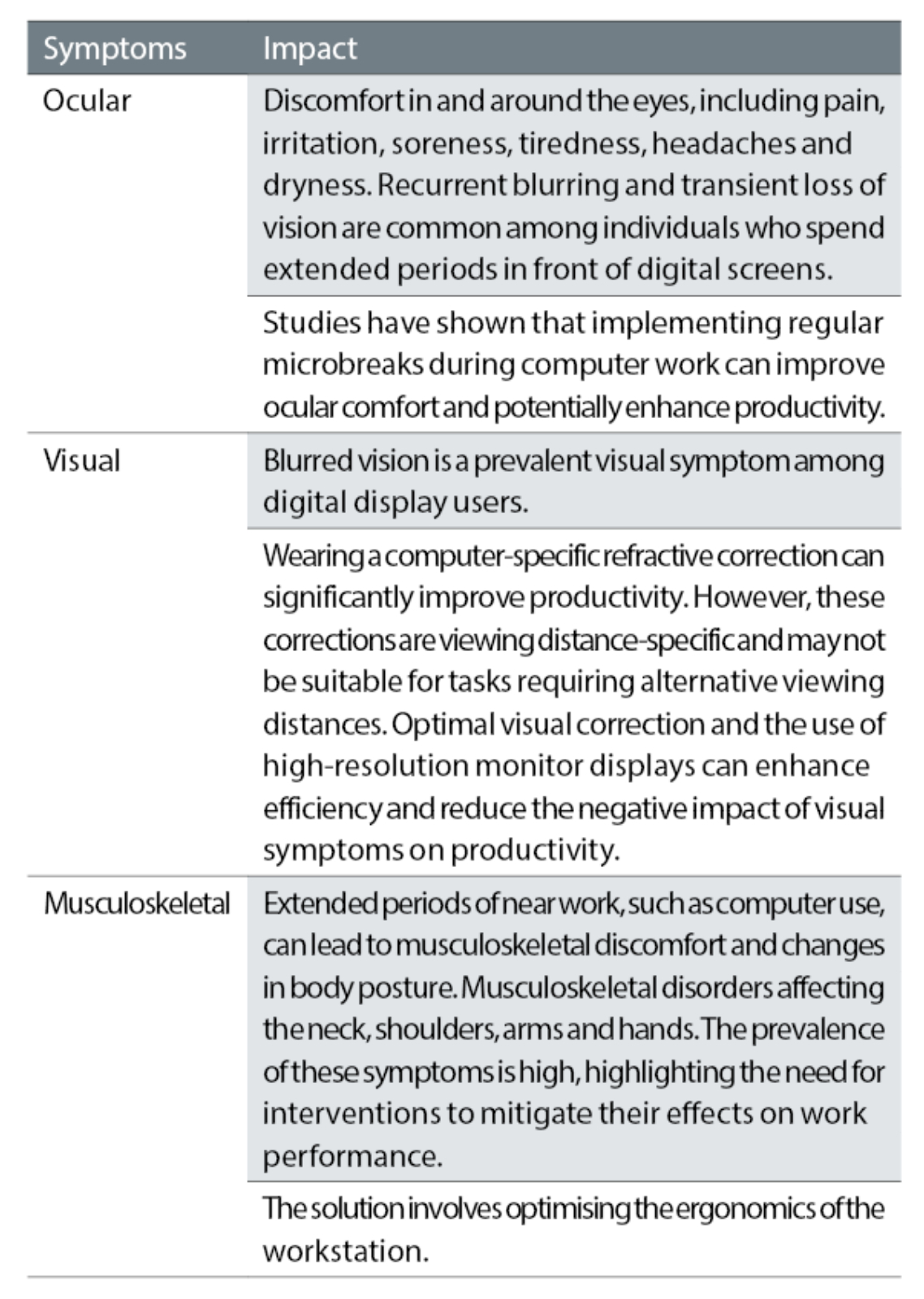
However, along with these advancements comes the prevalence of digital eye strain, which has been linked to lower quality of life and reduced work productivity, with significant economic implications. Individuals experiencing digital eye strain may encounter delays in completing digital tasks, an increase in errors, or the need for more frequent breaks.13 The symptoms associated with digital eye strain can be categorised into ocular, visual and musculoskeletal symptoms (table 2).
Table 2: Associated symptoms of digital eye strain and their impact
Quality of life
While digital engagement can positively influence the quality of life for older individuals, the impact of digital eye strain on overall quality of life remains understudied. However, research suggests that digital eye strain can have a small but significant impact on quality of life, particularly concerning ocular and physical symptoms.14 Dry eye disease, a condition often associated with digital eye strain, has been shown to have adverse effects on physical and mental health, sleep, mood and functional visual acuity.
Management of digital eye strain
Figure 3 shows the ideal workflow for the ECP. Once digital eye strain has been diagnosed through ocular symptoms and clinical assessment, a decision must be made on intervention options, based on the level of current clinical and scientific evidence. Addressing digital eye strain requires a multifaceted approach, encompassing various interventions tailored to individual needs. From rest breaks to ergonomic adjustments, each strategy plays a crucial role in alleviating symptoms and improving overall ocular health.
Figure 3: Workflow for the management of dry eye1
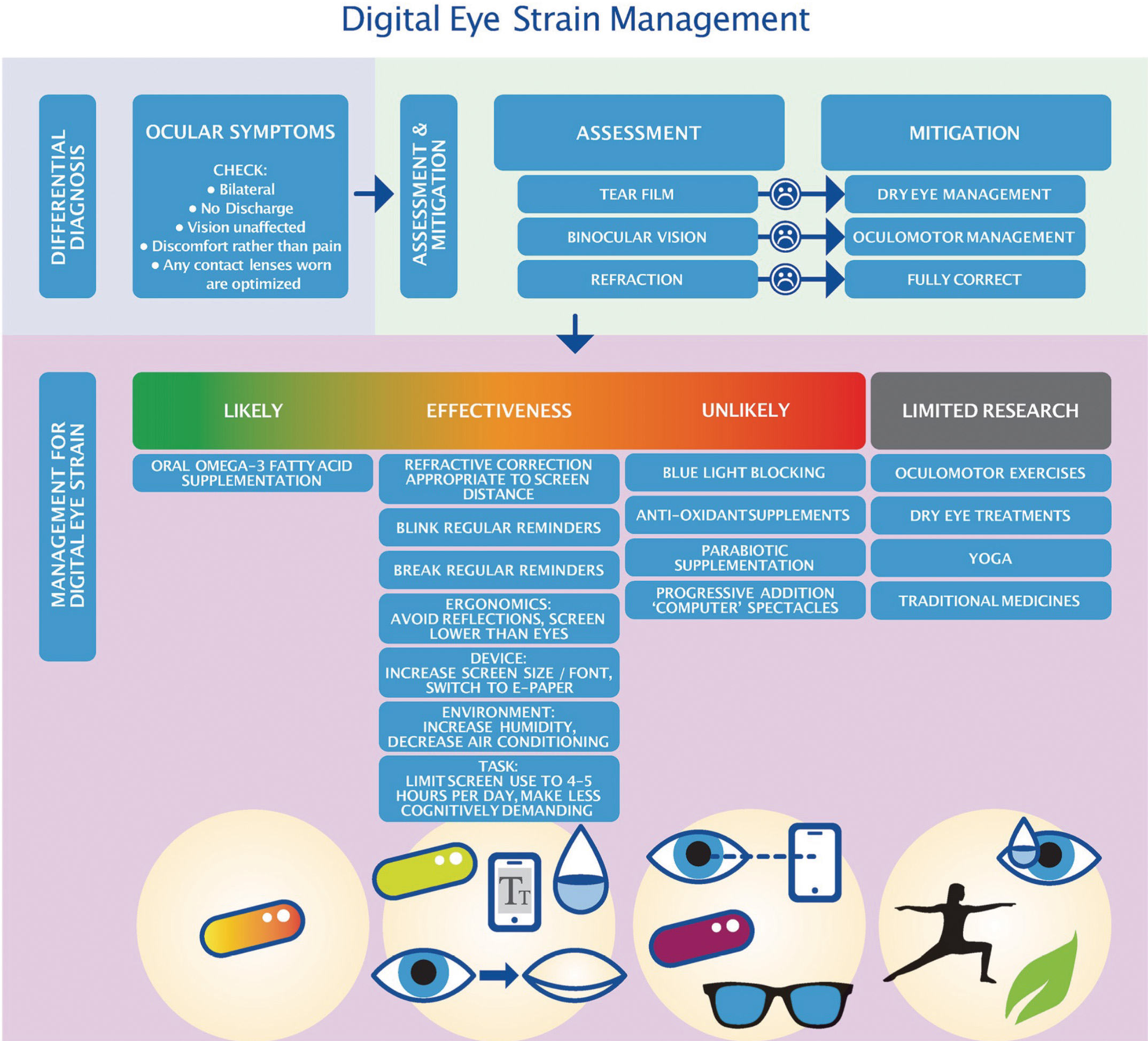
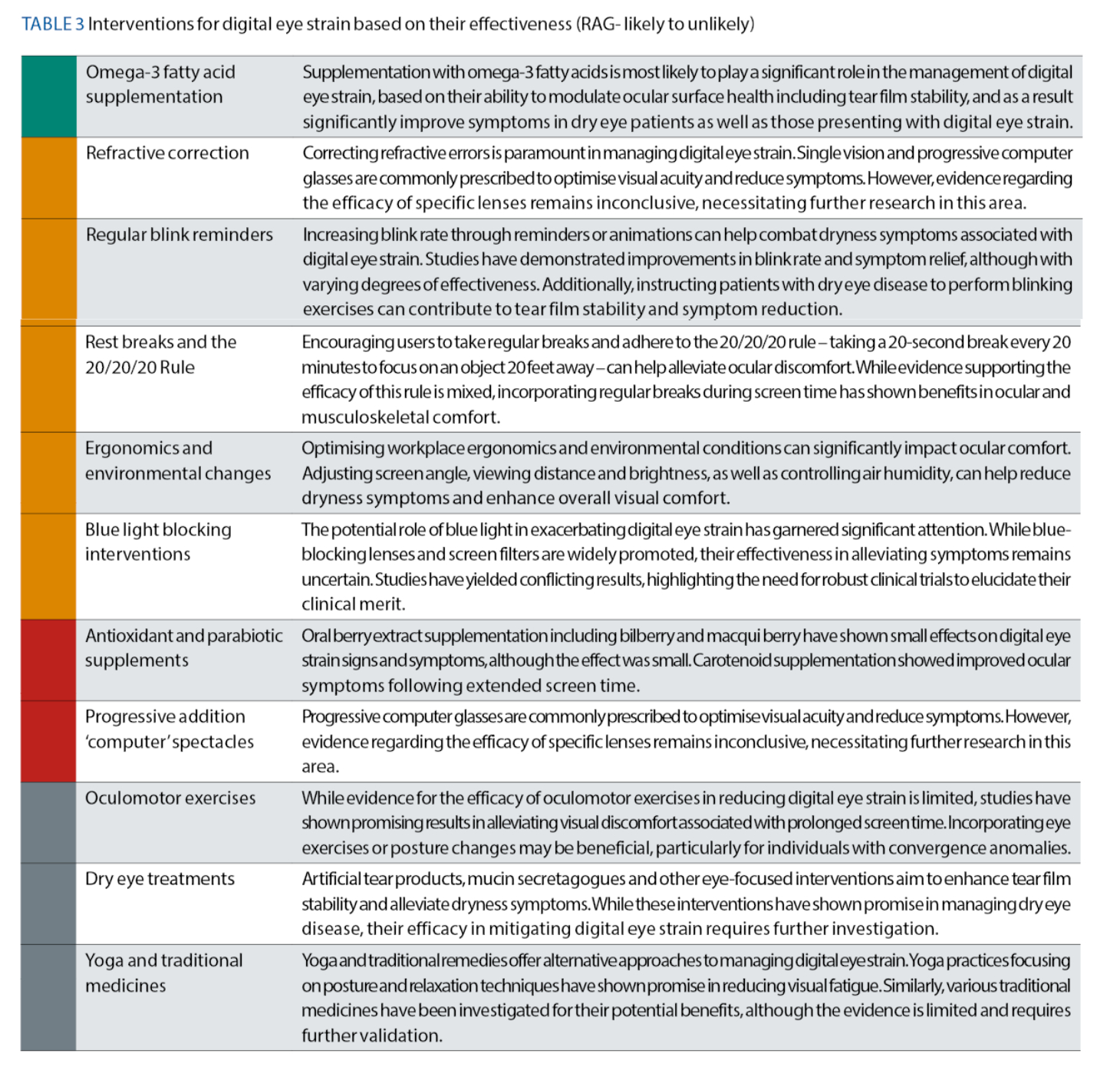
Each intervention is considered in table 3, in order of their likely effectiveness.
Practical tips for ECPs
In summary, there are several evidence-based strategies you can implement to diagnose and help patients mitigate the effects of digital eye strain:
- Consider differential diagnosis from established ocular conditions like dry eye disease, binocular vision abnormalities and refractive errors. Patients with digital eye strain should receive full refractive correction.
- Encourage regular breaks and promote the 20-20-20 rule. Recommend that patients take a 20-second break every 20 minutes and focus on something 20 feet away to alleviate eye strain.15
- Optimise workstation ergonomics by educating patients on proper posture and screen positioning to reduce musculoskeletal discomfort during computer use. An example of a detailed and ideal workstation ergonomical set up can be found here.16
- Prescribe computer-specific eyewear at the appropriate screen distance to alleviate digital eye strain and improve productivity. Blue light blocking interventions such as spectacles and screen filters do not appear to be effective based on current evidence.
- Utilise technology to monitor and manage digital eye strain, including smart cameras for tear film stability and mobile applications for reminders.
- Advocate for lifestyle modifications: encourage patients to adopt healthy lifestyle habits, such as getting adequate sleep, staying hydrated and practicing good screen hygiene to minimise the impact of digital eye strain on their overall well-being.
Conclusion
Digital eye strain poses a significant challenge in today’s digital age, impacting productivity, quality of life and overall ocular health. Addressing it in clinical practice requires a comprehensive approach, incorporating various interventions tailored to individual needs. While rest breaks, ergonomic adjustments and refractive correction play crucial roles in symptom management, ongoing research is needed to elucidate the efficacy of emerging interventions such as blue-blocking lenses and dietary supplements. By staying informed and adopting evidence-based practices, ECPs can effectively alleviate digital eye strain and improve the ocular health of their patients in an increasingly digital world.
- Dr Byki Huntjens is Educational Lead with the Association of Optometrists, and an honorary senior research fellow (City University) collaborating on TFOS Lifestyle: digital environment report, BCLA CLEAR, and Cochrane review on ‘Interventions for myopia control in children’. She is a BCLA council member and director of IACLE, and was awarded fellowships from both associations. She is president elect for the BCLA.
- Sarah Farrant is a director at Earlam and Christopher Optometrists, an optometrist and dry eye specialist and acts as a consultant and key opinion leader for a number of national and global companies. Farrant has a great passion for her work which is reflected in the wide variety of different interests she has within the profession. She has undertaken a number of additional qualifications and is a leading national expert in therapeutics and dry eye management and represents the UK as an Ambassador for TFOS. She is currently president for the BCLA. She sat for 12 years on the executive and council boards for the College of Optometrists. She has been instrumental in a number of local and national initiatives in order to improve access to education amongst the profession and access to eye care for patients. She is also a keen lecturer and regularly teaches other optometrists both nationally and internationally.
References
- Wolffsohn JS, Lingham G, Downie LE, Huntjens B, Inomata T, Jivraj S, et al. TFOS Lifestyle: Impact of the digital environment on the ocular surface. Ocul Surf. 2023 Apr;28:213–52.
- Iqbal M, Said O, Ibrahim O, Soliman A. Visual sequelae of computer vision syndrome: A cross-sectional case-control study. J Ophthalmol. 2021 Apr 2;2021:6630286.
- Jaschinski W, Bonacker M, Alshuth E. Accommodation, convergence, pupil diameter and eye blinks at a CRT display flickering near fusion limit. Ergonomics. 1996 Jan;39(1):152–64.
- Wolska A, Switula M. Luminance of the surround and visual fatigue of VDT operators. Int J Occup Saf Ergon. 1999;5(4):553–81.
- Janosik E, Grzesik J. Influence of different lighting levels at workstations with video display terminals on operators’ work efficiency. Med Pr. 2003;54(2):123–32.
- Shieh K-K. Effects of reflection and polarity on LCD viewing distance. Int J Ind Ergon. 2000 Feb;25(3):275–82.
- Inomata T, Nakamura M, Iwagami M, Shiang T, Yoshimura Y, Fujimoto K, et al. Risk factors for severe dry eye disease: Crowdsourced research using DryEyeRhythm. Ophthalmology. 2019 May;126(5):766–8.
- Lin H, Wu F-G, Cheng Y-Y. Legibility and visual fatigue affected by text direction, screen size and character size on color LCD e-reader. Displays. 2013 Jan;34(1):49–58.
- Seguí M del M, Cabrero-García J, Crespo A, Verdú J, Ronda E. A reliable and valid questionnaire was developed to measure computer vision syndrome at the workplace. J Clin Epidemiol. 2015 Jun;68(6):662–73.
- Talens-Estarelles C, Sanchis-Jurado V, Esteve-Taboada JJ, Pons ÁM, García-Lázaro S. How do different digital displays affect the ocular surface? Optom Vis Sci. 2020 Dec;97(12):1070–9.
- Chu CA, Rosenfield M, Portello JK. Blink patterns: reading from a computer screen versus hard copy. Optom Vis Sci. 2014 Mar;91(3):297–302.
- The childhood visual environment [Internet]. MyKidsVision. [cited 2024 May]. Available from: https://www.mykidsvision.org/knowledge-centre/all-about-screen-time-and-close-work#screen-time-recommendations
- Daum KM, Clore KA, Simms SS, Vesely JW, Wilczek DD, Spittle BM, et al. Productivity associated with visual status of computer users. Optometry. 2004 Jan;75(1):33–47.
- Hayes JR, Sheedy JE, Stelmack JA, Heaney CA. Computer use, symptoms, and quality of life. Optom Vis Sci. 2007 Aug;84(8):738–44.
- Five top tips on avoiding eyestrain [Internet]. The College of Optometrists. [cited 2024 May]. Available from: https://www.college-optometrists.org/news/2021/june/coronavision-eye-warning
- Environmental Health and Safety. Office ergonomics [Internet]. University of Toronto. [cited 2024 May]. Available from: https://ehs.utoronto.ca/our-services/occupational-hygiene-safety/ergonomics/
