Domains and learning outcomes (C110028)
• One distance learning CPD point for optometrists.
• Clinical practice
Upon completion of this CPD, ECPs will be able to describe how recent developments in the field of phakic IOLs could benefit patients (s5)
Upon completion of this CPD, ECPs will be able to
identify key information required to make a referral for phakic IOL surgery (s7)
Modern refractive surgery requires customised vision correction solutions and a range of options that meet patients’ visual demands and lifestyle needs. Traditional refractive procedures such as Lasik and PRK, as well as newer techniques such as small incision lenticule extraction are certainly transformative procedures. However, these options may not prove ideal for every patient and are not without their challenges and risk, such as post-operative dry eye syndrome and risk of ectasia. As prescriptions get higher and more complicated these risks have been shown to be increased.
Traditionally considered a valid alternative when laser vision correction was contraindicated – due to reasons such as dry eye disease, thin corneas and high myopia – phakic intraocular lens (IOL) implantation has more recently emerged as an essential fixture within the portfolio of refractive surgery offerings, for a wide range of patients from mild to severe myopia, hyperopia and astigmatism, thus playing a pivotal role in expanding the indications and options for refractive correction.
This article provides a historical perspective of phakic IOLs, also referred to as implantable collamer lenses (ICLs), highlighting the evolution of the technology and discussing what worked, what did not, where we are today, and what we can look forward to. For optometrists who are interested in incorporating ICL surgery into their referral discussion, this article will also review their significance in modern optometric practice. As the landscape of refractive correction continues to evolve, understanding the role of phakic IOLs within a comprehensive treatment portfolio is more important than ever for delivering the best outcomes in personalised care.
The Early Days of Vision Correction
The earliest recorded attempts at correcting vision date back to ancient Egyptian and Roman times, where glass lenses were used to magnify objects.1 It was not until the 13th century, however, that spectacles were invented, marking the first significant advancement in vision correction.
Fast forward to the 20th century, when eye care witnessed groundbreaking developments, including the introduction of contact lenses in the 1940s,2 IOLs in the early 1950s,3 and the introduction of keratomileusis in the 1960s.4
Even with these and other innovations, patients with severe myopia, hyperopia and astigmatism had extremely limited options for refractive correction, if any. The need for a more effective and comprehensive solution became increasingly evident.
Sparking Further Innovation
The first IOL, developed under the collaborative efforts of British ophthalmologist Sir Harold Ridley and optical scientist John Pike, was designed to be implanted in the posterior chamber.3 The invention of the IOL was initially met with criticism, partly due to surgical complications such as inadequate function after dislocation. Sir Harold Ridley’s innovation eventually gained recognition, and its success sparked interest in the potential of IOLs for vision correction beyond cataract surgery. It took several decades of research and development before the idea of phakic IOLs – lenses implanted in the eye without removing the natural lens – became a reality.
The first phakic IOL, designed for the correction of high myopia, was invented by Benedetto Strampelli, MD, in 1953.5 The negative-powered IOL had a concave-convex shape and was intended for placement in the anterior chamber (in front of the iris). The thick and rough lens material, however, was the source cause of complications, such as endothelial failure resulting in corneal decompensation, corneal dystrophy, pupil ovalisation, and fibrosis in the iridocorneal angle. Difficulties in appropriately sizing this anterior chamber phakic IOL often led to contact between the IOL and the structures of the angle, causing additional complications such as pupillary block and glaucoma.5
Other anterior chamber phakic IOLs were developed later in the 1950s by thought leaders such as José Barraquer, MD, and Peter Choyce, FRCS, DOMS, MS, to improve the tolerability of the IOL and reduce side effects, but both designs were associated with similar complications as Dr Strampelli’s design.6
In the 1970s and ’80s, three giants in the field – Georges Baikoff, MD; Jan Worst, MD; and Svyatoslav N Fyodorov, MD – considered iris-fixated, angle-fixated, and posterior chamber – fixated designs as different positioning sites for phakic IOLs.7, 8 They also considered various lens materials, including PMMA, silicone, collamer and hydrophilic acrylic, to determine their impact on corneal biomechanics and pressure on the iris root.9 Despite all these advances, many anterior chamber phakic IOL designs were ultimately pulled from the market and abandoned.
The Birth of Posterior Chamber Phakic IOLs
The first phakic IOL designed for placement in the posterior chamber (placed behind the iris, in front of the natural crystalline lens) was developed by Dr Fyodorov in 1986. The optic would sit in the anterior chamber while the haptics were positioned in the posterior chamber, behind the iris.10 The concept of implanting a phakic IOL in this space was sound; it was positioned at a safe distance from the endothelium and iridocorneal angle and aesthetically appealing because the lens was only visible with careful examination.
While the initial refractive results were promising, complications such as an increased incidence of anterior chamber inflammation and cataract formation resulted.11 Other posterior chamber phakic IOL models were developed, including a one-piece hydrophobic silicone IOL designed to float on the crystalline surface behind the iris with haptics resting on the zonules.
Issues with endothelial cell loss, pigment dispersion, chronic inflammation, zonular dehiscence, and subluxation in the vitreous chamber, however, remained major concerns.12
Modern Successes
Despite these challenges, the mild success of the first phakic IOLs laid the groundwork for future developments. Researchers and ophthalmologists around the world continued working on improving the design, material and surgical techniques associated with phakic IOLs.
The 1990s and early 2000s saw significant advancements in phakic IOL technology. A new lens material, collamer – a proprietary collagen copolymer – was introduced by Staar Surgical, offering greater biocompatibility than other materials such as PMMA and reducing the risk of inflammation and other adverse reactions.13 The material is also soft and flexible, allowing smaller corneal incisions, simplifying implantation and ensuring quicker healing.
The journey of phakic IOLs from experimental surgery to mainstream practice was marked by extensive clinical studies and regulatory approvals worldwide. In the United States, the FDA approved the first phakic IOL, the Artisan/Verisyse (Ophtec), designed for implantation in the anterior chamber, in 2004.
One of the most significant developments in the history of phakic IOLs, however, was the introduction of the Visian ICL in the early 2000s. The first model was approved by the FDA in 2005. Developed by Staar Surgical, the ICL is a posterior chamber lens with well-documented safety, efficacy and predictability.14, 15 Several iterative designs have been introduced over the years, with each new version offering improvements in design, materials and surgical technique.
Until relatively recently, a peripheral iridotomy was required to facilitate aqueous flow from the posterior to anterior chamber and create a protective cushion between the phakic IOL and crystalline lens. The latest model, EVO ICL (available in Europe from 2012), however, incorporates a 360µm central port in the optic that is designed to improve aqueous humour circulation in the eye. As a result, the procedure no longer requires an adjunct peripheral iridotomy.
EVO ICL posterior chamber phakic IOL
Additionally, the advanced design has increased the procedure’s safety and significantly reduced the risk of complications including anterior subcapsular cataract formation, pupillary block and the development of angle-closure glaucoma.16, 18
In the eyes treated during the FDA clinical trial, there was no incidence of pupillary block, cataract development or pigment dispersion at six months postoperative.14 These findings are consistent with other published literature.18 EVO ICL was approved by the FDA in March 2022.
A Paradigm Shift in Refractive Surgery
The success of laser vision correction techniques such as Lasik depends on many factors, including the amount and quality of corneal tissue available for ablation. As a result, patients with higher degrees of myopia as well as those with thinner or topographically irregular corneas may not be candidates for corneal-based refractive surgery due to the amount of stromal ablation required of higher refractive errors, given the increased risk of ectasia.
Additionally, individuals with preexisting dry eye disease are often not candidates because the ablative nature of the procedures can exacerbate the condition.19, 20
One way to avoid these issues with refractive correction is by leaving the corneal epithelium intact. Unlike corneal refractive surgery, phakic IOL surgery is an additive (as opposed to subtractive) procedure. Instead of disturbing the cornea, a lens is added to the eye and the cornea is preserved, as are more refractive presbyopia-correcting IOL options, for the future when age-related cataract surgery will likely be needed. ICL surgery does not alter the corneal curvature and thickness, nor does it affect future refractive targeting or optical biometry. Patients can therefore be considered for more premium presbyopia-correcting IOL options like enhanced monofocal, extended depth of focus and multifocal IOLs for reduced spectacle dependence. A phakic IOL can also be removed or exchanged by a surgeon in the rare event that it is required.
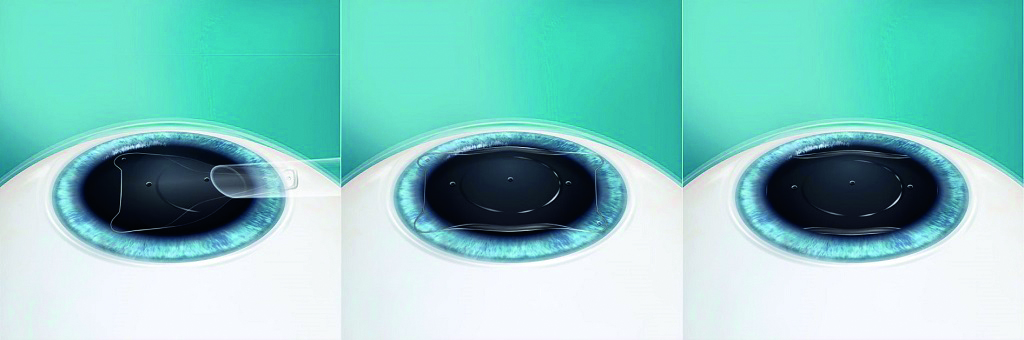
Phakic IOL procedure steps
Additionally, there is consistent evidence to suggest that ICL surgery is safe and effective even in lower degrees of myopia.15 In one comparative multicentre study of 351 eyes with low-to-moderate and high myopia, there was no significant difference in the postoperative refraction and visual acuity between the groups.21
Another study of one-year outcomes in 111 patients (172 eyes) with low myopia showed that most patients achieved 20/32 or better, 20/25 or better, 20/20 or better, and 20/16 or better uncorrected distance visual acuity (99%, 97%, 94% and 88%, respectively). Most (90%) also experienced no change in corrected distance visual acuity, and 100% and 91% of eyes, respectively, were within ±1.00 D and ±0.50 D of intended correction. At 12 months, refraction was stable (-0.14 ±0.28 D).22
In another study that compared postoperative results between patients with low (mean spherical equivalent -4.89 D) and moderate to high myopia (mean spherical equivalent >-6.00 D), the EVO ICL had excellent efficacy and safety indices in the low myopia group (1.05 ±0.17 and 1.13 ±0.18, respectively).23 This is comparative to the efficacy and safety indices of other refractive surgery procedures, such as transepithelial PRK (0.95 ±0.14 and 0.96 ±0.13, respectively) and Lasik (0.98 ±0.12 and 0.99 ±0.12, respectively).24
The Role of Optometry in Phakic IOL Surgery
Optometrists play a vital role in the management of patients with phakic IOLs from preoperative evaluation, guidance and referral, to postoperative and ongoing care. Preoperatively, optometrists may be responsible for identifying suitable candidates for phakic IOL surgery. This involves a thorough assessment, including manifest refraction, possible cycloplegic refraction, contact lens over refraction (if appropriate), and comprehensive anterior and posterior segment examination like gonioscopy.
Other important criteria for candidacy involve measurement of anterior chamber depth (ACD) and precise horizontal white-to-white measurements. Both are unique to ICLs and crucial to determining sizing. Devices such as calipers, the Pentacam (Oculus), the Orbscan (Bausch+Lomb), a topographer and more recently ultrasound biomicroscopy (UBM) may be used.
In addition to this measurement, an online lens calculator is used to obtain the ideal phakic IOL size, not unlike modern-day cataract IOL calculators. In some cases, enhanced diagnostic services as well as optimisation of the ocular surface are also performed.
Optometrists may play a key role in educating patients about the risks and benefits of phakic IOLs and helping empower them to make an informed decision about their treatment plan.
Postoperatively, optometrists may monitor patients for any signs of complications, such as elevated IOP, inflammation, clarity of the anterior chamber or endothelial cell loss. They may also evaluate the lens vault, defined as the distance between the posterior surface of the ICL and the anterior surface of the crystalline lens. Vault measurement is unique to ICL perioperative management. Thorough slit-lamp examination is important though adjunct anterior segment OCT imaging has also become a welcome support in some practices. Regular follow-up is essential to ensure the long-term success of the phakic IOL procedure and to address any issues that may arise in a timely fashion.
As primary eye care providers, optometrists are often the first point of contact for patients seeking information about vision correction options as well as a long-term trusted resource. By staying informed about the latest advancements in phakic IOL technology, we can provide patients with accurate and up-to-date information, helping them make the best and most informed choice for their vision care.
Phakic IOL operation

Challenges and Future Directions
As always, it is important to take the time with patients to explain their options and recommend the best option for their unique situation.
Looking to the future, ongoing research and development are likely to yield further improvements in phakic IOL technology. The extended depth of focus EVO Viva is a promising technology for patients with presbyopia and myopia. A multicentre prospective trial demonstrated the ability EVO Viva to improve uncorrected near, intermediate and distance vision without compromising quality of vision. Patients enrolled in the study reported significant improvements in quality of life and high levels of spectacle independence and satisfaction.25
In a study of 40 patients (80 eyes), mean postoperative binocular uncorrected and corrected distance visual acuity were 0.09 ±0.19 and 0.02 ±0.03 logMAR, respectively. The postoperative spherical equivalent was -0.61 ±0.54 D with a reduction in presbyopic add power from 1.31 ±0.74 D preoperatively to 0.44 ±0.58 D postoperatively (P <.0001).26
Conclusion
The evolution of phakic IOLs is ongoing. From the earliest days of vision correction to the modern era of customised refractive surgery, phakic IOLs play a crucial role in expanding the indications for surgery. As optometrists, staying informed about the latest developments in phakic IOL technology is essential to providing the best possible care for patients. Embracing the potential of phakic IOLs can help our patients achieve the clear, crisp vision they deserve.
- Optometrist Dr Anu Ondhia served as clinical optometric director of TLC Oakville, Ontario, Canada, and adjunct clinical instructor at the University of Waterloo, Ontario, Canada. She currently practices alongside world-renowned complex anterior segment surgeon Dr Ike Ahmed and the Glaucoma and Anterior Segment Surgery Team at Prism Eye Institute in Oakville, Ontario, Canada. She is also an active researcher, speaker, and industry partner.
- Dr Ondhia receives educational honoraria from industry partners including Alcon, Bausch+Lomb, Glaukos, Johnson & Johnson Surgical, Rayner, Staar Surgical, and others.
References
- Urban Optiks Optometry. The world before glasses: a historical insights into vision correction. March 23, 2024. Accessed August 15, 2024. https://www.uoosd.com/the-world-before-glasses
- GP Contact Lenses. A brief history of contact lenses. Accessed August 15, 2024. https://www.contactlenses.org/timeline.htm
- Apple DJ, Sims J. Harold Ridley and the invention of the intraocular lens. Surv Ophthalmol. 1996;40(4):279-292.
- London Vision Clinic. The complete history of laser eye surgery. Accessed August 15, 2024. https://www.londonvisionclinic.com/history-of-laser-eye-surgery-part-one/
- Hasan S, Tripathy K. Phakic intraocular lens myopia. StatPearls [Internet]. Treasure Island; Florida; StatPearls Publishing; 2024.
- Fechner PU, Strobel J, Wichmann W. Correction of myopia by implantation of a concave Worst-iris claw lens into phakic eyes. Refract Corneal Surg. 1991;7:286-298.
- Worst JG, van der Veen G, Los LI. Refractive surgery for high myopia. The Worst-Fechner biconcave iris claw lens. Doc Ophthalmol. 1990 Oct;75(3-4):335-41.
- Baikoff G, Arne JL, Bokobza Y, Colin J, George JL, Lagoutte F, Lesure P, Montard M, Saragoussi JJ, Secheyron P. Angle-fixated anterior chamber phakic intraocular lens for myopia of -7 to -19 diopters. J Refract Surg. 1998 May-Jun;14(3):282-93.
- Jonker SMR, Berendschot TTJM, Saelens IEY, et al. Phakic intraocular lenses: an overview. Indian J Ophthalmol. 2020;68(12):2779-2796.
- Jiménez-Alfaro I, Benítez del Castillo JM, García-Feijoó J, et al. Safety of posterior chamber phakic intraocular lenses for the correction of high myopia: anterior segment changes after posterior chamber phakic intraocular lens implantation. Ophthalmology. 2001;108:90-99.
- Marinho A, Neves MC, Pinto MC, Vaz F. Posterior chamber silicone phakic intraocular lens. J Refract Surg. 1997;13:219-222.
- Donoso R, Castillo P. Correction of high myopia with the PRL phakic intraocular lens. J Cataract Refract Surg. 2006;32:1296-1300.
- Huang D, et al. Phakic intraocular lens implantation for the correction of myopia: a report by the American Academy of Ophthalmology. Ophthalmology. 2009; 116(11):2244-2258.
- Packer M. Evaluation of the EVO/EVO+ sphere and toric Visian ICL: six month results from the United States Food and Drug Administration clinical trial. Clin Ophthalmol. 2022;16:1541-1553.
- Packer M. The EVO ICL for moderate myopia: results from the US FDA clinical trial. Clin Ophthalmol. 2022;6(16):3981-3991.
- Fujisawa K, Shimizu K, Uga S, et al. Changes in the crystalline lens resulting from insertion of a phakic IOL (ICL) into the porcine eye. Graefes Arch Clin Exp Ophthalmol. 2007;245(1):114-122.
- Shiratani T, Shimizu K, Fujisawa K, Uga S, Nagano K, Murakami Y. Crystalline lens changes in porcine eyes with implanted phakic IOL (ICL) with acentral hole. Graefes Arch Clin Exp Ophthalmol. 2008;246(5):719-728.
- Packer M. The Implantable Collamer Lens with a central port: review of the literature. Clin Ophthalmol. 2018;12:2427-2438.
- Shtein RM. Post-LASIK dry eye. Expert Rev Ophthalmol. 2011;6(5):572-582.
- Naves JS, Carracedo G, Cacho-Babillo I. Diadenosine nucleotid measurements as dry-eye score in patients after LASIK and ICL surgery. Paper presented at 2012 American Society of Cataract and Refractive Surgery Annual Meeting; April 20-24, 2012; Chicago.
- Kamiya K, Shimizu K, Igarashi A, et al. Posterior chamber phakic intraocular lens implantation: comparative, multicentre study in 351 eyes with low-to-moderate or high myopia. Br J Ophthalmol. 2018;102:177-181.
- Kamiya K, Shimizu K, Igarashi A, et al. A nationwide multicenter study on 1-year outcomes of posterior chamber phakic intraocular lens implantation for low myopia. Frontiers in Medicine. 2022;9:762153.
- Pinto C, Monteiro T, Franqueira N, Faria-Correia F, Mendes J, Vaz F. Posterior chamber collamer phakic intraocular lens implantation: Comparison of efficacy and safety for low and moderate-to-high myopia. Eur J Ophthalmol. 2022;32(2):894-901.
- Gershoni A, Reitblat O, Mimouni M, Livny E, Nahum Y, Bahar I. Femtosecond laser assisted in situ keratomileusis (FS-LASIK) yields better results than transepithelial photorefractive keratectomy (Trans-PRK) for correction of low to moderate grade myopia. Eur J Ophthalmol. 2020; dec 14 AoP.
- STAAR Surgical introduces EVO Viva presbyopia correcting lens—see young again! July 7, 2020. STAAR Surgical website. Accessed August 16, 2024. https://www.staar.com/news/2020/staar-surgical-introduces-evo-viva-presbyopia-correcting-lens-see-young-again
- Alfonso JF, Fernández-Vega-Cueta L, Lisa C, et al. Clinical and aberrometric outcomes of a new implantable collamer lens for myopia and presbyopia correction in phakic patients. J Refract Surg. 2023;39(9):589-596.
