Domains and learning outcomes (C110225)
• One distance learning CPD point for optometrists and dispensing opticians.
• Professionalism
(13.8) After successfully completing this CPD practitioners will recognise the reasonable adjustments that can be made in practice to accommodate patients with nystagmus including selecting clinically appropriate tests, adjusting the order of tests, allocating longer appointment times and utilisation of the null zone to improve delivery of optical care.
• Clinical practice
(6.2) After successfully completing this CPD Practitioners will be able to distinguish between early onset and acquired nystagmus identifying potential red flags and where necessary make appropriate referrals.
Nystagmus is characterised by continuous, rhythmic, involuntary oscillations of the eyes, and can be physiological or pathological. Pathological forms of nystagmus are not commonly encountered in primary practice, occurring in an estimated 0.24% of the population.1
This article will discuss the characteristics, assessment and management of pathological nystagmus that may present in practice.
Pathological nystagmus can be classified as early-onset or acquired. There are three types of early-onset nystagmus: infantile nystagmus syndrome (INS), fusion maldevelopment nystagmus syndrome (FMNS), formerly known as manifest latent nystagmus, and spasmus nutans syndrome (SNS). INS is the most common of these1 and will therefore be the primary focus of this article.
Clinical characteristics of Infantile Nystagmus Syndrome
INS typically develops within the first six months of life2 and is lifelong. Despite being previously called congenital nystagmus, the condition is rarely present at birth, with the average age of onset reported to be 1.9 months.3 The estimated prevalence of INS is 0.14%.1
The INS oscillation
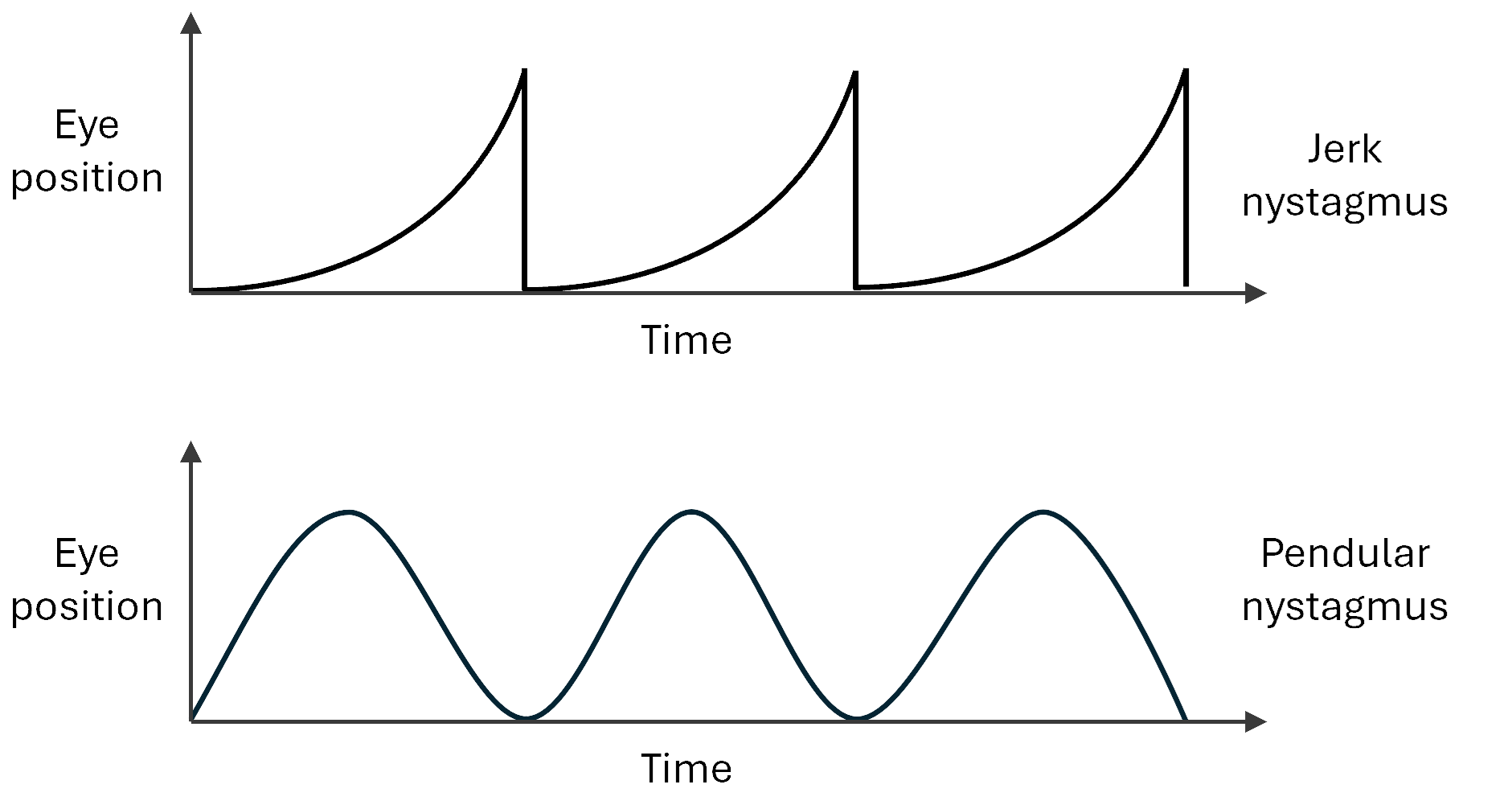
INS oscillations are primarily horizontal, although smaller secondary vertical and torsional components can be present.2 Nystagmus tends to be bilateral and conjugate.4 INS can be pendular, with the eyes moving away from and back towards the intended point of fixation in a smooth, sinusoidal manner, or jerk, in which a slow drift away from the intended point of fixation is followed by a corrective saccadic movement.
The pattern of the eye movements over time is called the nystagmus waveform. Other properties of the waveform include amplitude, frequency and intensity (amplitude x frequency). Individuals with pendular waveforms are more likely to have identifiable associated pathology.5
The intensity of INS can vary with several factors, often increasing with stress6, 7 and fatigue.4 Gaze position can also affect intensity, with many patients having a null zone – a position of gaze at which the nystagmus is dampened and vision is most comfortable.2
If the null zone is away from primary position, an anomalous head posture (AHP) may be adopted to place the eyes in the null zone while directing gaze straight ahead. In around 44% of cases, INS is also dampened with convergence, referred to as a convergence null.2, 8
Figure 1: Examples of nystagmus waveforms in INS
Associated conditions
INS often occurs in association with other ocular conditions, including foveal hypoplasia, ocular albinism, aniridia, rod and cone dystrophies, such as achromatopsia, congenital cataracts, and optic nerve hypoplasia.1
The condition is also associated with genetic mutations, notably of the X-linked FMRD 7 gene.9 INS can occur idiopathically in a visual system that appears otherwise healthy, although it must be noted that this is a diagnosis by exclusion and therefore may depend on the extent of diagnostic testing.
Visual acuity
Visual acuity (VA) varies widely in INS, often being worse in those with associated visual conditions. Mean VA has been reported as 0.67 logMAR in individuals with INS associated with albinism and 0.55 logMAR in INS associated with other ocular pathologies.2 VA is often still reduced in idiopathic cases, although to a lesser extent, with mean VA reported as 0.35 logMAR and some individuals even achieving VAs of -0.10 logMAR.2
Refractive error
High refractive errors are common in INS, ranging from myopia to hyperopia with no strong evidence that either predominates.10, 11 The prevalence of astigmatism over 1.25 DC is approximately six times higher in INS than the general population,12 with high levels of with-the-rule astigmatism observed.2, 13
Oscillopsia
Despite the continuous eye movements in INS, patients do not typically experience the perception that the world is moving back and forth, referred to as oscillopsia.14 However, some individuals do report instability of their vision under certain conditions, such as during stress and tiredness.2
Functional vision
While routine sight tests generally focus on the measurement of visual function, such as VA, it is also important to consider the effect of INS on functional vision in everyday life. Patients often find that focusing their eyes demands effort and concentration and can soon become tiring.
Furthermore, vision in INS is affected by crowding, possibly due to an underlying amblyopia.15 Reduced stereoacuity2 and motion sensitivity16 may also be experienced, and facial recognition may be challenging.17 Reading performance can be slower in INS than the general population,18 however near-typical reading performance can be achieved for font sizes 0.6 logMAR above acuity.18
Additionally, patients may experience a ‘time to see’ or ‘slow to see’ phenomenon whereby more time is required to make visual discriminations.19-22
Figure 2: Infantile nystagmus often occurs in association with albinism
(Image: Nystagmus Network)

Differential diagnosis
A key role of the optometrist when seeing a patient with nystagmus is to differentially diagnose the type of nystagmus, in order to manage and refer appropriately.
Optometrists must distinguish between early onset and acquired nystagmus, since acquired cases most commonly result from vestibular or neurological trauma or disease such as stroke or multiple sclerosis,1 and therefore require urgent referral to neuro-ophthalmology. Red flags indicating that nystagmus may be acquired include acute onset of vertical or torsional nystagmus over six months of age.23
The nystagmus waveform may differ in intensity between the two eyes and may change direction in different positions of gaze.23 Patients are also likely to experience oscillopsia alongside neurological symptoms, such as headache, nausea, diplopia and ataxia.23
Differentiating between the types of early-onset nystagmus can be more challenging due to their overlapping characteristics, however each type does have distinguishing features.
FMNS is associated with disrupted binocular vision, particularly infantile esotropia.24 On occlusion of one eye, the nystagmus will increase in intensity and beat towards the uncovered eye.5 The oscillation is further exacerbated in abduction.24
A useful approach to identifying FMNS is therefore to perform an alternating cover test with the patient looking either to the right or the left, observing if the direction and intensity of nystagmus changes with alternate occlusion.
In contrast, SNS is characterised by a fine, pendular nystagmus, which tends to occur intermittently alongside a notable AHP and irregular head nodding.25 The nystagmus tends to spontaneously reduce to subclinical levels in childhood.26
Figure 3: Infantile nystagmus can reduce with convergence
(Image: Nystagmus Network)

Optometric investigation of INS
The clinical characteristics of INS and its impact on an individual’s life can vary widely, requiring individualised assessment with a number of potential adaptations to the routine sight test. Sight tests can be demanding and stressful for those with INS due to the effort required to focus the eyes, which in turn can exacerbate the nystagmus. Optometrists should therefore ensure that patients are comfortable and at ease, and do not feel rushed.
Booking the appointment
Vision can be highly variable in INS, with many individuals having worse vision when they are tired. Scheduling appointments for times when the patient is less fatigued, such as mornings, may improve both patient experience and test results. Given that patients with INS often need more time for subjective tests and can become fatigued throughout the test, it may be beneficial to book a longer appointment or even to split the appointment into two visits.
History and symptoms
For any patient with nystagmus, it is vital to establish the age of onset and whether oscillopsia is experienced. Most patients with INS attending for a routine eye examination will have been previously diagnosed in the hospital eye service, and details of previous investigations and findings should be recorded, especially if comorbidities have been diagnosed. It is also helpful to ask about what previous management has been tried, both in the eye hospital and in primary care, and whether the outcomes have been successful.
The patient’s personal awareness of their nystagmus and how it impacts their everyday life and visual experience should be discussed, particularly noting any specific challenges and coping strategies or adaptations that have been adopted. Most patients who have a null zone will be aware of it, although use of the null zone may be more of a natural process than a conscious one.
Finally, as with any sight test, specific visual requirements such as those relating to work, hobbies and interests, computer use, and daily life should be identified so that appropriate management options can be offered.
Figure 4: Using trial frames and binocular techniques can help dampen nystagmus and make subjective refraction easier (Image: Unsplash)

Refraction
The order of tests in an eye examination should be considered to minimise the impact of patient fatigue through the appointment. Subjective tests should be performed before objective tests where possible, such as performing refraction before ocular health assessment.
Subjective refraction can be difficult for patients with INS, so a strong objective refraction is valuable. Autorefraction is rarely successful in eyes that are continuously moving, making static retinoscopy the best objective technique. To make the process as easy as possible, use trial frames and wide aperture lenses to utilise the null zone and allow for AHPs to be adopted, making sure to remain aligned with the visual axis if the eyes have moved away from primary position.
When performing subjective refraction, as with retinoscopy, trial frames are preferable to a phoropter to allow utilisation of the null zone. Given that patients with INS can take longer to make a visual discrimination and that stress can exacerbate the nystagmus and impact the refractive outcome, it is advisable to give the patient plenty of time to read the acuity chart and to respond when offering lenses. Binocular fogging with plus lenses is more suitable than monocular refraction as the intensity of INS may increase on occlusion if a latent component is present. For the same reason, monocular VA may be worse than binocular VA.
As a side note, patients who have a null zone and/or AHP will tend to naturally adopt this when reading down an acuity chart, especially as they reach their acuity threshold. This part of the sight test is therefore ideal for observing and recording the AHP and the location of the null zone.
Oculomotor assessment
A detailed assessment of the nystagmus is beyond the scope of a routine sight test, but certain aspects of the INS eye movements can be investigated, such as the presence and position of the null zone and any AHP that has been observed. It is helpful to record whether the nystagmus intensity worsens on occlusion or improves with convergence, noting the preferred near working distance in the latter case. The nystagmus should also be observed to determine whether the patient has a jerk or pendular waveform.
A cover test should be performed to attempt to identify any notable tropias, with the understanding that it can be challenging to detect small deviations when the eyes are continuously moving. Motility is also necessary to determine the relative intensity of the nystagmus in different positions of gaze.
Ocular health assessment
Thorough slit lamp assessment and fundoscopy are essential to identify and/or monitor conditions associated with INS. Common associated signs to look out for include congenital cataract (or aphakia in the case that congenital cataracts have been extracted) and aniridia as well as iris transillumination and fundus hypopigmentation in ocular albinism.
The optic nerve heads should be assessed for congenital abnormalities such as hypoplasia, and the fovea should be assessed for hypoplasia. In patients with high myopia, clinical signs such as peripheral retinal degeneration may be present.
In most cases it is possible to obtain a fundus photograph of sufficient quality to document specific clinical features of the posterior eye, although a few attempts by an experienced operator may be required. Optical coherence tomography (OCT) is also invaluable for assessing foveal hypoplasia.
In the event that the INS oscillations prevent a clear image being captured, live viewing of the OCT capture screen can still provide valuable information about the foveal structure.
Considering photophobia
For patients with associated conditions that cause photophobia such as ocular albinism, aniridia and retinal dystrophies, care should be taken to minimise the amount of bright light involved in the eye examination. Avoid excessive light from equipment such as the slit lamp and be mindful of switching the room lights on and off. In all cases, warn the patient before bright lights or sudden lighting changes, and allow them plenty of time to adapt and recover before the next test.
Additional tests
Measurement of intraocular pressure is undoubtedly challenging in patients with INS. The safest approach is to use non-contact tonometry, minimising nystagmus intensity by using the null zone where possible. Contact tonometry techniques, such as Goldmann and Perkins, pose a risk of corneal abrasion, however rebound tonometry may be a more suitable approach in the hands of an experienced practitioner.
Visual field testing is also difficult in INS due to the instability of fixation, and it may only be possible to determine coarse estimates of the visual field. Standard automated perimetry (SAP) can be attempted, using the null zone where possible. Blind spot mapping may need to be turned off.
Where SAP proves impossible, accurate confirmation perimetry can be used to identify gross visual field defects, and defects of the very central visual field may be detected using an Amsler chart if the patient has sufficient vision to resolve the grid lines.
Optometric Management of INS
Referral
Perhaps the most critical role of the optometrist, when assessing a patient with nystagmus, is determining if referral is required. As discussed previously, acquired nystagmus must be differentially diagnosed and urgently referred to neuro-ophthalmology.
Patients with nystagmus who do not exhibit signs of acquired nystagmus and have not been previously seen in the hospital eye service should be routinely referred to ophthalmology for further investigation and formal diagnosis, including identification and management of any underlying pathologies or associated conditions such as amblyopia. These patients will usually be children, but it is also possible that adults may have longstanding INS that has not been identified.
Changes in previously diagnosed INS cases should be re-referred to rule out newly acquired comorbidities. Those with longstanding INS may also wish to be referred back into ophthalmology to benefit from recent advancements in nystagmus treatments and diagnostic testing, particularly in the case of genetic testing and counselling.
Patients with INS may benefit from referral to be considered for certification of visual impairment (CVI), which will enable access to services and benefits that can support children in school and help adults live independently. In cases where patients do not meet the VA and visual field criteria for CVI but experience visual difficulties that impact their quality of life and independence, a consultant ophthalmologist can still make a discretionary decision to certify on these grounds.
Regardless of whether a patient meets the CVI standard, they can still be referred to an eye clinic liaison officer (ECLO) for signposting and practical and emotional support, as well as to low vision services for assessment and rehabilitation.
Refractive correction
For stable cases of INS that can be managed in optometric practice, a key objective is to provide the optimum form of refractive correction. This will vary widely depending on the patient’s INS characteristics and visual requirements, and a process of trial and error may be required to find the best solution.
When dispensing spectacles, lens weight, lens thickness and frame choice must be considered as with any case of high refractive error.
Patients with INS associated photophobia will benefit from tinted lenses in some form. Polarised sunglasses in particular will help to reduce glare. Clip on sunglasses, photochromic lenses, and/or multiple pairs of glasses with different grades of tint may also be useful options.
Those who require presbyopic solutions are typically more likely to get on well with lenses with a wider field of view, especially if the nystagmus is of high amplitude or the null zone is far from primary position.
Varifocals may therefore be poorly tolerated and single vision spectacles the preferable option. However, a range of multifocal lenses with varying fields of view are available to be tried, and the success of the dispense can depend completely on the patient’s motivation and lifestyle needs.
Measuring pupillary distance (PD) can be challenging in participants with INS. A sensible approach is to mark up the pupils on the dummy lenses of a frame and leave the patient to view naturally so alignment can be checked, making adjustments to the measurements as required. The lenses can be marked up directly, or PD can be measured using a pupillometer or ruler.
If it is difficult to judge the distance between the pupil centres due to the movement of the eyes, even when utilising the null zone, canthus-to-canthus measurement can be used as a starting point and refined when marking up the lenses.
In some cases where there is a clear null zone that is used regularly and is reasonably close to primary position, it can be appropriate to decentre the lenses to move the optical centre towards the null zone. Bear in mind that this will introduce aberration and prismatic effect in primary position, so this adjustment should only be made after careful consideration with the patient.
Contact lenses can be a favourable option for patients with INS as eccentric null zones can be used without experiencing the prismatic effect and aberration induced by oblique viewing through a spectacle lens.
Additionally, there is no frame to interfere with an eccentric null zone. In cases of high prescriptions, contact lenses offer the usual advantages of comfort and cosmesis as well as avoiding spectacle magnification or minification. The high prevalence of astigmatism in INS may pose a challenge to contact lens stability, so rigid lens options such as gas permeable lenses (especially back surface torics) and scleral lenses may offer a more stable fit and superior optical correction.
Some studies have indicated a possible proprioceptive effect of rigid gas permeable lenses in some patients with INS whereby the intensity of the nystagmus is dampened,27, 28 however there is no conclusive evidence that either contact lenses or spectacles give better vision in INS on the whole.29
Finally, yoked prisms can be used to reduce AHPs by shifting the image towards or into the null zone while the patient’s head remains straight. To accomplish this, the base of the prism will be in the direction of the head turn. Base out prisms can also be used to induce convergence, allowing patients with a convergence null to use this to dampen their nystagmus for distance vision.
Any prism being glazed into spectacles must be balanced with the prescription, and the weight and edge thickness of the prism should be considered. Fresnel prisms may be a preferable alternative, especially in cases where a trial period would be beneficial to confirm the suitability of the prism.
Low vision solutions
Patients with INS who have impaired visual function may benefit from low vision aids such as large print, optical or electronic magnifiers, and monoculars or binoculars. Many patients find devices that allow adjustment of text size, background colour and contrast, such as tablets, to be especially helpful.
Support services and resources
A number of groups exist that provide a wealth of support information and resources for those with nystagmus and their families. Patients with any type of nystagmus may be directed in particular to the Nystagmus Network, a UK charity that offer understanding and community alongside educational information and signposting, as well as to the RNIB. The University of Sheffield also offers helpful nystagmus information packs for both patients and practitioners.
Figure 5: Nystagmus Network community support groups

Treatments for INS
A number of nystagmus treatments can be offered by the hospital eye service, which generally aim to correct significant AHPs and/or reduce the intensity of nystagmus. These include surgical procedures to adjust the extraocular muscles and pharmacological treatments such as gabapentin and baclofen.23 It is important for patients to be aware that these interventions do not expect to eliminate the nystagmus completely.
Additional resources
For further detail on the management of INS, the reader is directed to a recent review of nystagmus management in the UK,23 which provides additional information on many of the topics covered in this article.
A Concise Practice Points document summarising the most recent guidance and best practice for investigating and managing children with nystagmus was produced last year by the Nystagmus UK Eye research group and has since been adopted by the Royal College of Ophthalmologists. This resource aims to provide an easily accessible point of reference for busy clinicians and may be a valuable addition to the test room.30
Summary
The primary goal of the optometrist in managing nystagmus is to determine if referral is required, especially by identifying the red flags that indicate acquired cases. Where INS can be managed in practice, the optimum refractive correction should be provided, and use of the null zone maximised.
Through appropriate adaptation of the routine eye examination, optometrists can meet the unique clinical challenges posed by nystagmus and significantly enhance visual function for these patients.
- Katherine Ward is an optometrist and PhD candidate at Cardiff University. Her research focuses on better understanding vision and eye movements in infantile nystagmus.
References
- Sarvananthan N, Surendran M, Roberts EO, Jain S, Thomas S, Shah N, et al. The Prevalence of Nystagmus: The Leicestershire Nystagmus Survey. Investigative Ophthalmology & Visual Science. 2009;50(11): 5201–5206. https://doi.org/10.1167/IOVS.09-3486.
- Abadi RV, Bjerre A. Motor and sensory characteristics of infantile nystagmus. British Journal of Ophthalmology. 2002;86(10): 1152–1160. https://doi.org/10.1136/bjo.86.10.1152.
- Gottlob I, Zubcov A, Catalano RA, Reinecke RD, Koller HP, Calhoun JH, et al. Signs Distinguishing Spasmus Nutans (with and without central nervous system lesions) from Infantile Nystagmus. Ophthalmology. 1990;97(9): 1166–1175. https://doi.org/10.1016/S0161-6420(90)32440-5.
- Abadi RV, Dickinson CM. Waveform characteristics in congenital nystagmus. Documenta Ophthalmologica. 1986;64(2): 153–167. https://doi.org/10.1007/BF00159990.
- Leigh RJ, Zee DS. The Neurology of Eye Movements. 5th ed. Oxford University Press; 2015.
- Cham KM, Anderson AJ, Abel LA. Task-induced stress and motivation decrease foveation-period durations in infantile nystagmus syndrome. Investigative Ophthalmology and Visual Science. 2008;49(7): 2977–2984. https://doi.org/10.1167/iovs.07-1626.
- Jones PH, Harris CM, Woodhouse JM, Margrain TH, Ennis FA, Erichsen JT. Stress and visual function in infantile nystagmus syndrome. Investigative Ophthalmology and Visual Science. 2013;54(13): 7943–7951. https://doi.org/10.1167/iovs.13-12560.
- Dickinson CM. The elucidation and use of the effect of near fixation in congenital nystagmus. Ophthalmic and Physiological Optics. 1986;6(3): 303–311. https://doi.org/10.1111/j.1475-1313.1986.tb00720.x.
- Tarpey P, Thomas S, Sarvananthan N, Mallya U, Lisgo S, Talbot CJ, et al. Mutations in FRMD7, a newly identified member of the FERM family, cause X-linked idiopathic congenital nystagmus. Nature Genetics. 2006;38(11): 1242–1244. https://doi.org/10.1038/ng1893.
- Healey N, Mcclelland JF, Saunders KJ, Jackson AJ. Longitudinal study of spherical refractive error in infantile nystagmus syndrome. Ophthalmic and Physiological Optics. 2014;34(3): 369–375. https://doi.org/10.1111/OPO.12117.
- Sampath V, Bedell HE. Distribution of refractive errors in albinos and persons with idiopathic congenital nystagmus. Optometry and Vision Science. 2002;79(5): 292–299. https://doi.org/10.1097/00006324-200205000-00008.
- Fresina M, Benedetti C, Marinelli F, Versura P, Campos EC. Astigmatism in patients with idiopathic congenital nystagmus. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2013;251(6): 1635–1639. https://doi.org/10.1007/S00417-013-2290-Y.
- Wang J, Wyatt LM, Felius J, Stager DR, Stager DR, Birch EE, et al. Onset and progression of with-the-rule astigmatism in children with infantile nystagmus syndrome. Investigative Ophthalmology & Visual Science. 2010;51(1): 594–601. https://doi.org/10.1167/IOVS.09-3599.
- Leigh RJ, Dell’Osso LF, Yaniglos SS, Thurston SE. Oscillopsia, retinal image stabilization and congenital nystagmus. Investigative Ophthalmology & Visual Science. 1988/02/01. 1988;29(2): 279–282.
- Tailor VK, Theodorou M, Dahlmann-Noor AH, Dekker TM, Greenwood JA. Eye movements elevate crowding in idiopathic infantile nystagmus syndrome. Journal of Vision. 2021;21(13): 9–9. https://doi.org/10.1167/JOV.21.13.9.
- Dai B, Cham KM, Abel LA. Perception of Coherent Motion in Infantile Nystagmus Syndrome. Investigative Ophthalmology & Visual Science. 2022;63(1): 31–31. https://doi.org/10.1167/IOVS.63.1.31.
- McLean RJ, Windridge KC, Gottlob I. Living with nystagmus: a qualitative study. British Journal of Ophthalmology. 2012;96(7): 981–986. https://doi.org/10.1136/bjophthalmol-2011-3011833.
- Barot N, McLean RJ, Gottlob I, Proudlock FA. Reading Performance in Infantile Nystagmus. Ophthalmology. 2013;120(6): 1232–1238. https://doi.org/10.1016/J.OPHTHA.2012.11.032.
- Wang ZI, Dell’Osso LF. Being ‘slow to see’ is a dynamic visual function consequence of infantile nystagmus syndrome: Model predictions and patient data identify stimulus timing as its cause. Vision Research. 2007;47(11): 1550–1560. https://doi.org/10.1016/j.visres.2007.01.008.
- Fadardi MS, Abel LA. Saccades under Mental Load in Infantile Nystagmus Syndrome and Controls. Optometry and Vision Science. 2018;95(4): 373–383. https://doi.org/10.1097/OPX.0000000000001194.
- Dunn MJ, Margrain TH, Woodhouse JM, Erichsen JT. Visual processing in infantile nystagmus is not slow. Investigative Ophthalmology and Visual Science. 2015;56(9): 5094–5101. https://doi.org/10.1167/iovs.15-16977.
- Hertle RW, Maybodi M, Reed GF, Guerami AH, Yang D, Fitzgibbon EJ. Latency of Dynamic and Gaze-Dependent Optotype Recognition in Patients with Infantile Nystagmus Syndrome versus Control Subjects. Annals of the New York Academy of Sciences. 2002;956(1): 601–603. https://doi.org/10.1111/j.1749-6632.2002.tb02894.x.
- Self JE, Dunn MJ, Erichsen JT, Gottlob I, Griffiths HJ, Harris C, et al. Management of nystagmus in children: a review of the literature and current practice in UK specialist services. Eye. 2020;34:1515–1534. https://doi.org/10.1038/s41433-019-0741-3.
- Self JE, Lee H. Infantile nystagmus. Clinical Ophthalmic Genetics and Genomics. Elsevier Inc.; 2022. https://doi.org/10.1016/B978-0-12-813944-8.00019-6.
- Averbuch-Heller L, Dell’osso LF, Leigh RJ, Jacobs JB, Stahl JS. The Torsional Component of ‘Horizontal’ Congenital Nystagmus. Journal of Neuro-Ophthalmology. 2002;22(1): 22–32.
- Gottlob I, Wizov SS, Reinecke RD. Spasmus nutans. A long-term follow-up. Investigative Ophthalmology & Visual Science. 1995;36(13): 2768–2771.
- Theodorou M, Quartilho A, Xing W, Bunce C, Rubin G, Adams G, et al. Soft Contact Lenses to Optimize Vision in Adults with Idiopathic Infantile Nystagmus: A Pilot Parallel Randomized Controlled Trial. Strabismus. 2018;26(1): 11–21. https://doi.org/10.1080/09273972.2017.1418394.
- 28Bagheri A, Abbasi H, Tavakoli M, Sheibanizadeh A, Kheiri B, Yazdani S. Effect of Rigid Gas Permeable Contact Lenses on Nystagmus and Visual Function in Hyperopic Patients with Infantile Nystagmus Syndrome. Strabismus. 2017;25(1): 17–22. https://doi.org/10.1080/09273972.2016.1276939.
- 29Jayaramachandran P, Proudlock FA, Odedra N, Gottlob I, McLean RJ. A Randomized Controlled Trial Comparing Soft Contact Lens and Rigid Gas-Permeable Lens Wearing in Infantile Nystagmus. Ophthalmology. 2014;121(9): 1827–1836. https://doi.org/10.1016/J.OPHTHA.2014.03.007.
- 30Arblaster G, Dunn MJ, Erichsen JT, Griffiths H, Harris C, Kuht H, et al. Managing Nystagmus in Childhood. London: The Royal College of Ophthalmologists; 2023. https://www.rcophth.ac.uk/resources-listing/managing-nystagmus-in-childhood [Accessed 02 October 2024]
