Domains and learning outcomes (C110801)
• One distance learning CPD point for optometrists, dispensing opticians and contact lens opticians.
• Clinical practice
Upon completion of this CPD, ECPs will be able to list the societal factors that may influence the ocular surface as described by current research (s5).
Upon completion of this CPD, ECPs will be able to describe current research into how both modifiable and non-modifiable environmental factors may influence ocular surface disease (s5).
• Specialty CPD – contact lens optician
Upon completion of this CPD, ECPs will be able to recognise the importance of history taking with regards to lifestyle when seeing patients for anterior eye health examinations including as part of contact lens fittings/aftercares (s5).
The TFOS Lifestyle reports investigate how certain environmental, social, and intrinsic factors challenge the ocular surface.
- Impact of societal challenges: Biologic, socio-economic, working/living and health communication conditions ultimately impacting the ocular surface.
- Impact of environmental conditions: Climate, its change, and the environment on ocular surface health.
The key findings of the report and its clinical implications will be outlined in this article.
Societal challenges
Biology and genetic factors
Age
Dry eye disease (DED) is one of the major age-related diseases of the ocular surface. Increasing age is a robust risk factor,1 although unexpectedly high rates of disease have been reported in young adults. DED could be partially explained by societal or behavioural factors and lifestyle activities linked to young age, such as: contact lens use, which has been shown to increase the risk of dry eye disease by two to four times,2 and high screen time, poor sleep quality, allergies, arthritis, smoking, use of oral contraceptives, antidepressants and anti-allergy medications, ocular surgery, windy conditions, very low humidity, and air-conditioning.
Age is also an established risk factor for meibomian gland dysfunction (MGD), demodex blepharitis, conjunctivochalasis, pinguecula and pterygium, infectious keratitis, and ocular surface tumours. With an increase in longevity and the rapidly growing number of older populations, it is expected that these ocular surface diseases will result in significant social and economic cost.
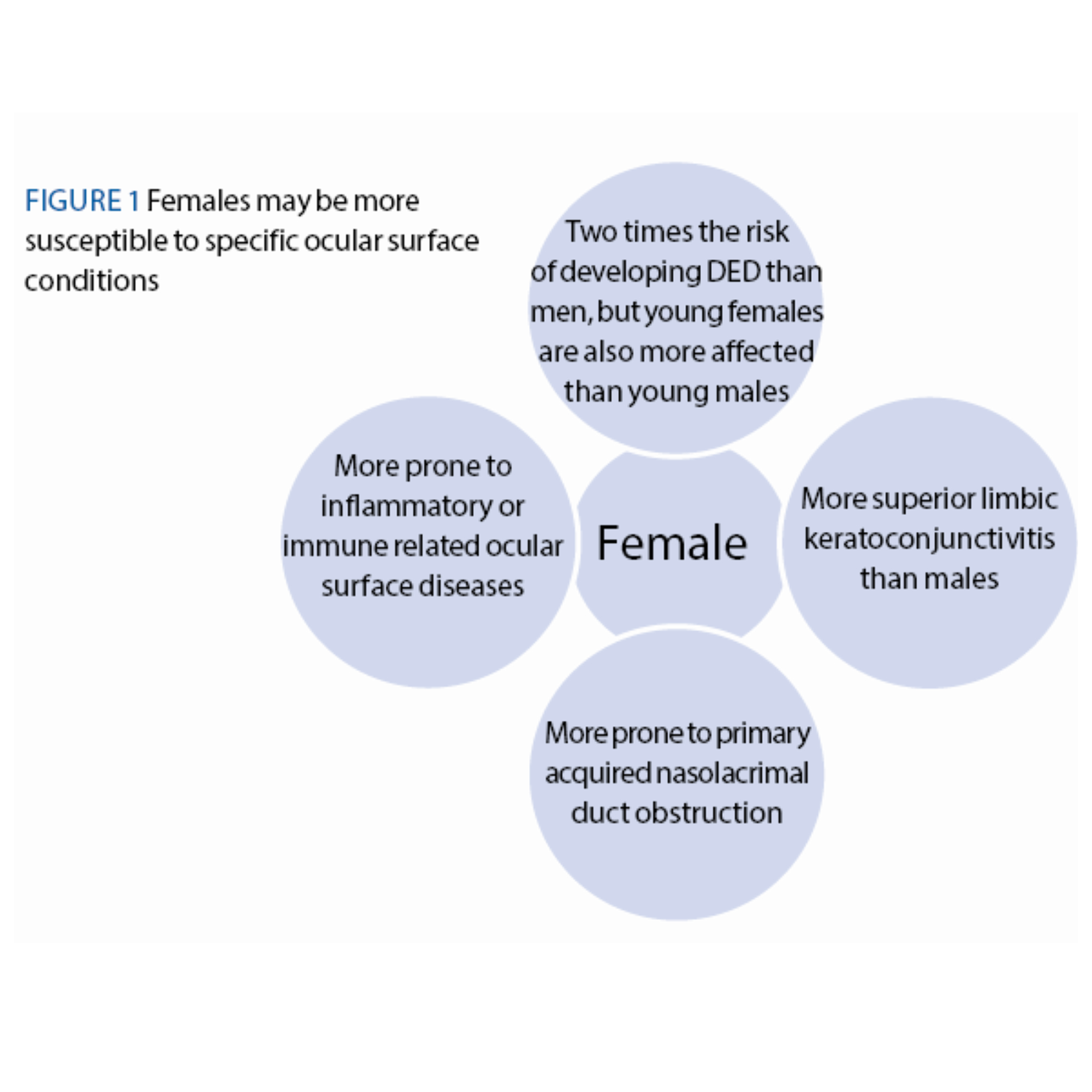
Figure 1: Females may be more susceptible to specific ocular surface conditions
Sex
Sex-related biological and physiological differences have been identified in all ocular surface structures: cornea, conjunctiva, lacrimal gland, meibomian glands, tear film and in immune function, which may be modulated by sex hormones.3 This may suggest a greater sex-related impact, particularly on those conditions related to inflammatory or immune-related mechanisms, with females being more susceptible than males to a range of ocular and systemic autoimmune diseases.
Females
- Two times the risk of developing DED than men, but young females are also more affected than young males.
- More superior limbic keratoconjunctivitis than males.
- More prone to primary acquired nasolacrimal duct obstruction.
- More prone to inflammatory or immune related ocular surface diseases.
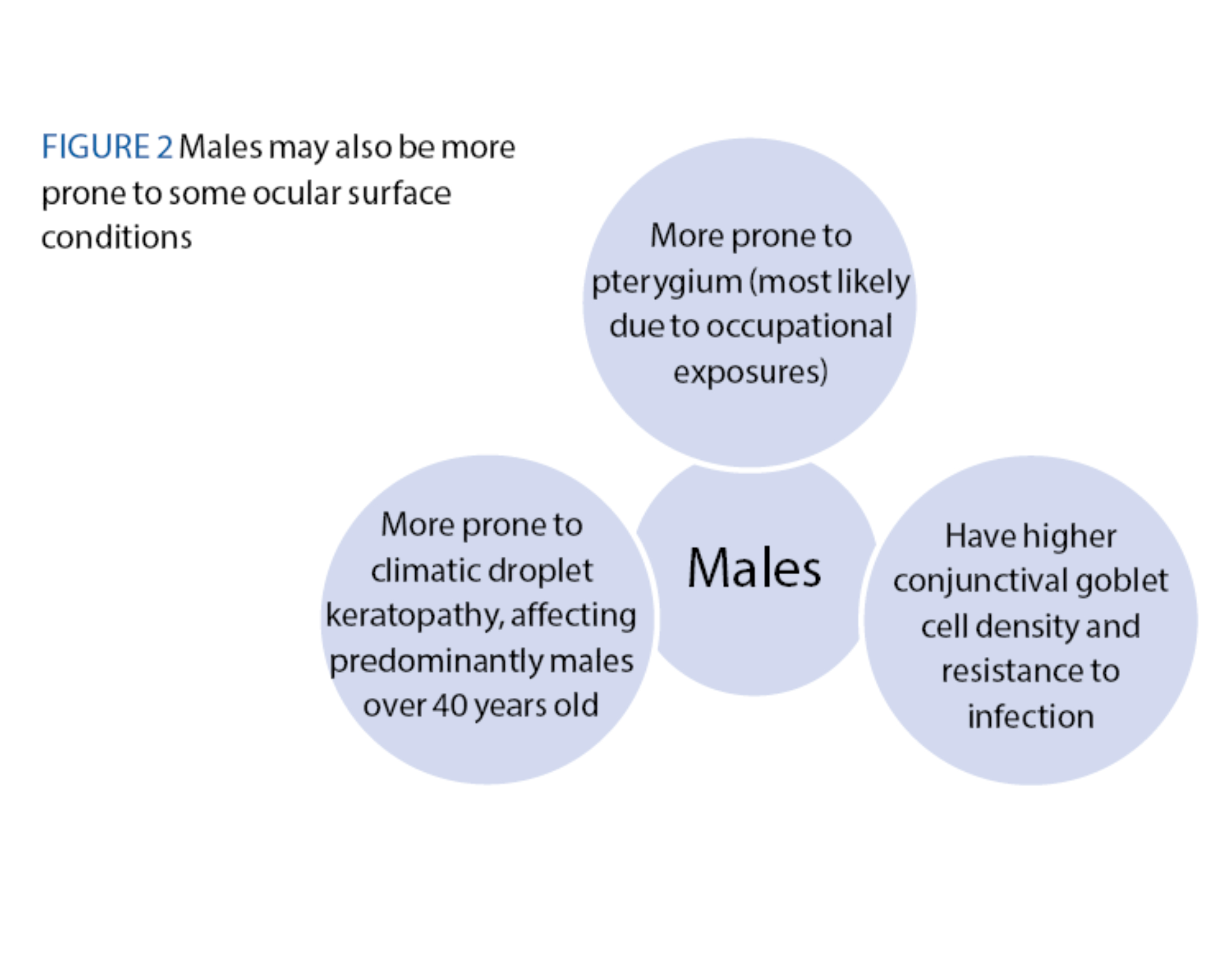
Males
- Have higher conjunctival goblet cell density and resistance to infection.
- More prone to pterygium (most likely due to occupational exposures).
- More prone to climatic droplet keratopathy, affecting predominantly males over 40 years old (Environmental report).
The perceived and reported pain is also different between sex; women are more likely than men to experience chronic pain syndromes, such as fibromyalgia, and report more severe, frequent, and more widespread body pain.
Demographic population group
It has been found that south-east Asians, particularly, appear to have 1.5-2x the risk of DED and MGD compared with Caucasians.
Genetic and hereditary factors
There is moderate heritability of approximately 30% for DED symptoms and 40% for report of a prior diagnosis of DED by a clinician, and a varying heritability of 25-80% for the various DED signs. Tear break-up time showed no evidence of genetic effects.
Atopic keratoconjunctivitis is almost exclusively associated with atopic dermatitis, with both genetic and environmental causes. While ocular allergic diseases clearly have a strong hereditary component, the evidence shows that the inheritance of these diseases does not follow a classical Mendelian pattern, suggesting that the genetics of ocular allergic disease are complex and multifactorial.
Co-morbidities
Chronic co-morbid conditions influence the prevalence and severity of ocular surface diseases, particularly those conditions which alter immune function.
Patients with chronic pain syndrome are more likely to have depression and anxiety, and as a result may take up a more withdrawn societal role, with negative perceptions of their interactions with care providers and a higher difficulty in seeking treatment for DED or any other ocular surface disease. Persistent ocular discomfort may cause patients with DED to become less physically active, lose their ability to work and experience societal withdrawal, which in turn may predispose affected patients to chronic physical and mental health conditions.
An increased DED severity was associated with a decrease of health-related quality of life.4 Furthermore, those with undiagnosed DED had significantly worse mental health-related quality of life than those who already had a diagnosis. This is a key point to understand that, as clinicians, we have the power to improve a patient’s mental health and quality of life by giving them a tangible, visceral diagnosis and therefore an understood reason for their ocular issues.
Individual lifestyle/social or community factors
Smoking (Environmental report)
Smoking is a known cause of tear film alterations, with a reduced risk of DED in current smokers, but with a higher risk in previous smokers.
- Cigarette smoke: Increase tear interleukin-6, decrease goblet cell density (associated with ocular surface staining), decrease the secretion of tear MUC5AC, increase on tear film evaporation rate reducing tear film lipid spread time, and can irritate the ocular surface, resulting in patient symptomatology.
- Nicotine-containing e-cigarettes: Reduces tear film stability and increases ocular surface staining, adversely impacts the tear lipid layer, causes changes in conjunctival impression cytology, reduces corneal and conjunctival sensitivity, increases ocular irritation and decreases anesthetised Schirmer scores, alters tear ferning grades, increases tear osmolarity, increases eyelid margin abnormalities and decreases meibum quality.
- Vaping: Decreases non-invasive tear break-up time, fluorescein tear break-up time and tear meniscus height. These effects are reported to be worse with higher vaping voltage.
Exercise
Physical exercise and sedentary behaviour were strongly linked with increased susceptibility to DED. In Japanese children, screen time and decreased physical activity was associated with obesity, DED and reduced academic performance.
Alcohol/caffeine/recreational drug use/abuse
- Alcohol: Some studies reporting alcohol consumption having a protective effect for DED, and some others detecting ethanol in tears, which decreased break-up times and Schirmer scores. More information can be found on the Nutrition report.
- Caffeine: Its consumption resulted in increased Schirmer scores at 45 min and 90 min post-consumption. On an RCT, its consumption also increased tear meniscus height. Caffeine seems to offer a benefit to the ocular surface by decreasing DED symptoms, increasing tear secretion and tear film stability.5
- Green tea is mostly consumed for its benefits in cardiovascular disease, anti-stress, anti-inflammatory and antioxidative properties, as well as neuroprotective and cholesterol-reducing properties, but its effects on the ocular surface are equivocal.
- Drug use
- Marijuana use has been associated with reduced tear secretion and decreased corneal endothelial cell density. While marijuana use may lead to DED symptoms and a decrease in tear production, it may however be useful in the management of corneal neuropathic pain.
- Snorted cocaine has been linked to decreased tear production, corneal sensitivity and decreased blink rate. Other ocular associations are anterior staphyloma, corneal ulceration, epithelial defects, corneal infiltration and infectious keratitis. Similarly, methamphetamine use has been reported to lead to conjunctivitis, corneal melting and keratitis.
Cultural and religious beliefs (plus traditional medicine)
While some traditional medicines clearly have benefits to the ocular surface, they may act as a source of microorganisms, induce toxic keratopathy, and pose a threat to vision. Where medications are not manufactured with strict hygiene protocols and tested for efficacy and safety, they should be used with caution. Their use should be restricted to those with history of ocular toxicity and by trained skilled practitioners.
Hobbies, recreational and sport-related factors
Sports such as soccer and hockey increase the risk of sight threatening eye injuries, as well as the use of miniature non-functioning replica of a gun (firing caps or pellets), which can cause a range of traumatic injuries. Firework-related eye injuries and associated consequences were reviewed by the International Globe and Adnexal Trauma Epidemiology Study: Fireworks Study Group. Outdoor or indoor ultraviolet (UV) exposure to UV light is related to ocular surface diseases including pterygium, droplet keratopathy and snow blindness. The recommendation of eye protection when doing sports is highly recommended and a private use of fireworks ban should be considered.
Societal supports/pressures
While appearance-changing diseases significantly impact mental health and psychosocial functioning (disfiguring eye conditions or prosthetics), cosmetic surgeries can improve personal wellbeing, self-esteem and different aspects of daily life. More information can be found on the elective medications and procedures report.
These include a risk of direct mechanical trauma from the needle, which may conceivably cause damage to the meibomian glands. Meibomian gland loss, evidenced by a lower meiboscore, has been reported in those with eyelid tattoos. Tattoo ink pigments persist as pigment granules in the epidermis and dermis.
Living and working conditions
- Unemployment has been linked a higher rate of ocular surface disease and DED, due to risk factors such as obesity, smoking, alcohol consumption and depression.
- Type of occupation: Occupational exposure to chemicals, thermal accidents, corrosives, pesticides, ammonia, chlorine and excessive heat may cause acute or chronic ocular surface injury. Mask-associated dry eye is due to leakage of air and limitations to lower lid movements from inappropriate mask fitting. Tape adhering to the skin of the nose and upper cheek may also interfere with movement of the lower lid, which may cause secondary entropion and lagophthalmos. Prolonged use of face masks and screens have resulted in an increased prevalence of dry eye symptoms, and working night shifts is another occupational risk factor associated with MGD, tear film instability and exacerbation of dry eye symptoms.
- Water and sanitation: Reduced access to clean water and sanitation may increase the risk of ocular surface diseases, particularly in the context of trachoma. Water contamination by various chemical and pathogens can occur through toxic, allergic, inflammatory or infective mechanisms.
- Educational and childhood education: There is a well-established link between education and poverty, socioeconomic class and access to health services, which affects both the prevalence and severity of a range of both systemic diseases and ocular diseases. Infectious keratitis is more common in those with a low educational level. There is also, a strong association between a low education level and a higher risk of both poorer visual outcome and infectious corneal blindness.
- Poverty and socioeconomic status: There is a higher prevalence of a range of eye diseases in the homeless, with trachoma and fungal keratitis being the main ones.
- Incarceration: Prison populations experience adverse health outcomes due to lack of access to services, delay in accessing appropriate care, limitations in nutrition and lack of awareness. Ocular surface conditions that are over-represented in prison populations include allergic conjunctivitis, pterygia and xeropthalmia.
Regional/global socio-economic, cultural and environmental conditions
Remoteness/geography/seasonality
The prevalence and severity of symptomatic DED, MGD and meibomian gland loss is higher in rural communities compared to urban areas. Individuals living in rural areas experience tend to suffer more with ocular surface infections such as trachoma, eyelid disease and infections, meibomian gland loss and DED. Versus in urban areas, the use of digital devices, air conditioning and exposure to pollutants also has an impact on the ocular surface.
DED is more common at high altitude and rural communities such as indigenous people, which are often marginalised and disadvantaged, due to poverty and remoteness to health care.
Seasonal and geographic variations have been reported in ocular surface infections. Warmer summer months appear to be associated with an increase in the reporting of infectious keratitis, and a particular Pseudomonas sp. Similarly, the onset of Acanthamoeba keratitis appears to be higher in the summer and autumn months. Climate influences the rate and severity of contact lens-related infectious keratitis, with more severe disease caused by environmental organisms more common in tropical regions and with high daytime temperatures.
Culturally appropriate services, free of bias or discrimination
Cultural factors such as trust, perceptions of health, communication and language play a critical role in the acceptability of health services. Furthermore, distrust, racism and discrimination can negatively influence the ability of some patients to seek care.
Effect of sex and (trans) gender on access to services
The societal impact of sex or (trans) gender on ocular surface diseases may manifest as a lack of timely access to services for a range of reasons. Factors affecting the ability of women to seek eye care services include social and cultural factors (freedom of mobility and lack independence).
There is evidence of discrimination and decreased access to healthcare services for transgender individuals in both developing and high-income countries. Transgender individuals have reported discrimination from health workers, fear of rejection and stigma and financial constraints as factors hindering access to health care services in general, and to eye care services in particular.
Cost of diagnosis/treatment insurance coverage/out of pocket expenses
The costs of diagnosis and management of ocular surfaces diseases and the bearer of these costs varies enormously by region. Apart from factors that differ across countries, interstate differences in financing and providing state of art health care in federated countries further contribute to widening the chasm of affordability among individuals.
Environmental report
Impact of climate change
The increased rate of natural disasters, continuous crop losses and loss of livelihood, extreme weather conditions and their impact on agricultural yield adds to the very present threat to food security. Such an effect on food security a clean water may impact children, increasing the prevalence of diseases associated with malnutrition such as vitamin A deficiency and trachoma associated with eye-seeking flies related to high air temperature (caused by Chlamydia trachomatis – considered one of the main causes of infectious corneal blindness)
- Temperature (extremely high or low either outdoor/indoor) is associated with DED, can affect ocular surface homeostasis, and directly and indirectly precipitate distinct forms of ocular surface diseases and symptoms.
Cool air current lowers the ocular surface temperature and increased ocular surface temperature is associated with ocular blood flow from ocular surface inflammation.
- Humidity: Low relative humidity is associated with increased ocular irritation and alteration of the precorneal tear film; these effects may be exacerbated by visual display unit work.
- Wind speed played an important role in tear film rupture time, especially at higher speeds. However, the current literature is limited.
- Dew point (temperature in which air must be cooled to reach maximum water saturation – 100% humidity), was positively correlated only with tear break-up time, suggesting that a higher dew point may be a protective factor for tear film stability.
- Altitude: High altitude conditions are characterised by low air pressure, hypoxia, low oxygen saturation, dry and cold air, prolonged and increased exposure to sunlight, solar infrared light and ultraviolet radiation, and wind and dust. At high altitudes, the ultraviolet radiation impact is greater, damaging almost all eye tissues from lids, cornea and conjunctiva to lens and retina. The UV photo-oxidates tissues, and generates reactive oxygen species, which may trigger the pathophysiology of DED and other ocular surface diseases. The most common related ocular surface diseases are pterygium and cataracts. High altitude for short-term has effects on corneal thickness, and increased risk of photokeratitis, and long-term effects such as high risk of pterygium and DED.
- Allergens: Extreme weather conditions, increasing temperatures and precipitation have resulted in longer pollen seasons and allowed for higher concentrations of indoor and outdoor mould spores. Consequently, exposure to such aeroallergens grows, making the management of allergic rhino-conjunctivitis a significant challenge.
Outdoor risk factor
Air pollution is the mixture of toxic chemicals or compounds in the air at levels that present a risk to health. Across the globe, air pollution-related diseases pose a massive threat to human health. The ocular surface is constantly exposed to indoor/outdoor air pollutants that are not mutually exclusive. Gases, bioaerosols and particulate matter (PM) can freely exchange between outdoor and indoor environments through opening sites of windows and doors upon certain meteorological and airflow conditions.
- Gases and PM: There were a greater number of inflammatory cells in conjunctival cytology sample in participants living in towns with heavy pollution compared to those living in the countryside, regardless of patient sex. Increased air pollution from the burning of biomass is associated with increased tear film instability, ocular surface staining and irritating ocular symptoms. There is also a significant association between the development of primary Sjögren’s syndrome and exposure to occupational chemical solvents.
- Volcanic ash: Volcanic eruptions appear to cause a variety of ocular symptoms, which may be self-limiting or mostly responsive to symptomatic treatment. Contact lens wearers and patients with pre-existing DED appear to suffer more symptomatology and ocular surface abrasions.
- Coal dust: Coal dust exposure was associated with reduced tear secretion and tear break-up time comparing coal miners and general workers.
- Other pollutants: High blood mercury levels have been associated with symptoms of DED in the South Korean population. The incidence and prevalence of Sjögren’s syndrome were significantly increased in areas where soils contained high levels of chromium.
This systematic review (Environmental report) evaluated evidence for the association between various air, soil and water pollutants and DED, and found:
- Air pollution from NO2 is probably associated with increased ocular irritation and lower tear break-up time.
- Soil pollution from CO is probably associated with increased dry eye symptoms.
- PM <10μm is not associated with DED diagnosis or symptoms.
- Soil pollution from chromium may be associated with DED and Sjögren’s syndrome diagnoses.
Indoor risk factor
- Sick building syndrome and sick house syndrome: Acute health effects or discomfort that can be linked directly to the time spent in the building – former – and that are alleviated when away – latter – (related to; humidity, illumination, temperature, air velocity, air conditioning, toluene and paint thinners, construction materials, particles and mould, as well as gaseous and particulate indoor air pollution). The most prevalent symptoms reported were: ‘tired or strained eyes,’ ‘dry, itching, or irritated eyes’ and ‘watering eyes’. These symptoms are general but may also be a sign of a specific ocular condition or disease, such as DED, refractive error or conjunctivitis, which indicates a building-related illness rather than sick building syndrome.
Others
- Biochemicals and bioterrorism (chemical): Lead to systemic alterations, but when in contact with the ocular surface results in an immediate ocular pain, followed by conjunctivitis and blurred vision, causing epithelial defects, chronic inflammation, neovascularisation and permanent corneal limbal stem cell deficiency.
Environmental-related OSD
DED
Environmental exposures are listed as consistent risk factors of DED along with age, female sex, Asian race, MGD, connective tissue disease, Sjögren’s syndrome, androgen deficiency, and modifiable factors including computer use, contact lens wear, hormone replacement therapy, hematopoietic stem cell transplantation and medications (antihistamines, antidepressants, anxiolytics, isotretinoin).
Allergy
The most severe forms of ocular allergy, vernal and atopic keratoconjunctivitis, although rarer, deserve specific focus, given their major impact on quality of life and their potential for devastating visual complications. Some forms of ocular allergy show seasonal variations in symptom prevalence and severity due to pollen count and weather variations.
Risk factors associated with a higher prevalence of ocular allergy include climate-related factors of high environmental temperature and low humidity, exposure to mould/dampness, dust particles, cigarette smoke, close household animal contact during childhood and atopic parental history.
Ocular surface neoplastic disease
The most important environmental predisposing factors are chronic solar UV B radiation and cigarette smoke exposure. Individual risk factors for ocular surface squamous neoplasia include, pale skin, pale iris, propensity to sunburn, more than 50% of exposure time outdoors in the first six years of life and living within 30° of the equator.
Climate change and OSD
Conflict/displacement
War and violent attacks may affect the eye and ocular health in several ways, most notably through ocular trauma from penetrating and perforating injuries to the cornea or globe, endophthalmitis, and secondary ocular infections.
Chemical injuries that may occur accidentally in the domestic setting, violent chemical attacks, such as acid attacks impact the ocular surface significantly and lead to significant epithelial loss, limbal ischemia, and even blindness.
About 45% of intimate partner violence is associated with ocular injury. Injuries that may occur in cases of domestic violence include orbital fractures, closed globe injuries and chemical injuries such as intentional acid attacks.
Information communication and technology – health communication
Impact on mental, physical and social health
Younger people increasingly use social media, thus may be at a higher risk of impact. Both screen viewing and mobile phone use may contribute to the development of depressive symptoms in young adolescents. Prolonged exposure to social media, especially cosmetic surgery–related material, is associated with an increased likelihood of considering cosmetic procedures in the future.
Patient and practitioner specific issues with impact on access to care
While patients generally view telemedicine as a favourable modality due to elimination of the need for travel and improved ability to be able to communicate with a provider, the opinion of physicians is less definitive, with a perception of superior overall quality for in-person visits, which may in part be due to a lack of experience with telehealth.
Impact of COVID-19 pandemic
Mental health
The prevalence of mental illness increased during the pandemic, specifically depression, anxiety and harmful behaviours. Social isolation and loneliness may have underpinned these adverse psychiatric co-morbidities, along with reduced access to appropriate services, which may increase the risk or severity of ocular surface disease, including DED. Medical treatments for mental health conditions have been linked to abnormal ocular surface pigmentation, corneal oedema, eye irritation, ocular itching, reduced tear break-up time and decreased lacrimation.
Access to services
A reduction in the number of eye exams being performed and postponement of visits for comprehensive eye exams and follow ups for management of chronic eye conditions, likely negatively affected the eye health of many patients. In the United Kingdom, it is estimated that more than 10,000 patients at risk of sight-threatening macular disease missed out on essential eye care.
Frequency and severity of OS diseases
Most studies reported increased screen time, extensive use of digital and screen-based technologies, or distance learning because of the pandemic, and consistently reported the development or progression of digital eye strain or computer vision syndrome symptoms, and dry eye symptoms and signs.
Conclusions
Societal report
While the impact of age, race and biological factors on many ocular surface diseases are well established, the effects of sex may be confounded by other social or gender constructs including access to health care, employment, poverty and education. Individual choices, social or lifestyle factors, such as exercise, recreational drug use, hobbies, traditional medicines, the effects of societal supports/pressures, and living and working conditions can significantly impact ocular surface diseases.
Additional factors having an impact on ocular surface are; regional and global socioeconomic, cultural and environmental conditions including the impact of remoteness to treatment, the change in the spectrum of disease with seasonality or climate variations, availability and affordability of eye care services and culturally appropriate services.
The effects of climate change on access to services, water quality and food security may influence the type and severity of ocular surface diseases. The systematic review established that the Covid-19 pandemic and various mitigating strategies/their consequences, including increased screen time and online learning were associated with an increased risk of developing new or worsening pre-existing ocular surface diseases.
Environmental report
Multiple risk factors can play a pivotal role in the mechanisms of a specific ocular surface disease (for example, pterygium and exposure to UV, exposure to allergens and allergic conjunctivitis), but also can increase risk and/or aggravate clinical presentation and outcomes in many others such as DED. Indoor exposures are very common and affects the workforce leading to reduced productivity and absenteeism. Symptoms are often non-specific and there is no consistent symptom pattern reported in published studies.
- Dr Sònia Travé Huarte is a researcher and optometrist at Aston University. She specialises in dry eye diagnostics and treatments. Dr Huarte is a clinical supervisor at Aston University; associate fellow of the higher education academy; and the British Contact Lens Association’s fellowship lead.
- Sarah Farrant is a director at Earlam and Christopher Optometrists, an optometrist and dry eye specialist and acts as a consultant for national and global companies. She has undertaken a number of additional qualifications and is a leading national expert in therapeutics and dry eye management and represents the UK as an Ambassador for TFOS. She is currently president of the BCLA and sat for 12 years on the executive and council boards for the College of Optometrists.
Further information
Further information can be accessed at tearfilm.org:
Alves M, Asbell P, Dogru M, Giannaccare G, Grau A, Gregory D, Kim DH, Marini MC, Ngo W, Nowinska A, Saldanha IJ, Villani E, Wakamatsu TH, Yu M, Stapleton F. TFOS Lifestyle Report: Impact of environmental conditions on the ocular surface. Ocul Surf. 2023 Jul;29:1-52. doi: 10.1016/j.jtos.2023.04.007. Epub 2023 Apr 14.vi
Stapleton F, Abad JC, Barabino S, Burnett A, Iyer G, Lekhanont K, Li T, Liu Y, Navas A, Obinwanne CJ, Qureshi R, Roshandel D, Sahin A, Shih K, Tichenor A, Jones L. TFOS lifestyle: Impact of societal challenges on the ocular surface. Ocul Surf. 2023 Apr;28:165-199. doi: 10.1016/j.jtos.2023.04.006. Epub 2023 Apr 14.vii
References
- Sharma A, Hindman HB. Aging: a predisposition to dry eyes. J Ophthalmol. 2014;2014:781683. doi: 10.1155/2014/781683. Epub 2014 Aug 14. PMID: 25197560; PMCID: PMC4150485.
- Stapleton F., Alves M., Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15(3):334–365.)
- Nuzzi R, Caselgrandi P. Sex Hormones and Their Effects on Ocular Disorders and Pathophysiology: Current Aspects and Our Experience. Int J Mol Sci. 2022 Mar 17;23(6):3269. doi: 10.3390/ijms23063269. PMID: 35328690; PMCID: PMC8949880.
- Mathias Kaurstad Morthen, Morten Schjerven Magno, Tor Paaske Utheim, Harold Snieder, Christopher J. Hammond, Jelle Vehof, The physical and mental burden of dry eye disease: A large population-based study investigating the relationship with health-related quality of life and its determinants, The Ocular Surface,Volume 21,2021,Pages 107-117,ISSN 1542-0124,
- Osei KA, Ovenseri-Ogbomo G, Kyei S, Ntodie M. The effect of caffeine on tear secretion. Optom Vis Sci. 2014 Feb;91(2):171-7. doi: 10.1097/OPX.0000000000000129. PMID: 24240351.
- Alves M, Asbell P, Dogru M, Giannaccare G, Grau A, Gregory D, Kim DH, Marini MC, Ngo W, Nowinska A, Saldanha IJ, Villani E, Wakamatsu TH, Yu M, Stapleton F. TFOS Lifestyle Report: Impact of environmental conditions on the ocular surface. Ocul Surf. 2023 Jul;29:1-52. doi: 10.1016/j.jtos.2023.04.007. Epub 2023 Apr 14.
- Stapleton F, Abad JC, Barabino S, Burnett A, Iyer G, Lekhanont K, Li T, Liu Y, Navas A, Obinwanne CJ, Qureshi R, Roshandel D, Sahin A, Shih K, Tichenor A, Jones L. TFOS lifestyle: Impact of societal challenges on the ocular surface. Ocul Surf. 2023 Apr;28:165-199. doi: 10.1016/j.jtos.2023.04.006. Epub 2023 Apr 14.
