The causes of a patient appearing to be intolerant to a particular lens type, material, lens form or prescription are many and varied. Occasionally non-tolerance can be the result of a psychological decision by the patient and for many practitioners initial experience of this is often gained by the patient presenting with symptoms that fail to fit any particular pattern combined with an apparent determination to simply not get on with their new spectacles. These psychological or non-clinical non-tolerances can often be the result of one or more of the following:
- The patient feels they were forced into the purchase of a pair of spectacles
- On reflection they didn’t want to spend that much
- They have changed their mind about the style of frame chosen
- A third party has made an unfavourable comment about their new spectacles
- The spectacle lens dispensed does not reflect the patient’s lifestyle
- The spectacles fail to meet the patient’s expectations
If the practitioner suspects a patient is psychologically rejecting their spectacles, he must eliminate the possibility of a clinical non-tolerance before adopting a diplomatic approach to finding a mutually acceptable solution. This is important if the practitioner is to retain the confidence of the patient. Many of the reasons for a non-tolerance to new spectacles can easily be prevented during the initial dispensing process by careful consideration of the optical, functional and cosmetic properties of the spectacles and along with a comparison of any changes when compared to the patients existing correction and appliance.
Single vision non-tolerance
The causes of a non-tolerance when considering single vision lenses, although varied can be summarised as follows:
- Optical centration errors
- Changes in lens form and/or material
- Incorrect frame fitting or inappropriate frame selection
- Manufacturing errors
- Poor glazing and mounting
- Communication
- Cosmesis
Optical centration errors
Incorrect horizontal centration results in unwanted prism at the visual point which increases as the error in centration and/or power of the lens increases. As a subject’s horizontal fusional reserves are much greater than those in the vertical meridian, there is a greater tolerance for horizontal errors. Subjects can of course adapt to unwanted prism. However, such adaptation does not mean that the patient’s vision is comfortable and continuous wear of incorrectly centred lenses can cause the visual system to become stressed over a period of time.
It is also important to consider the patient’s binocular status. If a patient has for example a poorly controlled exophoria and incorrect centration results in base out prism being experienced at the visual point, this unwanted prism may result in decompensation with symptoms that increase with wearing the new spectacles. As vertical tolerance is far less than for horizontal symptoms are often more obvious and immediate. Errors in vertical centration, especially when there is a difference between the new and old spectacles can lead to non-tolerance.
As an example consider the distance prescription right -6.00/-1.00 x 90 and left -6.50/-2.50 x 180. The back vertex powers in the vertical meridian will be right -6.00 and left -9.00. The centration points of the patient’s existing lenses coincide with the pupil centres in an attempt to avoid any unwanted vertical (relative) prismatic effect during primary gaze. A new spare pair of spectacles is ordered to the same prescription, but this time the optical centres coincide with the horizontal centre line (HCL) which is 5mm below the pupil centres. Using Prentice’s rule the resulting unwanted vertical prism is:
Right P = cF P = 0.5 x 6 = 3? base up
Left P = cF P = 0.5 x 9 = 4.5? base up
The introduction of 1.5? of differential (relative) vertical prismatic effect may cause a non-tolerance (see Part 16 of this series – 10.10.14). It is therefore important for practitioners to be aware of the full specification of a patient’s existing spectacles when dispensing a new appliance. If a patient’s existing correction has been incorrectly centred and the patient is asymptomatic there may be justification in not ordering the correct centration. Based on experience, some practitioners advocate ordering the same again while others may order a compromise centration distance. It is also important to mention that vertical centration and the correct pantoscopic angle tilt must correspond. Another good practical example of induced or acquired anisometropia is the unilateral pseudoaphakic patient where a sudden change in refractive error in one eye can lead to non-tolerance unless precautions are taken.
Practical steps to avoid centration errors can be summarised as:
- Ascertain the position of the optical centres both horizontally and vertically of the patient’s existing lenses in relation to the patient’s pupil centres not the spectacles
- Ensure that accurate monocular centration measurements are always taken
- Be prepared to compromise on the centration distances where a patient has already adapted to a previously incorrectly centred pair of lenses (some elderly patients will actually prefer a small amount of extra base in prism when reading).
- As contact lens wearers are rarely affected by anisometropia, advise them about the need for adaptation to new spectacles.
Changes in lens form, thickness and material
A non-tolerance with any type of lens may also occur when a change is made to the lens form or lens material. It is important when faced with a non-tolerance to where the centration distances are deemed to be correct, that a methodical approach is taken to eliminating each possible cause. Common lens form problems include a change in lens form from spherical to aspheric and a large change in base curve.
Aspheric lenses pose possibly the biggest risk for potential single vision non-tolerance and although their design overcomes the poor off-axis performance that occurs in flat spheric distance designs (Tables 1 and 2), some wearers cannot tolerate them. In the author’s opinion, non-tolerances with single vision aspheric lenses are usually linked to poor dispensing and fitting and the advantages of dispensing an aspheric lens usually outweighs the disadvantages. The advantages of aspheric lenses for the normal power range are:
- Good off-axis vision as the aspherical surface eliminates the oblique astigmatism of a flatter lens
- Less distortion than an equivalent flat lens
- Flatter and therefore less bulbous
- Thinner and lighter
- Less spectacle magnification
Disadvantages of aspherical lenses include:
- More distortion than the equivalent steep lens
- Centration is more critical
- Difficult to check
- The flatter lens means that back surface reflections are more in focus than with more curved lenses
- The flatter lens has less spectacle magnification which can be a problem for reading spectacles for elderly patients with reduced near acuity
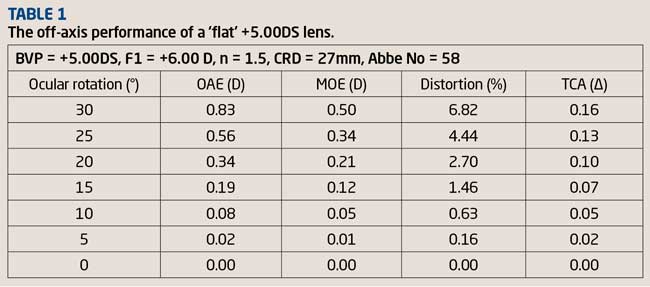
The off-axis performance of a +5.00D spectacle lens manufactured using spherical surfaces is illustrated in Table 1.
The lens is made in a relatively flat form using a front surface power of +6.00D and displays poor off-axis performance. The performance of the same lens manufactured in aspheric form with a convex hyperbolic surface is shown in Table 2.
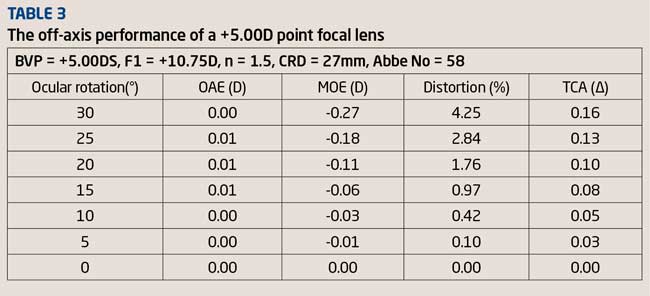
Inspection of Table 3 will show that the performance of the aspheric lens illustrated in Table 2 compares well with the performance of a +5.00D point focal lens made using conventional spherical surfaces. The lenses illustrated in Tables 1 to 3 are all designed for distance vision.
A wearer that has adapted to the off-axis performance of a spherical lens manufactured in a relatively flat form may find the sudden change in off-axis performance experienced when they are dispensed with an aspheric design difficult to adapt to. Although many wearers adapt in a few days some find adaptation problematic with common symptoms being clear vision in the primary position and blurred or ‘distorted’ vision in oblique gaze. Steeper base curves (6 to 8 base) such as those found in many wraparound style sunglass lenses can also lead to non-tolerance with the change in spectacle magnification and off-axis vision proving difficult for the patient to adapt to. Symptoms are often similar to aspheric intolerance with clear vision through the central zone of the lens and reduced acuity in oblique gaze.
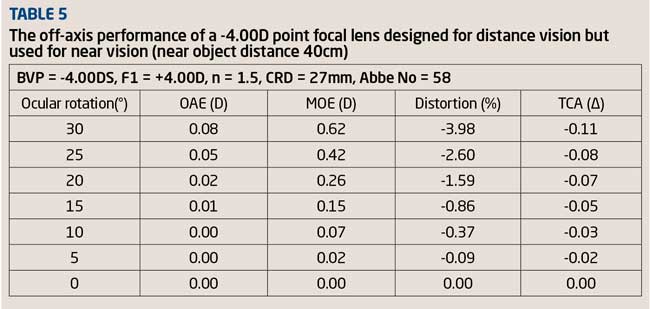
When minus lenses are used for near vision they display an increase in positive power as the eye rotates away from the optical axis. The lens effectively behaves like a weak PPL although this fact cannot of course be identified using a standard focimeter. Table 4 shows the off-axis performance of a -4.00D point focal lens designed for distance vision.
Table 5 shows the performance of the same lens used for near vision with a near object distance of 40cm.
Inspection of Table 5 shows that there is a gain in positive power of 0.62D at 30°. A -8.00D point focal lens gives a gain in positive power of almost 1.00D at 30°. This explains why myopes don’t usually require their first reading addition quite as early as hypermetropes (or need to change them so often) and why myopes sometimes have problems when changing from spectacles to contact lens in early presbyopia. However, this apparent benefit is slightly less with flatter lens forms so if a moderate to high myope complains that he cannot read quite as well with his new spectacles compared to his old ones even though the back vertex powers are the same, dust off the lens measure!
It should not be forgotten that a change in base curve, prescription, refractive index and/or lens thickness will affect spectacle magnification (SM) which was discussed in Part 16 of this series (Optician 10.10.14). Spectacle magnification is the product of the power factor and shape factor. As the shape factor is dependent on the surface powers, thickness and refractive index, theoretically changing any of these will affect the degree of SM experienced by the wearer. In practical terms since the SM of a lens directly affects retinal image size, the wearer may report that objects such as the ground appear closer or further away, although many patients do eventually adapt to this change, it is important to emphasise the need for patience while the adaption process occurs.
The effects of higher base curves, increased face-form angles and increased back vertex distance are evident in modern wrap-around style sunglasses and sports eyewear. Spectacle lenses that are mounted in frames of this type usually have a large horizontal lens size in order to give a wide field of view and are steeply curved (high base) to follow the wrap-around style of the frame. When such a frame is worn the visual axes are not normal to the lenses when the eyes are in the primary gaze position as the lenses are tilted about both their horizontal and vertical axes (Figure 1).
[CaptionComponent="2872"]
Compensation for this tilt can be made by increasing the curvature of the lenses, applying appropriate outwards decentration (or working prism) or a combination of the two. However, compensation is usually obtained by modifying the prescription to neutralise the astigmatism induced by tilting the lens. However, it should be noted that the compensated power will only be valid when the eyes are in the primary gaze position. When the eyes rotate behind the lens the cylindrical effect of the lens changes as the eye rotates around the field giving rise to the possibility of blurred vision in certain positions of gaze. When verifying an appliance that utilises prescription compensation it is of course necessary to check the power of the finished lenses against the information provided by the manufacturer.
Changes in the refractive index of a lens material may give rise to complaints ranging from a ‘lack of sharpness’ to ‘colour fringing’ around high contrast objects. Such issues are easily avoided during the dispensing process by inspection of the Abbe numbers of the lens material under consideration along with those of lens material that the patient is currently wearing. Correct centration and careful frame selection and adjustment can help reduce the unwanted visual effects of a low Abbe number material. When dispensing a patient with a very low Abbe number material it is, in the author’s opinion, sensible to mention these effects during the dispensing process. It is also sensible to advise the patient that a period of adaption is often required. In the author’s experience, although non-tolerance due to a low Abbe number lens material is not a common occurrence it does on occasions cause problems with certain patients, usually myopic physicists! Lens materials were discussed in Parts 5 and 6 of this series. In summary, care should always be taken when:
- Dispensing aspheric lenses
- Dispensing low V-value materials
- Changing the base curve of a lens
- Changing the centre thickness in plus lenses
- Dispensing a patient with a larger frame, particularly in cases of high prescriptions
Incorrect frame fitting or inappropriate frame selection
Occasionally, the practitioner may experience a potential non-tolerance to new spectacles despite the patient’s vision being perfectly acceptable. Symptoms such as poor comfort, contact marks and constant slipping are often grounds for a complaint, but not necessarily a non-tolerance. These are normally resolved through further adjustment and re-assurance. Failure to take into account any adjustment in the back vertex distance (BVD) can result in an over- or under-correction of the final lens power. Since the BVD of a frame can vary dramatically depending on the characteristics of the frame design and fit it is important that the BVD is considered when dispensing prescriptions of more than 5.00D in any meridian. Small adjustments in the vertical positioning of the optical centres (particularly in aspheric and low Abbe number lenses) can be made by altering the pantoscopic tilt and the distance between the pad centres of adjustable pad bridge frames. However, inappropriate frame selection is not as easily solved, as the complaint is often centred on the function of the frame rather than its fit or comfort. Common examples include sunglasses with a large gap between the upper rims and the wearer’s forehead, and sports eyewear that fails to perform as expected. In these cases the practitioner must re-visit the decisions made during the dispensing process and may have to accept that a remake is necessary to retain the patient’s confidence in the practice.
Mounting
Sometimes the reasons for a non-tolerance can be due to the glazing and mounting of the lenses. The most common errors include a high degree of internal stress and warped lenses. Internal stress occurs as a result of the lenses being too large for the frame. When a lens is too large it will bend at its thinnest point. This is especially true of very flexible high refractive index materials. This bending will result in a change in the curvature of the lens which will create a change in power. For example, a spherical lens may become astigmatic if it is fitted into a frame that is too small for the lens. If a lens is stressed the patient may complain of an overall lack of sharpness or clarity in vision. A secondary consideration regarding stress is any surface coating which may crack and peel. Mounting problems can of course affect all lens types and can be the cause of a progressive power lens (PPL) non-tolerance.
Communication
Any breakdown in communication between the practitioner and patient is often a major cause of patient dissatisfaction within the practice. In terms of spectacle dispensing, this can impact directly on the functional use of the spectacles. It is important that the patient immediately feels that their new spectacles are fit for purpose as it is too late to try and determine their intended use at a later date. A common example of this is single vision reading spectacles that are not suitable for computer use. Errors within the practice can also occur when writing out orders or typing them into a computer-based system. The final order and finished spectacles may initially seem to match but unless the order is checked against the original record card the error may remain undiscovered until the patient returns unhappy with their spectacles. Non-tolerance can also occur when the practitioner has failed to instruct the patient correctly on the use of their new spectacles. This may include reassurance regarding potential adaptation.
Cosmesis
Common complaints regarding the perceived cosmesis of the final appliance include:
- The lenses are thicker than the patient expected
- The tint is not what the patient expected
- The frame colour doesn’t suit them
- The frame style doesn’t suit them
Practitioners should always try to avoid issues concerning the patient’s expectations about lens thickness, tints etc by discussing the likely appearance of their new spectacles during the dispensing process. When faced with these at a later date the only solution is often a remake which is never in anyone’s interest. The most challenging non-tolerance issue is often when the patient decides that the frame colour or style doesn’t suit them. This is often the result of a negative comment by a third party and can require a high degree of diplomacy. This situation may ultimately result in a complete remake, although colour issues can sometimes be resolved by fitting the lenses into another frame of a different colour.
Whenever the practitioner is faced with a potential non-tolerance it is vital that a methodical, problem solving approach is taken. Practitioners should discuss the symptoms with the patient, look for any tell-tale signs that may assist in identifying the likely cause and discuss the problem solving processes as the various checks and measurements are completed. If the patient feels the practitioner is taking them seriously and professionally they will often be far more willing to accept any recommendations or the offer of a remake rather than insisting on a refund.
Bifocal non-tolerance
Although many non-tolerance issues relate to all lens types, bifocals present the practitioner with an additional risk in respect of the segment type, size and positioning. Common complaints include reference to:
- Jump
- A reduced field of view when reading
- The segment obstructs the patients distance vision
- Unsatisfactory intermediate vision
Changes in segment type from a round to flat-top design or vice versa will affect the amount of prismatic effect experienced at the dividing line (jump) and the centration of the near portion of the lens. Theoretically, flat-top bifocal segments provide better control of the prismatic effect at the near visual point of a bifocal lens as the base up prism induced by the segment neutralises some of the base down prism in the lower part of the main lens. Round downcurve bifocal segments induce base down prism and are therefore better for plus lenses. These neutralising effects are illustrated in Figure 2.
[CaptionComponent="2873"]
Vertical prism at the near visual point will alter the relative position of objects viewed through the segment. However, it is important to note that this is not jump which is of course the sudden introduction of base down prism introduced by the segment as the subject crosses the dividing line (Figure 3). The jump (prism) produced by a flat-top bifocal segment is base down as the optical centre of the segment (OS) is usually a few millimetres below segment dividing line. Once the patient’s gaze has passed through OS the prism produced by the segment produces base up prism. Symptoms relating to jump include the apparent movement of objects and an annular scotoma caused by the segment dividing line.
[CaptionComponent="2874"]
Symptoms of a non-tolerance due to a change in segment type are often an inability to walk up or down stairs in their new spectacles, disorientation when glancing down through the segment margin and having to raise or lower the head to read comfortably. Care taken during the dispensing process to examine the features of any previously worn bifocals will often avoid such non-tolerances.
Segment size and position should again, where possible, be matched with any previously worn bifocals and respect the patient’s vocational requirements. For new wearers it is vital that the practitioner establishes the patient’s expectations in respect of their use of the spectacles for near, distance and intermediate vision. Differential (relative) prism also poses a risk of non-tolerance if the differential (relative) prism at the near vision point is not eliminated or reduced to a tolerable level. The solutions for anisometropia were discussed fully in Part 18 of this series (16.01.15). Cosmesis is always going to be an issue when differential (relative) vertical prismatic effect is corrected with a multifocal or progressive power lens. To avoid rejection of the new spectacles the practitioner should, if possible, demonstrate the appearance of the lens using an appropriate sample.
PPL non-tolerance
By far the most challenging non-tolerances that most practitioners face are those involving PPLs. With the exception of detail that relates specifically to bifocal lenses, the practitioner must consider the issues discussed so far along with the issues of lens design and positioning. PPL non-tolerances can broadly be divided into the following reasons:
- An incorrect prescription or a genuine non-tolerance to a prescription
- Inappropriate patient selection
- Inappropriate instruction as to the use of the lens
- An inappropriate change in lens design
- An inappropriate choice of lens design
- Incorrect positioning/dispensing
- Incorrectly manufactured PPLs
A suggested procedure for dealing with PPL problems has been suggested by Tunnacliffe.1 Often an apparent non-tolerance to PPLs is caused by the patient not fully understanding how to use the lenses and therefore not obtaining the best possible performance. The role of the eye care practitioner dictates that we must ensure that every new PPL wearer understands how to use their new lenses, acknowledges any possible limitations of PPLs and has reasonable expectations of what the lens will provide. A patient will rarely be able to perform close tasks above eye level with a traditional PPL. One of the most common complaints is difficulty when reading. This is, however, often quickly solved when the patient is reminded that they should keep their head up and ensure that their gaze passes through the lower part of the lens. Patients should also understand and appreciate that a period of adaption is nearly always required when wearing PPLs for the first time, collecting new PPLs with a different lens design or PPLs with a higher reading addition. Unfortunately there is no clinical test to assess the patient’s potential acceptance of PPLs.
An inappropriate change of lens design is probably the most tricky non-tolerance issue to overcome. The vast range and diversity of progressive lenses available combined with reluctance on the part of some manufacturers to release accurate technical information about their lenses leaves most practitioners with a dilemma when opting to change PPL brand or design. Many practitioners resort to only fitting a range of lenses that they feel comfortable with, possibly through years of experience. Others are less fortunate and are only allowed to fit a small range dictated by purchasing restrictions. At some point all practitioners are faced with the need to change PPL brand or design. It is therefore important to understand the design characteristics of the lens that the patient is currently wearing and also those of the proposed alternative product. In reality, this can be a challenge if the patient’s current PPLs are not familiar to the practitioner or if it is difficult to obtain information from the manufacturer. Some practitioners never or very rarely change the design or brand of a patient’s PPL. This action is of course to avoid the risk of non-tolerance to a different lens brand/design, the philosophy being if the wearer is happy with their current design, keep to it and only consider a change for very good reasons. In the author’s opinion, the excellent designs of modern PPLs mean that this strategy is not always a sound one as a change in design/brand may benefit a patient or solve a grumble about their current lenses.
Symptoms of intolerance to a different lens design are not always evident as both practitioner and patient are expecting a degree of adaption to take place. Patients then later return often complaining that although they can see clearly through the lenses for distance and near vision, ‘the lens just does not feel right’. Some complain of a restricted near field of view while others dislike the blur that has crept into the periphery of their distance vision.
Most PPLs are available in at least two corridor lengths usually described as long and short. Historically short corridor PPLs were introduced to accommodate the trend for shallower frames. However there are other important considerations when choosing a corridor length as the corridor length of a PPL significantly influences optical performance and ultimately wearer satisfaction. If the corridor is too long for a given frame reading comfort will be reduced. Reducing the corridor length means that the optics of the PPL design must be ‘compressed’ or ‘squashed’ (Figure 4).
[CaptionComponent="2875"]
This means that the rate of change in unwanted surface aberrational astigmatism must increase resulting in reduced intermediate effectiveness, narrower central viewing zone and increased peripheral astigmatism. In summary:
Short corridor PPLs:
- Have smaller intermediate areas
- Have smaller distance areas
- Are good for moderate to high myopes as less ocular rotation is required
- Are good for short vertex distances, an increase in pantoscopic tilt and patients with a head tilt
- Are good in cases of anisometropia
Long corridor PPLs:
- Are preferred by hypermetropes
- Are good for long vertex distances
- Are good for flatter fitting frames
- Provide wider intermediate areas
- Mean less head tilt when reading
Whatever design of PPL is dispensed, it is important to ensure that any thinning prism worked on the lenses is the same in both eyes as unequal thinning prism will result in vertical differential (relative) prismatic effect.
The effect of increasing the reading addition
As the reading addition increases, the progression corridor lengthens and the width of the reading area narrows. This needs to be taken into account when dispensing second and subsequent pairs of PPLs where the reading addition will probably have increased. Unless forewarned about, this may give rise to complaint. Figure 5 illustrates three different PPL designs each with the same distance prescription and reading addition but with three corridor lengths. Lens A is designed to give a wide distance field of vision, lens B is a general use lens and lens C claims to provide good near and intermediate vision. Note how the appearance of the isocylinder lines varies with the lens design and corridor length. It is important to note that short progression lengths and high reading additions are not a good combination!
[CaptionComponent="2876"]
Fitting tips
Incorrect positioning of a PPL may also result in a non-tolerance if this is not quickly identified and if possible rectified during the collection. As with bifocals, it is vital that previous spectacles are examined and their fitting positions identified. Small adjustments in vertical positioning can still be made by altering the pantoscopic tilt, a technique that proves very useful when a patient returns later complaining of poor distance or near vision. Occasionally, and even though the fitting crosses are correctly aligned with the pupil centres, the patient has to drop their head to see clearly when driving. Posture issues like this are often easily overcome with fine adjustment of the pantoscopic tilt or pad positioning thus avoiding a non-tolerance.
- When ordering a PPL the vertical and horizontal positions of the fitting cross must be specified
- Place the fitting cross on pupil centre not corneal reflex
- Allow for the patient’s habitual posture and head position
- Always follow guidelines for minimum fitting height
- At least 10mm is usually required above the fitting cross
- Frame size and shape can influence the usable distance and near areas area of a PPL
- Use as short a vertex distance as possible
- Always fit the frame before taking measurements
Remember, although the fitting height is taken from the pupil centre to the lower rim, it is important not to forget that the reading area is inset. Make sure that the frame shape in the nasal area allows for this.
The refraction
The performance of modern PPLs can be enhanced with an accurate refraction. In the author’s experience top tips include:
- Don’t over-plus or under-minus the distance prescription
- If a traditional PPL is to be used, don’t over plus the reading addition
- If a digital freeform PPL is to be used and the patient is finding it difficult choosing between two additions that are 0.25D apart, select the higher addition as prescription compensation can affect the reading addition
- Perform a binocular refraction whenever possible
- If binocular balancing following a monocular refraction is performed, check the cylinder power and axis under binocular conditions
- Always prescribe any cylinder found
- If small amounts of vertical or horizontal aligning prism are found, prescribing these will usually enhance the performance of the lenses
PPL summary
With all PPL non-tolerances the key is to avoid them in the first place. The main points to consider are:
- Avoid unnecessary changes in lens brand or lens design
- Discuss the patient’s lifestyle, hobbies and vocation carefully so that you can make an informed decision as to which lens type to recommend
- If changing lens design ensure you discuss this carefully with the patient and make sure they understand that a period of adaption may be required
- Satisfy yourself and a new wearer that they understand how to use their new spectacles
- Don’t always accept what the manufacturer says about its lenses, talk to colleagues and compare notes regularly on different lens brands
- Treat any potential non-tolerance as a challenge and explain each step of your reasoning and the checks you make to the patient
Patients who are unlikely to succeed with PPLs include:
- Previously failed PPL wearers
- Patients who require a wide near area and cannot or are not prepared to turn their head for more lateral viewing
- Patients who are happy with single vision, bifocal or trifocal lenses
- Patients who are not disturbed by or conscious of the segment top in bifocals or trifocals
- Patients who are not prepared to gamble on the chance of adapting to PPLs or who are not prepared to wait an indeterminate time for adaptation to occur
In the author’s opinion there are five key points that contribute most to PPL wearer satisfaction. These are:
- Ease of switching between the distance and near areas
- Ease of finding the near area
- Comfortable near vision
- Clarity of image and absence of peripheral blur
- Ease of adaptation
Although not as common as it used to be, mainly due to improved lens designs, occasionally the practitioner is unable to find any reason for a PPL non-tolerance. If having checked every possible cause over several return visits, the symptoms of intolerance have not improved and there appears to have been little or no adaption, there comes a point at which practitioner and patient must agree that PPLs are not the best solution. Most manufacturers also acknowledge that this is sometimes the case and offer an intolerance warranty. Although the timescales for this vary from manufacturer to manufacturer it appears to be from 30 to 90 days. This provides the practitioner with an opportunity to revisit the patient’s requirements and recommend an alternative lens solution, be it bifocals or separate single vision pairs.
Prescription non-tolerance
One aspect of non-tolerance to new spectacles that the dispensing optician has little influence over is a non-tolerance due to a prescription change. Although this is a relatively rare occurrence it does happen from time to time. It is of course essential that the dispensing optician eliminates all other possible causes for non-tolerance before referring the patient back to the prescriber.
Common causes of prescription non-tolerance are:
- Change in cylinder power
- Change in cylinder axis
- Reading addition is inappropriate for the required working distance
- First-time spectacle wearer cannot adapt to the prescription
Freeman and Evans2,3 investigated non-tolerances that occurred in a community optometric practice. Once problems that could be resolved by the dispensing optician had been excluded, those that required an appointment with an optometrist accounted for 1.8 per cent of eye examinations. Gender was not a relevant factor, but presbyopes accounted for 88 per cent of non-tolerances. In every case, the final prescription was within 1.00D of the non-tolerated prescription, and 84 per cent were within ±0.50D. In the opinion of the authors of these studies, the finding that refractive error assessment is repeatable to within ±0.50D, and yet most non-tolerances only require an adjustment within ±0.50D, highlights the challenging nature of optical prescribing. Some experienced practitioners routinely modify their prescriptions in order to reduce the risk of non-tolerance. Useful clinical pearls from this study include:
- Do not over-plus hypermetropes
- Do not under-minus myopes
- Do not overestimate the near/intermediate addition as patients are less tolerant of over-correction.
- Investigate carefully each patient’s working distance for reading or computer use. It is difficult for patients to assess this correctly in the testing room environment, so a pre-examination questionnaire might be useful
- If a refractor head (phoropter) is used, make an allowance for the BVD as refractor heads can lead to over-correction in myopes and under-correction in hypermetropes
- Take care with testing distance, especially with 3-4m projection charts. A 6m chart overcorrects by +0.167D and a 4m chart overcorrects by +0.25D (so need to reduce the prescription by 0.25D)
- Pay particular attention to changes in prescription with presbyopes as non-tolerances are more likely, especially in the 50-59 age group
- Take care when prescribing to new multifocal wearers or when changing lens design for an existing multifocal wearer. These two groups of multifocal wearers are more sensitive to changes and more prone to non-tolerance
- Take greater care when prescribing to patients with cataract
If using a refractor head (phoropter) care must be taken if the patient has marked facial asymmetry or head tilt. When examining presbyopes it is also useful to place the near prescription in a trial frame to confirm that the near working distance is appropriate.
Summary
As with all areas of our profession, the adoption of a methodical approach to problem solving which involves the patient at every stage can help us to avoid non-tolerance issues and to solve them when they occur. With some patients practitioners instinctively know there will be a non-tolerance. The author has on rare occasions booked a non-tolerance appointment for a patient before the spectacles have been dispensed! The Optical Confederation has issued guidance on how optical practices deal with non-tolerance cases when the sight test and dispense are delivered by different community practices. The essence of the guidance is that when a practice accepts an outside prescription they should also accept responsibility for financing and managing any non-tolerance issues.
Model answers
Correct answer is in bold italic
1 Which of the following statements is incorrect?
A When dispensing spectacles it is sometimes necessary to compromise with regard to the centration distances where a patient has already adapted to a previously incorrectly centred pair of lenses.
B As contact lens wearers are rarely affected by anisometropia it is important to advise them about the need for adaptation to new spectacles.
C A positive single vision lens designed for distance vision acts like a weak progressive power lens when used for near vision.
D A subject’s horizontal fusional reserves are much greater than those in the vertical meridian.
2 Which of the following statements regarding aspheric lenses is incorrect?
A Back surface reflections can be more problematic with aspheric lenses.
B An aspheric lens has less spectacle magnification which can be a problem when dispensed as reading spectacles for elderly patients with reduced near acuity.
C It is important that aspheric lenses are correctly centred and fitted.
D Aspheric lenses exhibit more distortion than an equivalent flat lens.
3 Which of the following answer options below is incorrect? Compensation for the visual effects of high curves can be made by:
A Modifying the prescription.
B Decentring the lens inwards.
C Decentring the lens outwards.
D Working prism on the lenses.
4 Which of the following statements regarding progressive power lenses (PPLs) is incorrect?
A Short corridor PPLs are recommended for moderate to high myopes as less ocular rotation is required.
B Long corridor PPLs are recommended for hypermetropes.
C The corridor length of a PPL has no effect on the amount and distribution of surface aberrational astigmatism.
D A higher reading addition results in an increase in the surface aberrational astigmatism produced.
5 When trying to avoid a non-tolerance to a progressive power lens, which of the following statements is incorrect?
A Only change the lens brand and/or lens design if this action will be visually beneficial to the patient.
B The practitioner must be satisfied that a new wearer understands how to use their new spectacles and appreciates that a period of adaption may be required
C If the brand and/or design of a progressive power lens is changed the practitioner should not advise the patient of this.
D If small amounts of vertical or horizontal aligning prism are found, prescribing these will usually enhance the performance of a progressive power lens.
6 Spectacle magnification is said to be the product of the power factor and shape factor of a spectacle lens. Which of the following does not affect spectacle magnification?
A Surface powers
B V-value
C Refractive index
D Lens thickness
References
1 Tunnacliffe AH. Essentials of Dispensing. 2003 ABDO pp 53-54.
2 Freeman C & Evans BJW. Investigation of the causes of non-tolerance to optometric prescriptions for spectacles. Ophthalmic Physiol Opt ,2010; 30: 1–11.
3 Evans BJW. In-practice (in-office) optometric research. Ophthalmic Physiol Opt, 2012; 32 83-88.
Further reading
Fowler C and Latham Petre K (2001) Spectacle Lenses: Theory and Practice Butterworth Heinemann Oxford UK.
Jalie M (1984) Principles of Ophthalmic Lenses 4th edition The Association of British Dispensing Opticians London UK.
Jalie M (2008) Ophthalmic Lenses & Dispensing 3rd Edition Butterworth Heinemann Oxford UK.
Keirl A and Christie C (2007) Clinical Optics and Refraction Elsevier Oxford UK
Andrew Keirl is an optometrist and dispensing optician in private practice, associate lecturer in optometry at Plymouth University, ABDO principal examiner for professional conduct in ophthalmic dispensing, ABDO practical examiner and external examiner for ABDO College