Picture this. A patient presents to your practice for an eye examination and on initial assessment, you find you need to dilate him. This may be because he presented with symptoms requiring further detailed investigation of the peripheral fundus or simply for a routine detailed examination of the fundus which would not be adequately done if undilated.
So then you choose a mydriatic drug, but find that your desired choice of drug and/or dose is not available in the practice, what do you do now? Is the available mydriatic still acceptable to use on your patient and will it still have the desired effect? What happens if your patient informs you that he may have had an allergic reaction the ‘last time he was dilated’, or that he has the smallest pupils you have ever seen and dilation with the mydriatic available to you may be futile.
The aim of this article is to refresh the reader’s understanding of the various mydriatics available for the dilation of the pupil, how they work, when to dilate and when not to dilate, what physiological factors may affect dilation and a step by step guide to dilation in practice.
What is a mydriatic?
A mydriatic is a drug that causes the pupil to dilate. This is known as mydriasis. The use of drugs by optometrists is controlled by the Medicines Act of 1968. An amendment by statutory order in 1978 (SI 1978/988) gave optometrists the right to use a specified list of medicines, which may usually only be available to the public via a prescription from a general practitioner of medicine, dentist or vet.
Under the Human Medicines Regulations 2012, medicines which are classified as pharmacy (P) medicines may be sold or supplied only through registered pharmacies by or under the supervision of a pharmacist (Regulation 220). Prescription only medicines (POM) are subject to an additional requirement: they may only be sold or supplied through pharmacies in accordance with a prescription given by an appropriate practitioner.
Drugs available to optometrists for the purposes of mydriasis are:
- Phenylephrine (P)
- Tropicamide (POM)
- Cyclopentolate (POM)
- Atropine (POM, additional supply optometrist).
For the purposes of this article, only the mydriatic effect of the drug will be discussed. Cycloplegia will be reviewed later in the year.
Provided it is in the course of their professional practice and in an emergency, registered optometrists may sell or supply POMs, which are not for parenteral administration, and that contain the following substances with regard to mydriasis:
- Cyclopentolate hydrochloride
- Tropicamide.
All POMs and P medicines to which the Medicines Act exemptions apply may be sold to a registered optometrist by way of wholesale dealing. Also, a registered optometrist may obtain the following medicinal products by way of wholesale dealing:
- P medicines for administration in the course of his/her business – phenylephrine is classified as a P medicine
- POM medicines for administration (as opposed to sale or supply) – this relates to topical anaesthetic which will be discussed in a future article.
A formulary of drugs available to optometrists may be downloaded from the College of Optometrists website.
Pharmacological principles underlying drug use
Access of drug to the site of action
Administration of a drug to the eye aims to produce an adequate amount of drug at the site of action and to maintain it there for as long as necessary while minimising systemic side effects. The amount of drug administered is determined by its absorption from the site of administration, its redistribution and the elimination of the active form, either by excretion or metabolism. In optometric drug use, the most important of these is absorption.
This in turn is influenced by the lipid/water solubility of the drug, its degree of ionisation, the concentration gradient across the cornea and the contact time of the drug at the corneal surface. Lipid/water solubility is important because of the nature of the cornea – a lipid/water/lipid ‘sandwich’. To cross effectively, a drug must be both lipid and water-soluble. Most drugs used in optometry are either weak bases or weak acids; therefore they can exist in both an ionised and a non-ionised form. The degree of ionisation is determined by the pH of the medium in which the drug is located and the acid-base dissociation (usually described as the pKA) of the drug. The pH, but not the pKa, may be changed, within limits, to influence ionisation. Ionisation is important because the non-ionised form tends to be lipid soluble, whereas the ionised form is likely to be water-soluble. For effective crossing of the cornea both forms of the drug are needed.
Sites of drug action
The nervous system consists of the central nervous system and peripheral nervous system. The peripheral nervous system can be further categorised to compromise of the autonomic nervous system (ANS) and somatic nervous system (SoNS). See Figure 1 for a schematic overview of the structures involved in each. Mydriatics produce their effects directly or indirectly on the ANS.
[CaptionComponent="2934"]
A typical pathway comprises two neurones with a junction, the ganglion, between them. Transmission across the ganglion and across the junction between the nerve and the cell it innervates (the neuroeffector junction) is by chemical means. The chemical involved is called a neurotransmitter.
The ANS consists of two branches, the parasympathetic nervous system and the sympathetic nervous system. The parasympathetic system is characterised by long pre-ganglionic and short post-ganglionic nerves, whereas the sympathetic system is characterised by short pre-ganglionic and long post-ganglionic nerves.
With regard to use of mydriatics, the most significant difference is the nature of the neurotransmitter at the neuroeffector junction. At parasympathetic junctions this is acetylcholine and at the sympathetic it is noradrenaline. These neurotransmitters produce their effects by binding to and interacting with receptors located at the membrane of the innervated cell (Figure 2).
[CaptionComponent="2935"]
Drugs with similar structures which are also able to bind (show affinity) and interact to produce the same response (efficacy) are termed agonists. Those with affinity but no efficacy are termed antagonists. These will occupy the receptor and prevent access of the normal neurotransmitter, thus they will reduce or abolish the normal response to nerve stimulation.
The parasympathetic nerves supply the iris sphincter, the ciliary muscle and the lacrimal gland. Stimulation causes contraction of the iris and ciliary muscle resulting in miosis (closure of the pupil) and spasm of accommodation along with increased activity in the lacrimal gland.
Sympathetic fibres innervate the dilator pupillae and the smooth muscle of the upper lid (Müller’s muscle), the conjunctival blood vessels and the blood vessels supplying the lacrimal gland. Stimulation of these nerves results in contraction of the smooth muscle at all of these sites causing mydriasis, widening of the palpebral aperture (due to action of the Müller’s muscle in the lid), blanching of the conjunctiva and possibly decreased lacrimation. See Figure 3 for a summary of ANS influence on the iris and ciliary body.
[CaptionComponent="2936"]
The overall sequence of events is similar in both the parasympathetic and sympathetic nerves and involves synthesis and storage of the neurotransmitter in nerve endings. Arrival of a nerve impulse causes the release of the neurotransmitter, which diffuses across the synapse and interacts with the receptors, (muscarinic in the parasympathetic system and a or b in the sympathetic system). The neurotransmitter is then inactivated, either by hydrolysis by acetylcholinesterase or for noradrenaline by monoamine oxidase or catechol ortho-methyltransferase.
What mydriatics are available to optometrists?
The ideal mydriatic should dilate the pupil with little or no change in accommodation, be effective in all patients, have little/no effect on the intraocular pressure and be reliably reversed. This might be achieved by mimicry of the sympathetic system (stimulating the dilator pupillae muscle) or blockage of the parasympathetic system (blocking the action of the iris sphincter muscle). These two actions can be utilised synergistically to achieve maximum pupil dilation.
Blocking the action of the sphincter pupillae
Contraction of the sphincter muscle of the iris results in constriction of the pupil. By eliminating this action the pupil dilates. Anti-muscarinic agents actively compete with acetylcholine for receptor sites on the sphincter muscle. The drug used has a greater binding affinity for these than the body’s own neurotransmitter substance. Therefore, once an anti-muscarinic binds, acetylcholine is unable to elicit an effect (which would normally be to constrict the pupil) and hence the pupil dilates.
Tropicamide (0.5 per cent and 1 per cent minims – Figure 4) is usually the anti-muscarinic mydriatic drug of choice in optometric practice. Tropicamide is also available in a multidose bottle (Mydriacyl). It is a weakly binding compound, which has a rapid action, with good dilation and total loss of the light reflex; it causes a minimal transient accommodation changes as it does not penetrate in to the posterior chamber well and is reversible. The 1 per cent concentration is usually used for darker irides due to the pigment binding effects of the drug. It is occasionally used when cycloplegia is required for an adult, for example when investigating accommodative spasm in a teenager.
[CaptionComponent="2937"]
Cyclopentolate (0.5 per cent and 1 per cent minims) is also a mydriatic but is usually the drug of choice for cycloplegia as it causes significant paralysis or dampening of accommodation. If being used for mydriasis, the 0.5 per cent concentration should be opted for. However, patients should be advised of the significant reduction on accommodation.
Atropine (0.5 per cent and 1 per cent minim and other formulations) is also available as an anti-muscarinic mydriatic. However, due to its toxic nature, it is only available for optometrists with a therapeutic higher qualification (additional supply or independent prescriber).
Stimulating the dilator pupillae
The sympathetic division of the ANS innervates the dilator pupillae. Stimulation of the dilator will result in dilation of the pupil.
Phenylephrine (2.5 per cent and 10 per cent minims) is the sympathomimetic mydriatic drug of choice. It is also available in multidose bottles and in lower concentrations (0.125 per cent) for use as a vasoconstrictor for the relief of conjunctival congestion. It mimics noradrenaline at the a receptors, causing pupillary dilation; its effects are reversible. However, pupil dilation is not complete as the sphincter muscle is not affected and therefore the light reflex is still present. Dilating patients with dark irides is particularly difficult and as it can speed up the heart rate and blood pressure it should be avoided in the elderly especially those suffering from high blood pressure, heart disease and thyrotoxicosis. The use of phenylephrine should also be limited where conjunctival disruption or bleeding is seen.
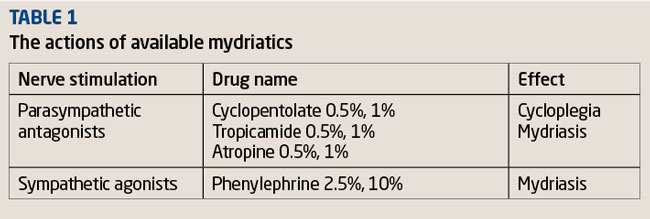
Phenylephrine 2.5 per cent can be (and is usually) used in combination with an anti-muscarinic drug (like tropicamide) to produce enhanced pupil dilation. This is particularly useful in patients whose pupils are very difficult to dilate, such as elderly patients with very small pupils, diabetics and high myopes. Table 1 summarises the actions of available mydriatics.
Clinical indications for dilation
The Opticians Act and General Ophthalmic Services (GOS) specify that an optometrist is required to perform an eye test on a patient for the purpose of detecting signs of injury, disease or abnormality in the eye or elsewhere.
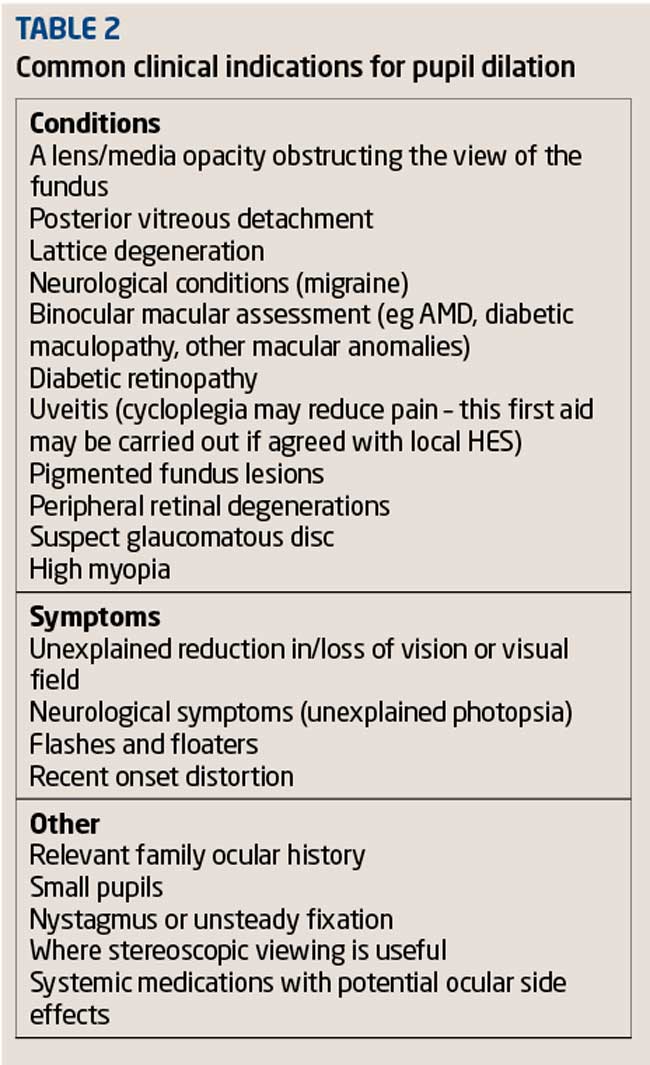
The use of a diagnostic agent such as a mydriatic may be indicated to detect some eye diseases and aid further investigation and improve visualisation, for example, a patient presenting with symptoms flashing lights and floaters, of the peripheral retina. In other situations, the use of the mydriatic may be mandatory; for example, the new GOS contract in Scotland (2006) requires optometrists to carry out a dilated fundus examination in all patients over the age of 60. In Wales, optometrists provide extended primary eye care services to improve patient access to eye care. Table 2 summarises indications for dilation.
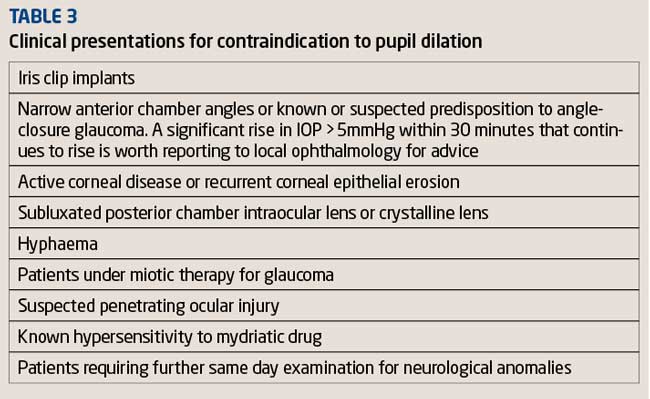
Contraindications to, and risk Factors for, pupil dilation
Although optometrists should be aware of the potential risk factors from the use of mydriatic drops, there are very few contraindications, since its use may be mandatory for the further investigation of conditions such as diabetes, glaucoma, sudden onset of flashes and floaters and high myopia. The potential risk of acute closed-angle glaucoma from using a mydriatic is rare and the possibility of precipitating an angle-closure glaucoma attack must be weighed against the importance of detecting ocular pathology. Patients should be assessed for narrow anterior chamber angles and where possible the angle should be further assessed with gonioscopy prior to dilation. Table 3 summarises recognised contraindications.
Conclusion
Optometrists regularly perform pupil dilation to comprehensively examine the ocular fundus as part of a comprehensive eye health examination where clinically indicated. They should familiarise themselves with the various mydriatic drugs available, have an understanding of their pharmacological effects and how best to utilise them depending on the patient.In all cases, consideration should be made regarding indications for use and risk factors involved when carrying out a dilated fundus examination. Good record keeping is essential when using any diagnostic agent and particularly when a patient declines pupil dilation; records should reflect this and it should be noted that the patient has been advised the importance of the need for further investigation to rule out any undetected pathology.
Procedure for dilation/mydriasis
1 History and symptoms
- Determine whether the patient has had any previous adverse reactions to the drug
- Determine if the patient reports any symptoms suggestive of angle closure
- Determine if the patient has any systemic condition or ocular disease that may be aggravated by the use of the drug
- Determine if the patient is taking any systemic medication that could interact with the drug
2 Advice to the patient
- Fully explain to the patient the importance of pupil dilation and why dilation is being performed
- Explain the potential the side effects for example, stinging on instillation, blurry vision for several hours and sensitivity to light/glare/difficulty in reading
- Advise the patient not to operate any heavy machinery or drive in this time if their visual acuity is reduced
- Inform the patient of the possible risks of dilation, eg inducing acute angle-closure glaucoma
3 Record keeping
- Note that informed consent was received prior to instillation of the dilating drops and the patient did not inform you of any previous known allergies. Note that the patient was informed of the possible side effects and risks and advised not to drive etc
- If available, give the patient a written information leaflet outlining the verbal information given regarding dilation, drug, precautions, possible side effects and what to do in an emergency
4 Pre-tests
- Assess the anterior chamber angle using van Herick, anterior OCT or gonioscopy (if available)
- Check corneal integrity
- Note tonometry
- Note visual acuity
- Note pupils – size, shape and reaction
- Note iris colour
5 Record keeping
- Select drug type and concentration carefully taking iris colour and patient age into consideration
- Check the minim for drug name, concentration, expiry date and batch number recording these details on the record card along with dosage and time of instillation
6 Instillation
- Instil one drop into the lower conjunctival sac with the patient looking superiorly to account for Bell’s reflex (the protective rapid upgaze when the eyes are approached unexpectedly)
7 Absorption
- Gently apply pressure to the lower nasal puncta to prevent uptake into the systemic circulation and enhance corneal absorption
- Monitor the dilation effects after a few minutes. It may be necessary to instil a further drop of the mydriatic. Note on the record card if a second drop was instilled and what time
8 Fundus examination
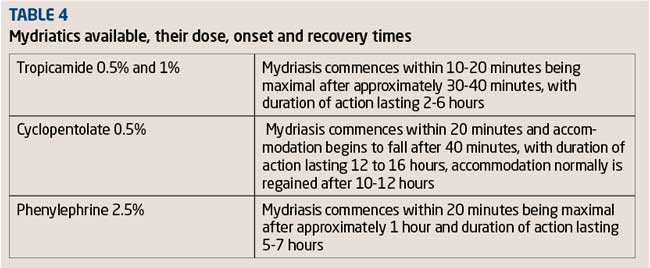
- Once maximum dilation is achieved (see onset and recovery times in Table 4) commence your dilated fundus examination
9 Measure angle and pressure
- Following examination and mydriasis, measure and note the anterior chamber angle and intraocular pressures
- Pressure rise of more than 5mmHg should be monitored until it returns to normal levels. If pressure continues to rise, seek advice of an ophthalmologist
- Angle-closure glaucoma precipitated through dilation with tropicamide is most likely to occur within an hour of initial instillation. If intraocular pressure has not risen significantly in the first hour, the probability of angle closure occurring is extremely low
10 Advice to the patient
- The patient should be warned again of the effects of dilation, sensitivity to light, no driving or operating of heavy machinery and of symptoms of an acute angle closure attack. Ensure they have an instruction leaflet for the procedure of what actions to take if symptoms occur (ocular pain, nausea, red eye, reduced vision)
- Patients are advised not to drive following dilation, because, although (high contrast) Snellen acuity is only mildly affected by the pupillary dilation, studies have shown that low contrast acuity is greatly reduced
Practical tips for improving the efficacy of dilation
The following practical tips may be considered to enhance the clinical effectiveness of pupil dilation:
- The higher concentration of mydriatic (1 per cent) should be used on patients with darker irides, due to the pigment binding of the drug
- Simple eyelid closure and digital occlusion of the tear duct for at least two minutes after eye drop instillation reduces systemic absorption of any topical drug by up to two-thirds
- Instillation of a topical anaesthetic prior to instillation of the mydriatic increases the speed of onset of both tropicamide and phenylephrine by enhancing corneal permeability and reducing irritation caused by the medication. It also prolongs recovery time
- Dilation of narrow angles is generally considered to be safer with an anti-cholinergic such as tropicamide. Phenylephrine 2.5 per cent increases the risk of pupil block, because of its mode of action
- Instillation of one drop of 2.5 per cent phenylephrine followed by one drop of tropicamide 0.5 per cent or 1 per cent is likely to give greater dilation than either drug used alone – maximising the effect on both the iris sphincter muscle and iris dilator muscle. This can be useful for patients whose pupils are difficult to dilate including patients with diabetes. Consideration should be given to patients with cardiovascular disease, in which case phenylephrine would be contraindicated
- In systemic disease and with concomitant drug therapies, tropicamide (0.5 per cent or 1 per cent) remains the mydriatic of choice as phenylephrine is frequently contraindicated
Model answers
According to the Medicines Act, what class of drug does phenylephrine come under?
B P
The neurotransmitter found at the neuroeffector junction of the sympathetic system is?
D Noradrenaline
Which of the following structures is supplied by the parasympathetic nervous system?
C Lacrimal gland vasoconstrictor muscles
Which of the following statements regarding mydriasis is TRUE?
D Sympathomimetics mimic noradrenaline at the a receptors causing pupil dilation
Which of the following clinical conditions does not contraindicate dilation?
B Neurological symptoms
Which of the following tests is NOT essential to conduct prior to dilation?
D Checking visual fields
Tina Patel practises in South London and is an assessor for the College of Optometrists