When needed, optometrists have access to a wide range of ophthalmic diagnostic agents available for them to use as specified under the Medicines Act of 1968. The use of these diagnostics agents, whether it is an anaesthetic, a mydriatic, a cycloplegic or a staining agent, are essential for executing further investigative techniques that may be required in an otherwise routine eye examination and/or assessing certain ocular complaints that a patient has presented with.
When working in optometric practice it is useful for optometrists to know which diagnostic agents are available to use, in what capacity they might be used (for example, using a mydriatic with cycloplegic properties to examine a child with visual symptoms) and what effect they will have on the patient.
This article looks at the cycloplegic effects of mydriatic diagnostic agents, neurotransmitter controls, the cycloplegic agents available to optometrists, the clinical indications and contraindications (if any) for cycloplegia, as well as a step-by-step guide to performing a cycloplegic examination.
What is cycloplegia?
In order to understand cycloplegia, mydriasis should first be briefly revisited (see also Optician 17.07.15). A mydriatic drug dilates the pupil by blocking the action of the iris sphincter muscle (antimuscarinics or parasympatholytics), or by stimulating the iris dilator muscle (sympathomimetic or adrenergic stimulating drug) (see Figure 1).
[CaptionComponent="2938"]
Antimuscarinic drugs not only produce mydriasis (which in this context might be considered an unwanted side-effect), but also paralysis of the muscles of the ciliary body (cycloplegia), by preventing access of acetylcholine to its receptor site.
The result of this is that the accommodative ability of the eye is impaired and therefore the patient’s near-vision becomes blurred. For this reason, they may be referred to as cycloplegics.
What cycloplegics are available to optometrists?
The ideal cycloplegic drug should be rapid in onset, produce an adequate depth of effect, be of adequate duration, ideally not have any mydriatic effect (however, as the parasympathetic system nervous system also innervates the pupillary sphincter muscle, cycloplegia is accompanied by mydriasis and, as a result, mydriasis is considered to be an unwanted side-effect that can cause photophobia), be absent of any side-effects, avoid any systemic or local toxicity and be reversible.
Several antimuscarinic agents have been used in the past, however only a few are now readily available for optometrists to use in mainstream practice.
All cycloplegics used by optometrists are prescription-only medicines (POMs) and some, such as atropine, are now only available for use and supply by additional supply optometrists and can be prescribed and used by independent prescribing optometrists.
Cyclopentolate
[CaptionComponent="2939"]
Cyclopentolate is the most common cycloplegic drug used in optometric practise. It does not elicit complete paralysis of accommodation but gives sufficient cycloplegia for the majority of cases. It is rapid in onset, has a short duration of action compared with other cycloplegics and has a greater intensity of effect. It is most commonly used in primary care practice in a preservative single use minim preparation (Figure 2), but is also available in a repeat use drop formulation (Figure 3). Some practitioners have found a spray formulation to be useful, especially when assessing babies or those with very poor cooperation.
[CaptionComponent="2940"]
Cyclopentolate is now the drug of choice for cycloplegic refraction in optometric practice. It is also used for dilating the pupil in anterior uveitis, for alleviation of ciliary spasm following corneal abrasion and for penalisation therapy in amblyopia.
Atropine
Atropine is a strong antimuscarinic extracted from a plant species called Atropa belladonna. Also known as Deadly Nightshade, extracts from this plant were used in the past as a beauty aid by women to make their pupils bigger, hence the ‘belladonna’ or ‘beautiful woman’ etymology. It is extremely toxic, potentially lethal if swallowed, and has a high risk of systemic adverse effects and, therefore, rarely used by optometrists.
It has a slow onset and is usually prescribed for instillation a few days before examination to achieve total cycloplegia. Recovery is slow and may take several days to a week.
Due to its toxicity, slow action and long duration compared with other cycloplegics, atropine is rarely used. It is also used for dilating the pupil in anterior uveitis, the alleviation of ciliary spasm following corneal abrasion
and for penalisation therapy in amblyopia.
Tropicamide
Tropicamide is most frequently chosen for its mydriatic properties rather than its cycloplegic effects, as it has minimal effect on accommodation because it does not penetrate well into the posterior chamber. However, some light-eyed and/or elderly patients may have disturbance of accommodation for a few hours after maximal dilation. It might be considered for use in an adult patient with a spasm of accommodation.
It is mainly used for mydriasis (short duration) with minimal cycloplegic effect. Increasing the dosage (1 per cent) or combining 0.5 per cent tropicamide with 0.5 per cent cyclopentolate will elicit a greater cycloplegic effect. It is used for patients in late teens or older.
Homatropine
Homatropine is a semi-synthetic alkaloid prepared from atropine; the base tropine obtained by hydrolysis of atropine is chemically combined with mandelic acid.
Homatropine is rarely used now. It does not produce as satisfactory a cycloplegia in children and is, therefore, usually restricted to the over-15 age group. Typically, it is used in managing any accommodative and iris spasm in anterior uveitis and the alleviation of ciliary spasm following corneal abrasion.
Clinical indications for cycloplegia
Cycloplegic examination may be indicated in some children and young adults in the following cases:
- Children with constant or intermittent esotropia on initial presentation
- In children and young adults with asthenopic symptoms
- In children and young adults with esophoria and latent hyperopia
- Fluctuating accommodation found during retinoscopy and subjective refraction
- In cases of accommodative insufficiency, accommodative fatigue, accommodative inertia and spasm of accommodation
- In cases of suspected pseudo myopia
- In cases where subjective refraction/retinoscopy is not viable due to disabilities
Contraindications to and risk factors for cycloplegia
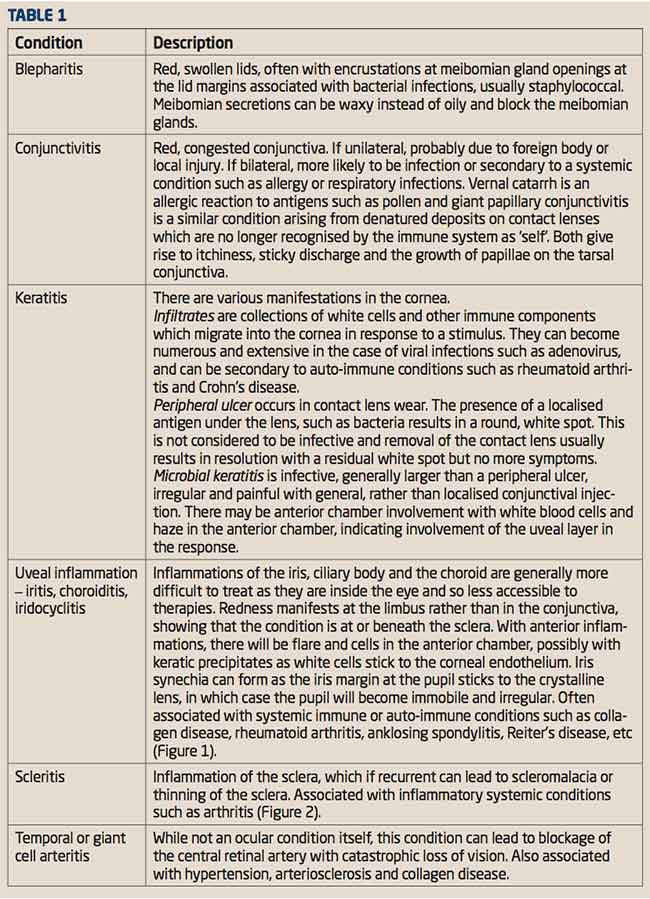
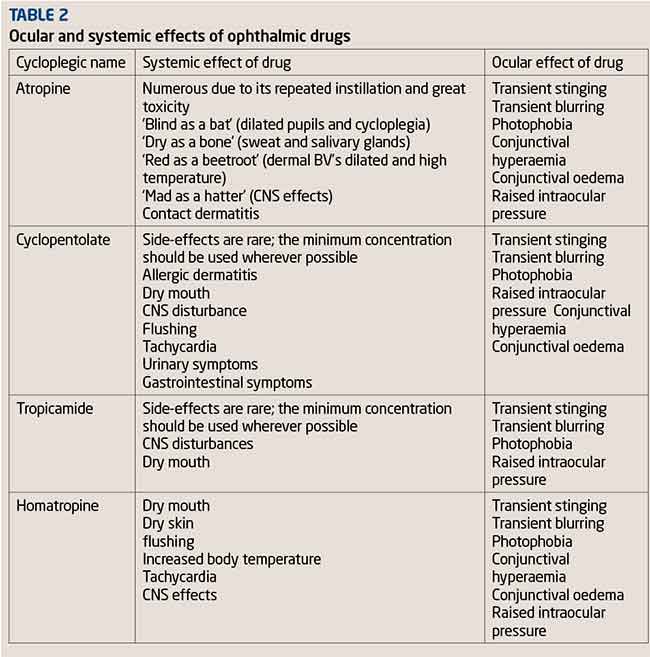
As with any drug, antimuscarinics are powerful agents that can cause adverse effects on several structures in the body. The principle of ‘as little as possible but as much as necessary’ should be applied to the use of all drugs. A cycloplegic drug should be selected according to the needs and requirements of the examination, the patient’s systemic health and any known sensitivity to a specific cycloplegic agent. Table 2 summarises possible side-effects of cycloplegics.
Cyclopentolate
Hypersensitivity to cyclopentolate or any component of the preparation is rare but possible. The drug is contraindicated in patients with confirmed or suspected angle-closure in whom an acute attack may be precipitated.
Premature and small infants are especially prone to central nervous system (CNS) and cardiopulmonary side-effects from systemic absorption of cyclopentolate and it is contraindicated in these patients. The elderly and children with spastic paralysis or brain damage are also more susceptible to CNS effects of cyclopentolate.
Atropine
Hypersensitivity to atropine or any component of the preparation is possible. Again, it is contraindicated in patients with confirmed or suspected angle-closure because an acute attack may be precipitated. The drug should be used with caution in patients with Downs syndrome and in patients receiving systemic anticholinergic drugs.
Tropicamide
Hypersensitivity to tropicamide or any component of the preparation is rare but possible. It is contraindicated in patients with confirmed or suspected angle-closure, since an acute attack may be precipitated. Multi-dose preparations contain benzalkonium chloride and should not be used when soft contact lenses are worn. Contact lenses should be removed prior to application, while the patient should wait at least 15 minutes before reinsertion.
Homatropine
Hypersensitivity to homatropine or any component of the preparation is possible. It is contraindicated in patients with confirmed or suspected angle-closure, as an acute attack may be precipitated.
Practical tips for improving the effects of cycloplegia
The following practical tips may be considered to enhance the clinical effectiveness of cycloplegia:
- Where possible, the lowest concentration of cycloplegic drug that will satisfactorily give the desired cycloplegia should be used on patients to avoid any adverse reactions
- Simple eyelid closure and digital occlusion of the tear duct for at least two minutes after eye-drop instillation reduces systemic absorption of any topical drug by up to two-thirds
- Obtaining a thorough medical and ocular history with particular emphasis on present medications, allergies, drug reactions and previous eye examinations will aid in the selection of cycloplegia drug
- Instillation of a topical anaesthetic prior to instillation of the cycloplegic diminishes the local stinging, irritation and lacrimation that often accompany cycloplegic drops
[CaptionComponent="2941"]
Cycloplegic refraction
A cycloplegic refraction is a procedure whereby a refractive error is determined while the ciliary muscles that control accommodation are temporarily paralysed with cycloplegic eye drops.
A cycloplegic refraction is indicated when patients present with symptoms of either decreased vision not corrected to a predicted level, variable and inconsistent end point of refraction, amblyopia, suspect latent hyperopia, suspect pseudomyopia, uncooperative/non-communicative patients, accommodative esotropia or uncompensated esophoria, there are significant risk factors linked to previous family ocular history and in suspected malingering. This procedure is also used in adults prior to refractive surgery to ensure the manifest refraction is correct.
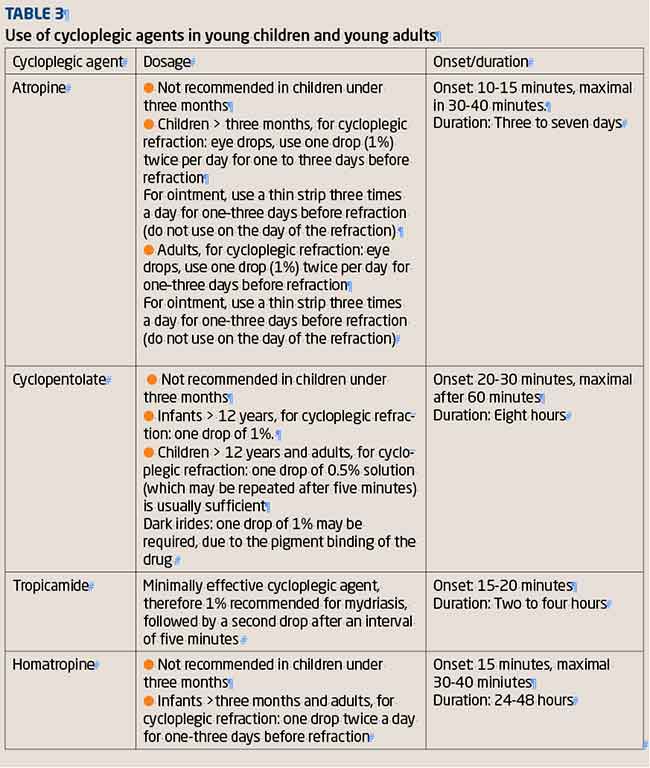
Table 3 summarises the choice of agent for any particular patient.
Pre-cycloplegic tests
As mentioned, the use of cycloplegic agents will only be indicated on a patient who presents with symptoms requiring a need for further detailed assessment. Once a non-cycloplegic examination has been conducted and it is determined that a cycloplegic assessment is required, various pre-cycloplegic tests should be performed in order to assess suitability and minimise the risk of any drug-related adverse reactions.
History and symptoms
- Determine whether the patient has had any previous adverse reactions to the drug
- Determine if the patient reports
- any symptoms suggestive of angle closure
- Determine if the patient has any systemic condition or ocular disease that may be aggravated by the use of the drug
- Determine if the patient is taking any systemic medication that could interact with the drug
Advice to the patient
- Fully explain to the patient/carer/guardian the importance of cycloplegic examination and why it is being performed. Obtain informed consent from the patient/carer/guardian
- Explain the potential side-effects, for example, stinging on instillation, near- vision blur for several hours, pupil dilation and sensitivity to light/glare
- Explain the potential duration of the cycloplegic drug (dependent on the drug and dose being used)
- Advise the patient not to operate any heavy machinery or drive at this time, as their visual acuity will be reduced
- Inform the patient of the possible risks of dilation, eg, inducing acute angle-closure glaucoma
- Advise the parent/carer/guardian to attend with the patient for the cycloplegic examination on a day when important visual tasks are not going to be performed
Pre-tests
- Check the manifest refraction with vision and visual acuity at distance
- and near
- Determine the binocular status with tests appropriate to the patient’s age (cover test, fixation disparity,
- ocular motility and accommodative function)
- Carry out an external eye examination including, slit-lamp examination, pupil function and note iris colour
- Carry out an internal eye examination including, ophthalmoscopy and intraocular pressures
- Check the amplitude of accommodation pre-cycloplegia (see further details)
Performing cycloplegic refraction
Select a drug that will provide adequate cycloplegia with minimal side-effects (see Table 3 for drug choice available in optometric practice). Instilling
drops can be daunting, especially in young children, and it is best to
explain the process of instilling drops without using words or terminology that might scare the child and/or parent (Figure 5).
[CaptionComponent="2942"]
As with all topical agents, note the expiry date, dosage and drug type that is being used, along with the number of drops being instilled and the time at which they are being instilled.
Prior to instillation, check and note the patient’s amplitude of accommodation. Since the parasympathetic nervous system also innervates the pupil sphincter pupillae muscle, cycloplegia is always accompanied by mydriasis, although mydriasis is not always accompanied by cycloplegia.
Therefore, looking at the amount of mydriasis alone is not a sufficient method for checking if adequate cycloplegia has been achieved.
Instill one drop in to each eye and ask the patient to either take a seat in the waiting room or return in 30 minutes, as this is the approximate time it will take for the commonly used drops to achieve maximum effect.
Recheck the amplitude of accommodation to ensure there has been sufficient reduction.
If this is not the case, instill another drop and recheck the results in 10 to 15 minutes.
Cycloplegic refraction is carried out in a similar fashion to dry static retinoscopy.
- Direct the patient to look at a distance target (duochrome) with both eyes open. For non-conforming patients, the patients may be encouraged to look directly at the retinoscopy light
- Due to pupil dilation and peripheral aberrations, the retinal reflexes may be distorted. Concentrate on the central 3-4mm reflex within the pupil. Some practitioners find autorefractors useful, especially if the pupil reflex appears difficult to interpret
- Determine the spherical/cylindrical error in the right eye first. If the patient has a strabismus, occlusion of the dominant eye will aid retinoscopy on the visual axis
- Repeat the procedure for the other eye
If possible, attempt a subjective refraction. However, due to spherical and ocular aberrations, the final visual acuity may be slightly reduced.
Practical tips for cycloplegic refraction
- When performing cycloplegia, concentrate on the central 3-4mm
- Anisocoria may sometimes, but not always, indicate unequal cycloplegia. In this case, it is wise to recheck for any residual accommodation in each eye. Add another drop if sufficient accommodation reduction has not been obtained
- Ignore the peripheral retinoscopic reflex motion due to aberrations
- The cycloplegic subjective refraction may differ due to pupil variations and spherical aberrations
- Movement of the light reflex in the peripheral parts of the dilated pupil may show positive or negative aberrations due to the differing refractive conditions in this area, as compared with the central axial region
- The use of a streak radioscopy can facilitate accurate location of cylinder axis, but spot retinoscopy has been advocated for paediatric use when using dynamic and near-retinoscopy techniques
- Due to the peripheral aberrations, a scissor movement of the light reflex may be observed on occasions, usually near the neutralisation point. Movement of the observers head forwards and backwards over a range of 25cm, giving first a ‘with’ then an ‘against’ movement, is a useful check that neutralisation has been attained
- Use the minimum light retinoscopy reflex possible in order to differentiate clearly the central and peripheral ret reflex
- In the presence of heterotropia, occlusion of the fixing eye will ensure retinoscopy is performed along the visual axis of the deviating eye
- Use a bracketing technique using +/- 1D spheres and +/- cylinders in order achieve reversal quickly
Prescribing after cycloplegic refraction
Following cycloplegic refraction, the results may differ significantly from the pre-cycloplegic findings. The final prescription given will depend on, what the patients needs are, what they will be able to adapt to and what will give them the best acuity and alignment.
It will be beneficial to arrange a further post-cycloplegic visit to assess the effect of the proposed correction on the patient’s binocular status.
The following are general guidelines to assist prescribing for common conditions:
- For patients with esophoria accompanied by hyperphoria, prescribe the minimum plus that allows the heterophoria to become compensated. Prescribe the maximum plus if binocular instability is noted
- For patients with esotropia under four years of age, prescribe the full refractive correction
- In older patients, prescribe closer to the manifest refraction to alleviate symptoms but without blurring the distance vision
- For patients who have not worn glasses, modify (reduce the plus) the prescription for adaptation purposes but avoid this if any eso component is found. It is better instead to encourage adaptation to the full plus prescription
Follow-up visits
It is likely that the patient will need to return for regular follow-up visits to reassess their vision when the final prescription is issued. The recall period will be dependent on the patient’s initial symptoms, if the prescription has been modified and how well the patient is adapting to the glasses.
Conclusion
Diagnostic agents are widely available for optometrists to use. Among these agents, the use of cycloplegics is indicated to accurately assess the refractive error and, in some cases, obtain a view of the fundus.
Cycloplegic refraction can be of great use in optometric practise, especially for cases involving latent hyperopia, esotropia and non-organic visual loss.
The advantages to be gained by using these drugs outweigh the possible adverse ocular and systemic effects that rarely occur. The least toxic drug and the lowest possible dose that will produce sufficient cyclopegia should be used.
Patient consent should be obtained and an in-depth explanation, including what to do in the event of an adverse reaction, should be given to the patient.
Complementing this advice with a patient leaflet regarding cycloplegia will also be helpful.
Tina Patel works at Moorfields Eye Hospital and is an assessor and examiner for the College of Optometrists