A good response to this exercise, with a fair representation from each of the registered professions. Key themes explored included:
• Awareness of professional responsibility regarding dry eye management
• Understanding the distinctive, varied nature of dry eye disease presentations
• Approaching management with a multiple approach strategy, and not a single-option approach such as ‘give drops’
In the source material, we were reminded of the TFOS DEWSII distinctions to reflect different presentations of dry eye disease (DED), as shown in figure 1.
Importantly, it was also highlighted that there usually exists a spectrum of DED, with a variable ratio of evaporative and aqueous deficient components of the disease. This is important and should be reflected in a stepped approach to management, as shown in figure 2.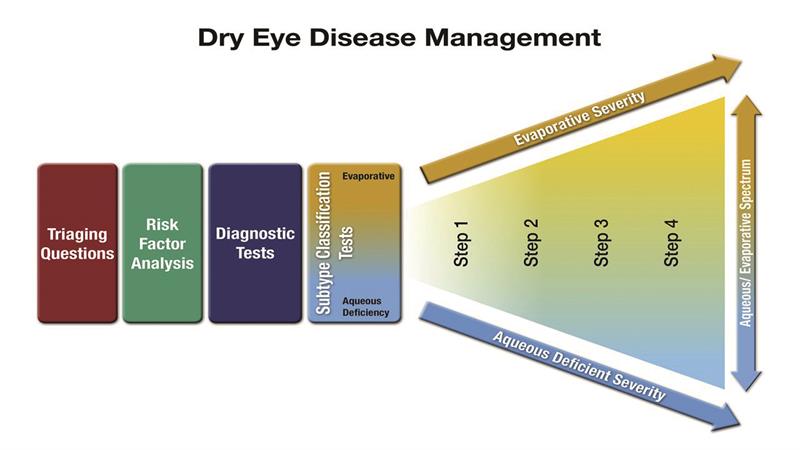 Figure 2 The TFOS DEWS II approach to managing DED
Figure 2 The TFOS DEWS II approach to managing DED
Case for Discussion
You were asked to consider the following: A 32-year-old woman arrives at your practice. She is concerned that, over the last few months, her eyes are becoming increasingly ‘dry and gritty’ towards the end of each day. She has never had an eye check before but had seen a television advertisement for some dry eye drops that had said to ‘consult your optician’.
• Can she be helped without booking in for an eye check?
• Can she be dealt with by a dispensing optician or contact lens optician?
• Assuming no systemic disease or medication contributing to her symptoms, what would be a systematic approach to the management of this patient?
Professional Responsibility
Though the vast majority of respondents recognised that an eye examination with an optometrist is definitely the right initial approach, there was a nice range of responses which tended to blend the first two of the three questions under discussion. Here is a sample of some of the responses.
‘After discussing this with my colleague we both agreed that we would advise the patient to have a full eye examination as she had never had an eye check before. I would explain to the patient that her symptoms of dry and gritty eyes would be assessed during the full eye examination so her main issue for attending would be addressed. We felt that it would be wise to perform a full eye examination and in fact in our practice the cost difference between this and a fitting appointment is negligible. As we both felt a full eye examination would be necessary, this would have to be performed by an optometrist hence the dispensing optician or contact lens optician could not deal with this.’
‘We both felt that it is always best to have a full eye check, as the many clinical tests will help assess the severity and type of DED. In an ideal world, every practice would run dedicated dry eye clinics. This is something we are looking to introduce in our practice. But a full history will always be the best starting point this is something a dispensing optician can help with.’
‘We both thought that an examination where a full history is taken and other diagnostic tests done would be required in order to determine the cause of her symptoms. While they may be dry eye, there are many other reasons that she may be experiencing symptoms, such as asthenopia, environmental, ocular surface disease, medications. Without an exam the Px may self-medicate and potential problems be missed. In addition, should it be a dry eye condition, it gives the opportunity to educate and treat accordingly. A dispensing optician would be able to advise why an exam would be advisable, though referral to an optometrist would be how it should be dealt with. A CLO would be able to examine the patient, but only if a contact lens (CL) wearer, and should refer to an optometrist for further examination if the symptoms continue when CL review and any CL related problems addressed is complete.’
‘In discussion with a colleague we both agreed that while the customer could be dealt with by front of house staff as she has not had an eye examination it would be advisable to book her in for one to fully assess the eyes first.’
‘I discussed this case with my dispensing optician colleague. He would try to refer the lady on to me or another optometrist at the practice but, if she declined, he would take a cursory look at her lids and conjunctivae, ask her if the symptoms were worse in a particular environment, eg towards the end of a working day and then suggest that she try using a modern formulation of dry eye drops such as Systane, Thealoz Duo or Hycosan. A contact lens optician would be better placed to advise with access to a slit lamp biomicroscope and use of staining dyes. He would recommend that if the drops didn’t relieve the symptoms then it would be wise if she did book an appointment for a full examination with an optometrist.’
‘As we are in the MECS system this patient would automatically be booked in for a MECS appointment. MECS would still be the answer here but, even without MECS, we would still prefer her to see an optometrist in case there was something else going on not just dry eye.’
Management Strategies
Thankfully, only a handful of respondents went down the ‘drops only’ route. Most, instead, adopted a multiple option approach, though there was some variation in these as might be expected from the deliberately vague nature of the discussion-prompting information offered. Here is a selection of answers.
‘I would start with the OSDI questionnaire to ascertain the history of her symptoms. This would allow me to rule out any trauma or more severe potential diagnosis (eg Sjögren’s) or the use of medicines which may cause dryness. If any of these questions revealed a suspect answer, I would advise her to have an eye test.
‘Her replies would guide my advice suggestions which might include the following:
• Suggest improved diet- including oily fish (omega-3)
• Suggest drinking more water and less caffeine
• Reduce VDU/digital device screen-time
• Remember to blink and create triggers to remind the patient to blink
• Reduce late nights (Harvey – good luck with that one!)
• Reduce contact lens wear (if appropriate)
• Consider tear replacement eyedrops, eg Thealoz Duo, to treat her symptoms’
‘We would educate the patient about hygiene, and recommend a lubricant and a heat pack and to return if the symptoms
persisted.’
‘She should be asked about lifestyle/hobbies health etc as there may be environmental issues contributing to the causes of her discomfort. In the diagnosis of the DED, tear film stability would be checked (using fluorescein) along with osmolarity and surface staining.
Checks on slit lamp of eyelashes, lids, checking for corneal swelling and ulceration and also anterior chamber flare are also important. If DED is diagnosed, then initially lid hygiene and eyebags/compresses should be discussed along with recommendation of a lubricant.’
‘The systematic approach would to be to firstly educate the patient as to what the condition is. What the possible causes could be and then recommend treatment and possible changes to their environments in both home and work. After a period of about a month recommend a follow up visit and review the case. At this point alternate treatments or onward referral may be made or the case may be closed.’
‘Along with the general eye health and vision being assessed, the optometrist can take into account her medication/environment/tear quality in relation to her presenting symptoms. TBUT and a slit lamp examination (using NaFl) along with evidence of MGD or LIPCOF. At this point, the practitioner can select, where appropriate, to employ a stage 1 staged/tiered management rationale to treatment which might include environmental advice/blinking exercises/hydration/use of rewetting drops/ hot compress or Eyebag treatment for MGD. A follow up appointment should then be booked for a month’s time (either with the optometrist or a dry eye practitioner CLO) where more specialised investigations could be employed; where applicable, such as tear osmolarity, MG condition/count using an infrared viewing technique. If the presenting symptoms have not abated, the Px treatment escalated up a stage. This might involve punctal occlusion, MG expression in conjunction with some/all of the previous treatments. Again, a follow up appoint would need to be made in after this consultation to assess progress or escalate onto a higher stage again.’
‘Management is ultimately aimed at restoring the homeostasis of the ocular surface by breaking the vicious cycle of the disease and offering long-term options to prevent a return to the vicious cycle and a resurgence of symptoms.
‘It is now generally believed that most people with symptoms relating to ocular surface disease (OSD) suffer from variable combinations of both abnormal meibomian gland function (evaporative eye disease or EDE) and tear underproduction (aqueous deficient eye disease or ADDE) rather than them being entirely separate conditions. Patients with DED have been shown to be over three times more likely to have evaporative dry eye than aqueous deficient dry eye and 30% of patients had both types.
‘The basis of effective management begins with accurate diagnosis. It is important to categorise an individual’s dry eye disease in terms of the degree to which EDE, ADDE and any other ocular surface conditions are contributing to the overall picture for that patient. The concept of determining the major causative factor is key to appropriate and effective management. While there are treatments which are indicated for multiple aspects of DED, others are specific to one particular aspect of an individual’s ocular surface condition.
‘The example under discussion seems likely to be early stage symptoms and so the recommended first stage step approach seems appropriate, namely:
• Education regarding the condition, its management, treatment and prognosis
• Modification of local environment
• Education regarding potential dietary modifications (including oral essential fatty acid supplementation)
• Identification and potential modification/elimination of offending systemic and topical medications
• Ocular lubricants of various types (if MGD is present, then consider lipid containing supplements)
• Lid hygiene and warm compresses of various types
‘These steps show the most evidence-based staged management of DED depending on severity. The exact nature of an individual’s DED will dictate the range and number of management options selected from one or more steps.’
