Over the coming year, optometrist Kirit Patel presents a monthly series looking at the presentation and management of a number of interesting patient presentations, including conditions as varied as visual field loss, myasthenia gravis and pituitary adenoma. Each will detail the patient episodes and offer useful background details about the condition being discussed.
Optic disc drusen
Optic disc drusen are often difficult to detect. Also, they can masquerade as a variety of other conditions including optic neuritis, papilloedema, and can impact upon nerves and vessels to induce effects that may suggest diseases such as primary open angle glaucoma and anterior ischaemic optic neuropathy. In this article I describe four patients of varying ages the range of effects from this congenital lesion.
Case 1 – Crowded optic disc
An 11-year-old Chinese patient attended for a routine eye examination with no obvious complaints. Refraction was normal, with no need for spectacles, and no colour vision defect was found.
Fundus examination revealed a very hyperaemic right optic disc, the redness central to nasal with a temporal crescent seen. The left optic disc appeared normal. Autofluorescence revealed no fluorescence suggesting no obvious evidence of drusen at the nasal edge. OCT showed a raised right optic disc along the nasal aspect, with a maximum 469 µ lift on the superior nasal aspect (see figure 1). The diagnosis was probable buried disc drusen along the nasal aspect.
Case 2 – Apparent optic neuritis
A 35-year-old policeman booked an emergency appointment on late Saturday afternoon having experienced constant pressure behind the left eye and some pain on movement of the eye. He had recently been suffering from an upper respiratory tract infection.
His vision was 6/6 in each eye and a colour test revealed protanopia, bilateral and congenital so not of recent onset. There was also no desaturation of red colour.
Examination revealed the following (see figure 2):
- Right optic disc showing mild cupping and a temporal pigment crescent. Nasally the disc appeared to have a blurry margin.
- Left optic disc gave the appearance of central disc swelling and peripapillary myelination.
- OCT revealed slightly raised nasal portion of the right disc while the left showed a centrally raised optic disc.
- Nerve fibre layer analysis revealed normal thickness in the right eye, while the left appeared to be disproportionately thick. The right RNFL thickness was 112 microns superiorly and inferiorly, while the left was 187 microns thick superiorly and 176 microns thick inferiorly.
A tentative diagnosis of optic disc drusen in the left eye was made, but it was also felt prudent to refer the patient to the ophthalmologist to eliminate optic neuritis on the basis of eye pain on movement of the eyes.
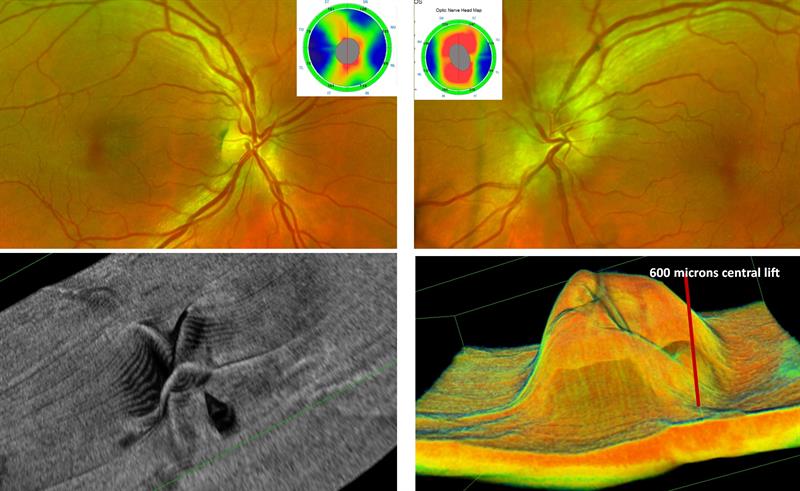
Figure 2: Left eye (right image) showing apparent myelination, no cupping and swelling confirmed by OCT (thickness maps and 3D). The right disc (left image) appears normal
Case 3 – Visual field loss with apparent AION
A 62-year-old female was seen for the first time at the practice with no obvious complaints. Her visual acuity was 6/7.5 in each eye.
Fundus examination revealed the following (see figure 3):
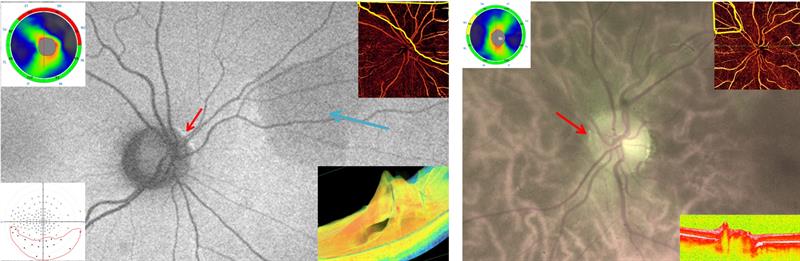
Figure 3: Right disc (left main) with nasal autofluorescence (red arrow). The RNFL map (inset top left) shows superior thinning and would explain the inferior field loss (inset bottom left). OCT angiography (inset top right) shows capillary loss and the 3D OCT (inset bottom right) suggests nasal tilting and elevation. The left eye (right main) shows nasal autofluorescence, slight RNFL thinning, some nasal capillary loss and nasal elevation
- Right optic disc revealed a yellowish deposit in an arc on the nasal aspect of the disc, and an area of retinal atrophy about two disc diameters away. Autofluorescence at the right disc was indicative of disc drusen.
- Visual fields assessment (full field, 120 degree) revealed an inferior scotoma at 30 degrees from fixation.
- OCT revealed some loss of superior nasal retinal nerve fibres with no associated ganglion cell loss, so appearing to rule out glaucoma as a cause of the field defect.
- OCT angiography revealed capillary loss in line with the retinal nerve fibre loss.
- The left disc showed slight glistening on the nasal aspect of the optic disc but no loss of retinal nerve fibres or visual fields.
Visual evoked potential (VEP) testing assesses the functioning of the visual pathway. The amplitude of the signal gives an indication of the number of axons conducting signals along the visual pathway, while the latency translates to the status of the myelin sheath. Our patients VEP (figure 4) revealed reduced amplitude of the left optic nerve compared to the right, even though drusen were apparently more prevalent on the right optic disc. There was also a delay in the latency of both eyes, and the left in particular appeared to show a delayed response with low contrast stimuli.
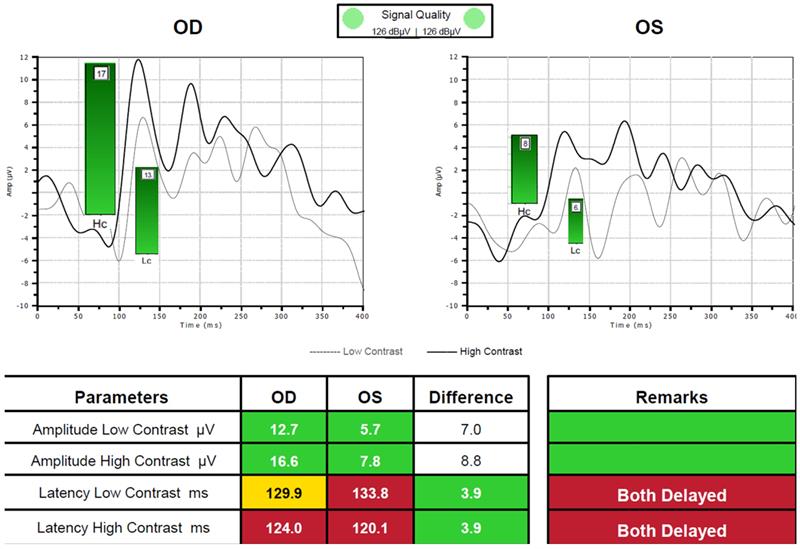
Figure 4: Visual evoked potential results showing delayed transfer for both high and low contrast targets. Left eye (with more drusen) showed lower amplitude signal (suggesting reduced signal transfer along the visual pathway)
Case 4 – Compressive lesion
A 71-year-old Asian came in for a routine eye examination. It was her first visit to the practice and she had no obvious complaints. She had undergone bilateral cataract extraction some five years earlier.
Ocular examination showed the following:
- Vision was 6/6 in each eye and N5 with a +2.00D add.
- No pupil abnormalities detected, with equally rounded and reactive pupils to light and convergence.
- Implants were in situ and clear of any posterior capsule opacification.
- Vitreous appeared attached to both the optic discs.
- Right optic disc appeared hyperaemic and raised on the nasal aspect with tortuous blood vessels emanating from the disc (figure 5). No spontaneous venous pulsation was observed.
- Possible drusen on the inferior nasal aspect of the right optic disc were detected and also implied on the OCT image. The OCT showed the vitreous still intact and not liquefied
- Left optic disc appeared normal with regular vessel arrangement. Similarly, the left vitreous is intact.
- Ishihara revealed no red-green defect.
- Visual fields assessment revealed no visual field defect.
Tentatively, we diagnosed optic disc drusen and a possible optic disc coloboma in the right eye. It was also thought necessary to refer her back to her consultant to ensure there was no obvious compressive lesion behind the right optic disc.
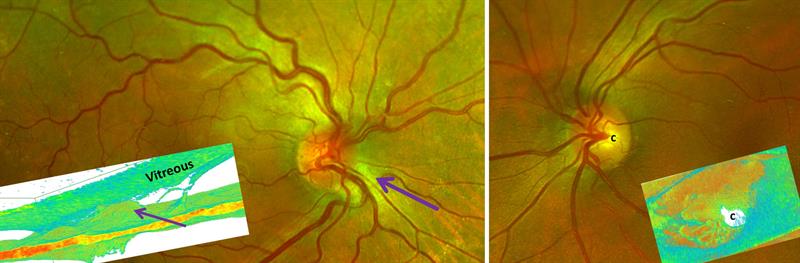
Figure 5: Right eye (left main) shows a hyperaemic and inferiorly raised disc (elevation noted by purple arrow) with drusen and an intact vitreous. Left disc (main right) appears normal with clear central cupping
The consultant was also surprised at the changes in the optic disc, which seemed to have occurred over the intervening five years since her cataract operations, and immediately carried out an MRI contrast media (gadolinium) scan of both the brain and the orbits. The results proved negative, so no brain tissue oedema, no pre-septal or retrobulbar abnormalities, no optic nerve or chiasm size or signal abnormality, no pituitary lesion, and the dural sinuses as well as the major intracranial arteries were all patent.
The conclusion was possible optic disc drusen and no compressive lesion.
Discussion of Optic Disc Drusen
Optic disc drusen are globular, often calcified, hyaline (glassy or translucent) bodies located within the optic nerve head. Drusen are relatively common, found in 1 to 2% of the population, and are thought to be inherited in an autosomal dominant pattern, though no specific gene has yet been found. The implied inheritance means it is advisable to screen siblings of any patient presenting with disc drusen.
Disc drusen are bilateral in 75% of cases, and the excrescence is more often seen on the nasal half of the disc. Drusen usually become visible after the age of 10 but sometimes appear at the surface at a younger age than this. Before this, they are buried and may give an appearance of papilloedema. At this stage, the drusen do not affect central vision so might easily be missed except, though compression of the retinal nerve fibres may result in a field defect. This abrupt, painless loss of peripheral vision may be detected with fields assessment of older patients and can mimic primary open angle glaucoma. A rare complication of disc drusen is the development of a choroidal neovascular membrane. Optic disc drusen have an association with angioid streaks in 25% of patients.
Optic disc drusen are thought to be a collection of 40 or 50 colloid bodies bunched into small nodules ranging from 5 to 100 µ in diameter. Histologically, they consist of needle-like calcium deposits in the nerve fibre axons and represent degenerative axonal by-products. It is postulated that small scleral foramina (pre-lamina cribrosa) impede the axoplasmic flow of protein, lipid and mitochondria leading to stasis. These degenerate into globules of mucoprotein and mucopolysaccharides, which later calcify and then leak into the interstitial spaces. Continuous calcification of these small microbodies causes them to coalesce to form groupings of drusen. Over periods of time there is then an associated pre-laminar spongiform oedema and eventually atrophy of the adjacent retinal ganglion cell axons.
VEP testing measures the signal registered at the occipital region in response to visual stimuli. Retinal ganglion cell axons in an early phase of mechanical stress may, instead of degenerating, enter into a state of functional impairment. This is evident by reduced VEP amplitude due to nerve loss or conduction block and fewer nerves being used. Also, demyelination due to drusen would cause a latency delay as the nerve impulse travels slower.
Appearance:
- Pseudo-papilloedema or anterior ischemic optic neuropathy appearance due to optic disc being elevated with blurred disc margins (see figure 6).
- Crowded disc appearance due to obstruction of the physiological cup by small buried drusen which elevate the optic disc.
- Glowing appearance, confirmed with autofluorescence, especially on the nasal aspect with retro-illumination due to large and more diffuse multi-lobular yellowish nodular drusen.
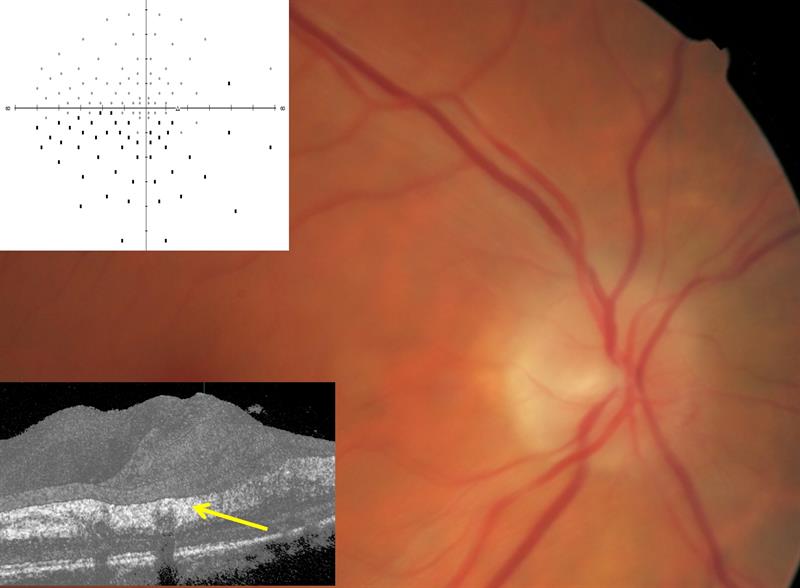
Figure 6: A true anterior ischaemic optic neuropathy showing a swollen optic nerve head with blurred margins and an oedematous nerve fibre layer as shown on the OCT scan by the yellow arrow. The fields assessment shows a typical altitudinal defect following a non-arteritic AION in a 50 year old male with systemic hypertension
Symptoms:
- Transient visual loss in 5 to 10% of patients due to transient disc ischaemia.
- Visual field defects predominantly in the inferior quadrant reported in 70% of eyes with visible drusen and in 30% of patients without visible drusen.
- Nerve fibre defects which do not often correspond to the position of the drusen on the optic nerve.
- Compression of the optic nerve and its vascular supply predisposes the nerve to disc haemorrhages and ischaemic optic neuropathy.
- Deep and buried drusen tend not to demonstrate nerve fibre layer thinning. Calcification can be confirmed by ultrasound.
- Drusen enlarge with age, and this enlarging colloid body within a crowded space that cannot expand exacerbates mechanical stress on the delicate structures within the pre-laminar scleral canal. Both nerve fibre thinning and field losses do slowly progress over time.
Eye care in the community
1 Optic disc drusen
2 Vein thrombosis
3 Sports Injuries
4 Ehlers-Danlos syndrome
5 Myasthenia gravis
6 Total sight loss
7 Shingles, molluscum contagiosum and VKC
8 Field loss
9 Sjogren’s disease
10 Optic neuritis
11 Glaucoma monitoring
12 Iris melanoma
