
We usually assume that, having referred a patient for suspect glaucoma, their continued care should remain at the remote glaucoma clinic. In this article, I present examples of where a vigilant optometrist can successfully co-manage the patient in the community setting.
Case 1
A 43-year-old patient, SC, had been under the care of a local eye clinic where her ocular hypertension in the right eye was monitored. She had been monitored every six months for over 20 years. She was born with a capillary haemangioma (port wine stain, figure 1) on the right side of the face. She was currently being prescribed timolol 0.25%, to be used twice a day in the right eye only.
 Figure 1: Right hemi-facial capillary haemangioma
Figure 1: Right hemi-facial capillary haemangioma
At her last appointment at the eye clinic, it was noted that her pressures were 16mmHg in the right eye and 14mmHg in the left eye. No mention of corneal thickness was made, and her visual fields were deemed to be normal. It was decided they should now monitor SC on an annual basis.
The patient was quite happy for our practice to monitor her annually, as she wanted to ensure that she did not suffer any field or vision loss in future. She also wanted to be sure that she was on the correct treatment.
Clinical findings
• Right hemi-facial capillary haemangioma (port wine stain)
• Right hemi-facial hypertrophy
• IOP
• R: 19mmHg
• Corneal thickness 524 microns (adapted IOP, 20mmHg)
• L: 17mmHg
• Corneal thickness 520 microns (adapted IOP, 18mmHg)
• Cup disc ratios
• R 0.7 and L 0.6
• Anterior examination: Normal, wide angles
• Gonioscopy: grade 4 open angle and mild pigmentation in the trabecular meshwork (figure 2)
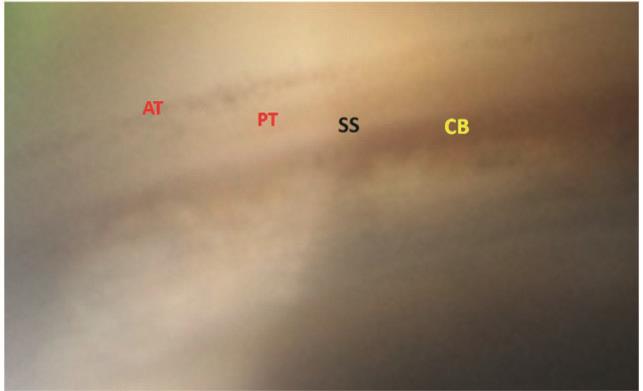 Figure 2: Gonioscopy showing all structures indicative of an open angle, and low-level pigmentation (AT; anterior trabecular meshwork, PT; posterior trabecular meshwork, SS; scleral spur, CB: ciliary band)
Figure 2: Gonioscopy showing all structures indicative of an open angle, and low-level pigmentation (AT; anterior trabecular meshwork, PT; posterior trabecular meshwork, SS; scleral spur, CB: ciliary band)
• OCT retinal nerve fibre analysis revealed thinning of the superior layer in the right eye by 10 microns to 96 microns (red arrow, figure 3). The left eye nerve fibre layers remained unchanged.
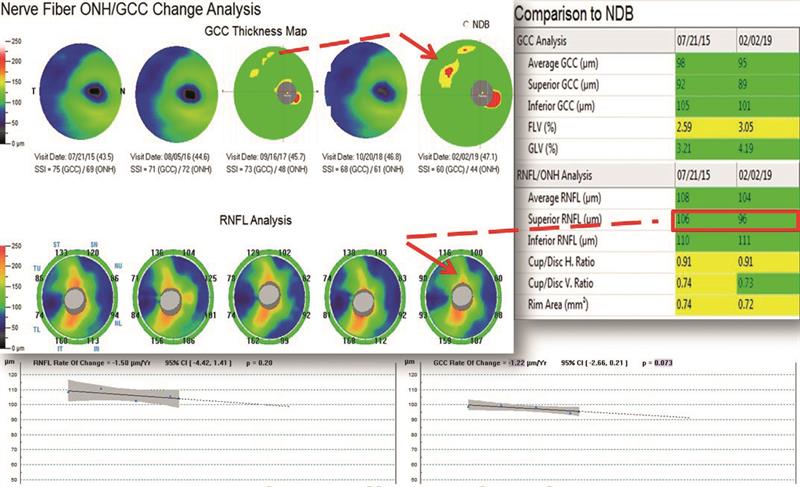 Figure 3: OCT showing superior thinning of both the ganglion cell complex (upper red arrow) and the superior retinal nerve fibre layer (lower arrow) between 2015 and 2019.
Figure 3: OCT showing superior thinning of both the ganglion cell complex (upper red arrow) and the superior retinal nerve fibre layer (lower arrow) between 2015 and 2019.
• Visual fields showed GHT within normal range in both eyes. The mean deviation was worse at -3.07db in the right eye compared to -1.52db in the left eye (figure 4).
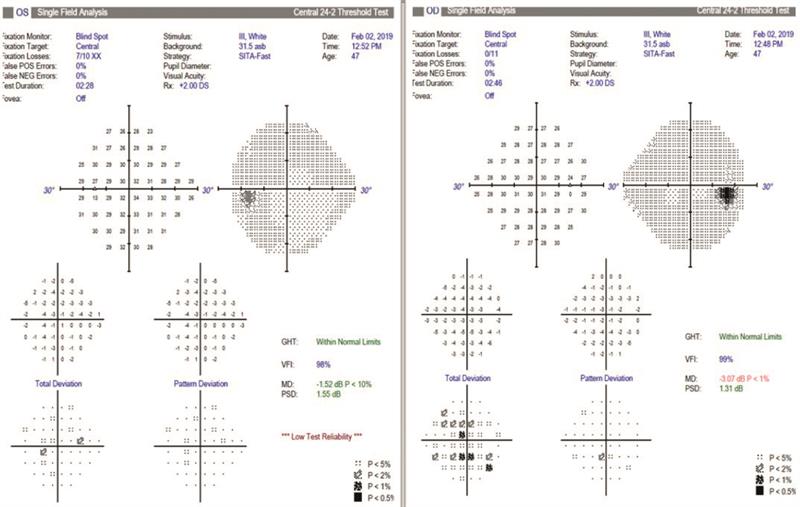 Figure 4: Normal visual fields for both eyes. The mean deviation is lower for the right eye, while fixation is less reliable for the left. This was likely due to fatigue.
Figure 4: Normal visual fields for both eyes. The mean deviation is lower for the right eye, while fixation is less reliable for the left. This was likely due to fatigue.
magnitude to be D low in the right eye compared to the left eye, indicating that the ganglion cells were dysfunctional or under stress due to the raised pressures.
Management
The patient was rightly concerned about whether she was on the correct treatment for her ocular hypertension, and was worried about developing glaucoma. I discussed my findings with her, explaining that the ERG showed the ganglion cells in the right eye appeared dysfunctional (figure 5). Fortunately, there was only minimal loss of the ganglion cell complex (GCC) on OCT. The retinal nerve fibre layer was starting to show some thinning on the superior aspect and it would be prudent to try alternative drops or SLT to reduce the pressures further.
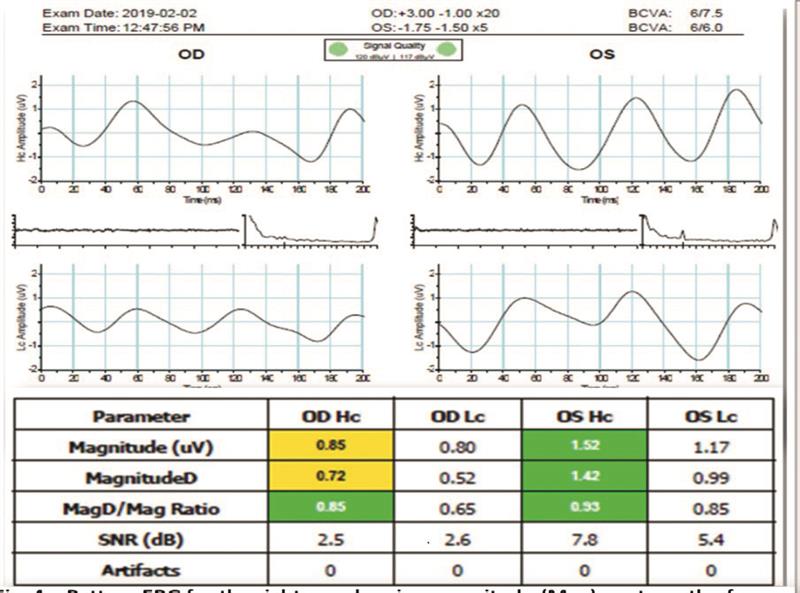 Figure 5: Pattern ERG of the right eye shows the magnitude (Mag) of the response from the ganglion cells to be reduced. This is further indicated by the consistency of the waveform not being in phase. The results suggest the right ganglion cells are dysfunctional or distressed. Left eye responses appear normal.
Figure 5: Pattern ERG of the right eye shows the magnitude (Mag) of the response from the ganglion cells to be reduced. This is further indicated by the consistency of the waveform not being in phase. The results suggest the right ganglion cells are dysfunctional or distressed. Left eye responses appear normal.
SC was referred to an alternative glaucoma specialist who agreed with our findings and changed the drops to Cosopt (a combination of dorzolamide and timolol) to be used twice a day for the right eye. The specialist was to reassess the patient in three months to ascertain whether the asymmetry was, in fact, longstanding or whether it represented a progressive change. This despite the fact that we had evidence from the OCT of a progressive change in the GCC over a four-year period.
Discussion
Capillary haemangioma, also known as infantile haemangioma, strawberry haemangioma, port-wine stain or strawberry naevus, is a benign, excessive growth of blood vessels, predominantly found on the face and neck. They present at birth, and often disappear in the first six months of life. In fact, 50% disappear by the age of five and 90% disappear by the age of nine.
There are two types of haemangiomas:
- Capillary haemangioma; found in the outer layer of the skin and often called strawberry birth marks (figure 6)
- Cavernous haemangioma; found within the muscle cone, but can be found anywhere in the orbit. They can affect normal development of the eye leading to amblyopia and glaucoma if involving the eye itself or optic neuritis and or atrophy due to compression of the optic nerve.
 Figure 6: Small, persistent capillary haemangioma on the wrist.
Figure 6: Small, persistent capillary haemangioma on the wrist.
- Staining of the forehead and or scalp
- Haemangioma involving the surface of the brain, on the same side as the surface lesion. Involvement of the brain can be serious, leading to seizures or developmental problems. Therefore, all children with port-wine stains should have an MRI scan to rule out brain changes.
Case 2
An 82-year-old male, VC, had been under my care for 25 years. Over the past five years his pressures had risen until, in 2016, they had reached R 27mmHg and L 29mmHg. His corneal thickness had been measured as R 601 microns and L 592 microns, so his adapted IOPs were R 23mmHg and L 24mmHg. At this point, I referred via his general practitioner for ocular hypertension.
Secondary care
The glaucoma monitoring clinic (that employs glaucoma specialist optometrists and ophthalmologists) subsequently sent letters to the patient saying that his pressures were well controlled with latanoprost eye drops. The last letter, sent in 2018, stated that corneal thicknesses were yet to be measured and that his IOPs with the drops were R 18mmHg and L 19mmHg. Cup/disc ratios were deemed to be 0.4 each eye. Next visit to the clinic was planned in six months’ time where, it was stated ‘gonioscopy would be performed by a named doctor’. The patient had reported some blurred vision at this last appointment, but no explanation for this had been offered. I saw him at our practice in 2018.
Clinical findings
• Visual acuity; 6/12 R and L
• Anterior assessment; narrow angles right and left (figure 7).
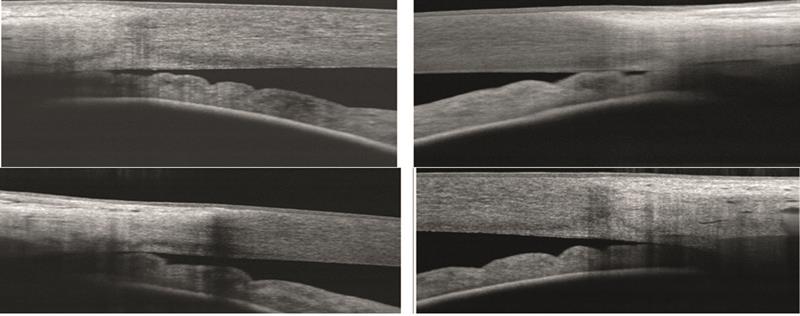 Figure 7: Anterior OCT showing (top) narrow angles in the right eye, temporal and nasal, and (bottom) similar narrowing in the left. Likely cause, enlargement of the crystalline lens.
Figure 7: Anterior OCT showing (top) narrow angles in the right eye, temporal and nasal, and (bottom) similar narrowing in the left. Likely cause, enlargement of the crystalline lens.
• IOPs:
• R 24mmHg (CCT 601 microns, adapted IOP 21mmHg)
• L 28mmHg (CCT 592 microns, adapted IOP 25mmHg).
• Fields were inconclusive due to poor test reliability
• Cup/disc ratio: R 0.5, L0.7
Management
It was explained to the patient that the vision was blurred due to bilateral cataract. The growing cataracts were pushing the iris forward and narrowing his angles, and thereby increasing his IOP. The patient agreed to have the cataracts removed by a private consultant, both to improve the vision and to see any benefit of reduced IOP once angles re-widen.
Post-operative findings
• Unaided visions; 6/7.5 each eye
• Angles; wide open right and left (figure 8)
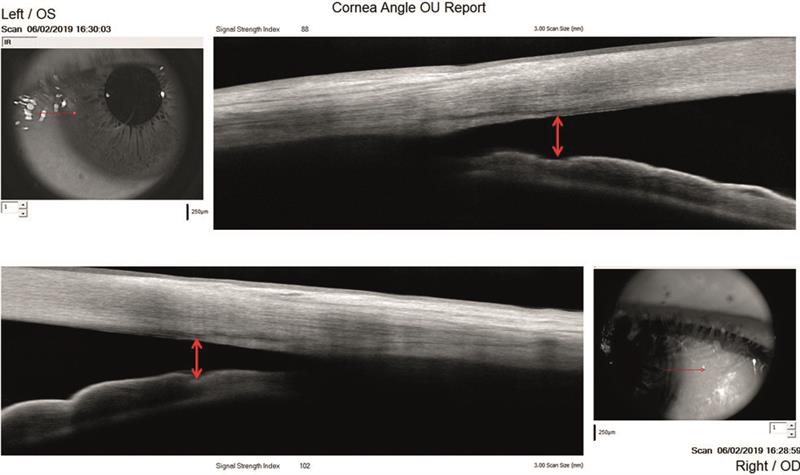 Figure 8: Anterior OCT showing nasal and temporal angles wide open after cataract removal (left top, right bottom)
Figure 8: Anterior OCT showing nasal and temporal angles wide open after cataract removal (left top, right bottom)
It is hoped that future loss of ganglion cells, retinal nerve fibre loss and eventual field loss might now be avoided.
Discussion
Ocular hypertension is the term used to describe the state where there is elevated IOPs without any measurable loss of ganglion cells or retinal nerve fibres, and no associated loss of visual field.
I agree with other modern thinkers who think of glaucoma as a process defined by the following findings:
- Distress or dysfunction of the ganglion cells as measured by pattern ERG
- Loss of ganglion cells as measured by OCT ganglion cell complex
- Thinning of nerve fibre layers shown by OCT RNFL analysis
- Increase in optic disc cupping
- Subsequent loss of visual fields.
- Eventual optic disc atrophy.
Case 3
An 89-year-old male patient, JC, was first seen at our practice in 2017 where he attended for a routine eye examination with no visual
complaints.
Clinical findings
• Visual acuity; R and L 6/9 with spectacles
• Low grade cataract R and L
• Pseudoexfoliation R and L
• Gonioscopy:
• Moderate pigmentation R and L
• Grade 4 wide open angles R and L
• IOPs:
• R 20mmHg (CCT 522 microns, adapted IOP 22mmHg)
• L 17mmHg (CCT 517 microns, adapted IOP 19mmHg)
• Cup/disc ratios; R 0.7, L 0.50
• Disc appearance; healthy R and L
• OCT; no loss of ganglion cells or retinal nerve fibres
Management
The patient was informed about his pseudoexfoliation, the
possibility of IOP rise and subsequent glaucoma. JC decided not to be referred at this stage, so instead we decided to monitor on a
six-monthly basis.
Clinical findings (at six months)
• IOPs:
a. R 29mmHg (CCT 522 microns, adapted IOP 31mmHg)
b. L 22mmHg (CCT 517 microns, adapted IOP 24mmHg)
• Visual fields:
a. R; GHT outside normal, mean deviation -3.74dB
b. L; GHT borderline, mean deviation -4.15dB
• Optic disc cupping; unchanged at R 0.7 and L 0.5
• OCT; no loss of ganglion cells and no loss of retinal nerve fibres.
• ERG contrast sensitivity; distress or dysfunction of the ganglion cells indicated by a ratio of Mag D to Mag of 0.50 in the right eye and 0.49 microvolts in the left eye (figure 9).
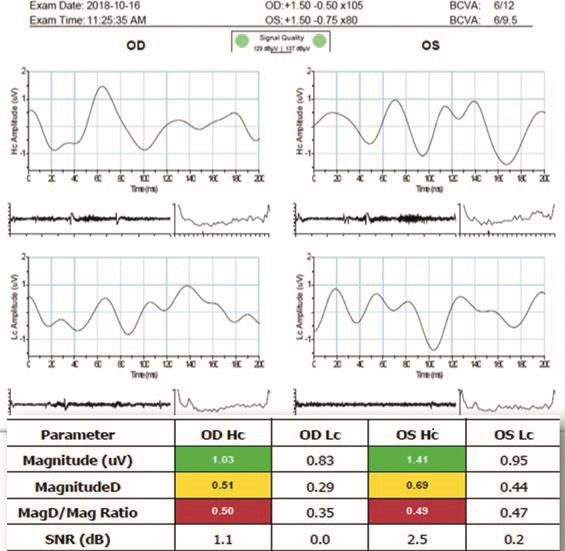 Figure 9: ERG showing a poor waveform for both eyes indicative of sub-optimum performance of the retinal ganglion cells. The magnitude at high contrast (HC) appears within the normal range, but the magnitude D shows a poor response. D measures 150 waveforms to see if they are responding in phase or not. The ratio of the magnitude to D is, therefore, outside normal limits at a paltry R 0.50 and L 0.49 mV.
Figure 9: ERG showing a poor waveform for both eyes indicative of sub-optimum performance of the retinal ganglion cells. The magnitude at high contrast (HC) appears within the normal range, but the magnitude D shows a poor response. D measures 150 waveforms to see if they are responding in phase or not. The ratio of the magnitude to D is, therefore, outside normal limits at a paltry R 0.50 and L 0.49 mV.
Considering the high IOPs (especially in the right eye) due to pseudoexfoliation together with the measurable distress of the retinal ganglion cells, a decision was made to refer the patient to the eye clinic. We cannot refer patients directly to the eye clinic, and instead they have to be referred to a triaging centre for initial assessment.
The patient was unhappy with the response from the triaging centre, with cancelled appointments and an insistence on him having another field test undertaken without any initial examination. Our patient got utterly fed up, and in the end we referred him privately to a consultant ophthalmologist who measured the IOPs now to be R 38mmHg and L 30mmHg. He was immediately prescribed latanoprost eye drops. A month later, his pressures were still elevated, at R 28mmHg and L 22mmHg. At this point, brinzolamide (Azopt) eye drops were added to the mix.
The consultant then suggested that we re-examine the patient in three months with all the tests and he would try and get the patient under his NHS clinic. A shared care scenario was instigated for the benefit of the patient. Figure 10 shows improvement in the ERG after six months of treatment.
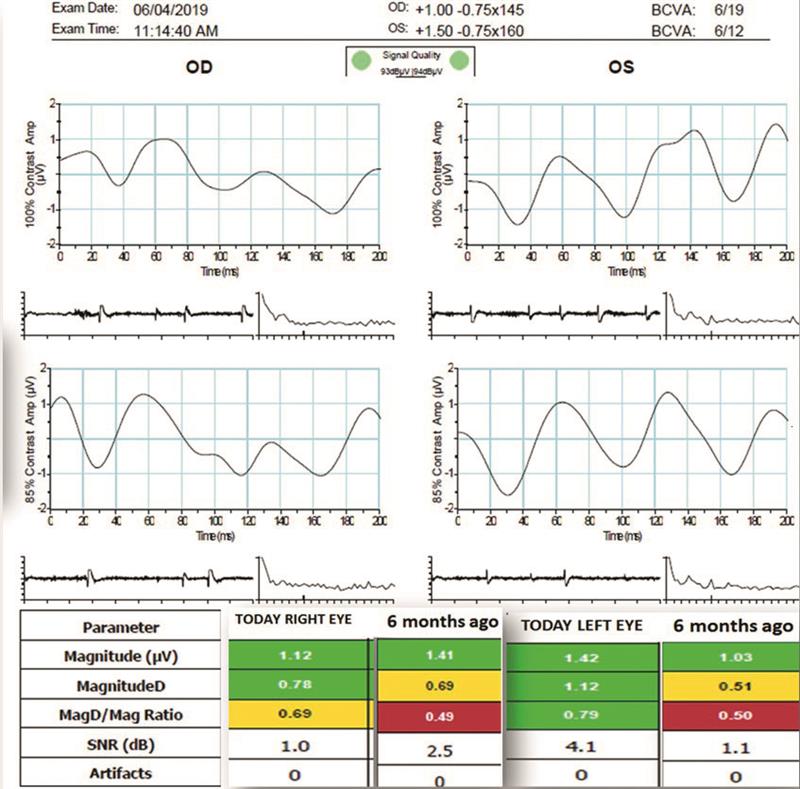 Figure 10: Six months after the introduction of topical hypotensives , there is a much improved waveform for the left eye. The magnitude is much improved, while D is higher. The Mag D/Mag ratio appears normal in the left eye and is improving in the right.
Figure 10: Six months after the introduction of topical hypotensives , there is a much improved waveform for the left eye. The magnitude is much improved, while D is higher. The Mag D/Mag ratio appears normal in the left eye and is improving in the right.
Discussion
Pseudoexfoliation syndrome (PEXs) is a systemic disorder where fibrillar extracellular material, thought to originate from abnormal basement membranes, is deposited throughout the body, including throughout the cardiovascular system. Some studies suggest that pseudoexfoliation may lead to an increased risk of heart attack, stroke and dementia. There are also reports of increased sensorineural hearing loss in patients with PEXs.
In the eye, the fibrillar material is deposited on the anterior capsule and is similar to amyloid. Amyloid deposits comprise insoluble fibrous proteinaceous material. The fibres are often described as ‘elastic-like’, and differ in composition and structure from most elastic fibres in the body. It is thought that the epithelium cells of the iris, ciliary body and crystalline lens produce the pseudo exfoliative amyloid-like material.
Causes of PEXs are not properly known. Predisposing factors are thought to include ultraviolet light and high altitude exposure. Recent studies have demonstrated that PEX syndrome is associated with changes in the lysyl oxidase-like protein 1 gene (LOXL1) found on human chromosome 15 (15q 24-25). Alteration of the LOXL 1 gene leads to a reduction in elastin cross-linking and so is a major pathophysiological component of the pseudoexfoliation syndrome.
Once thought to be confined to those of Scandinavian origin, PEXs is also prevalent in the Bantu tribe of South Africa (at 8.2%). In the Indian subcontinent, the prevalence is between 6 and 7%. In Norway the prevalence is 6%, while in England and France it is 5%. In Scandinavian countries, PEX syndrome accounts for half of all open angle glaucoma cases, while in the Bantu tribe it accounts for 20% of glaucoma cases.
Pseudoexfoliation syndrome is three times more common in women than in men. PEXs is almost always seen in patients over the age of 50 years, and with increasing age the PEXs incidence rises steadily. However, it is not part of the normal ageing process. A study in Norway noted a 15-fold rise in PEXs over a 30 year period, from 0.5% prevalence at 50 years of age to 7.9% at 80 years of age. In Iceland, a further study reported a 10% annual increase for both open angle glaucoma and PEXs in patients over the age of 50 years.
Slit lamp bio microscopy of a patient with PEXs will almost always reveal fibrous material deposits at the iris pupillary margin. The presenting signs are more pronounced unilaterally, but careful observation will reveal similar changes in the fellow eye albeit less pronounced.
Dilation should reveal three distinct zones on the anterior lens capsule (figure 11), namely:
- A central ‘bulls eye’ zone marked by a white ring of fibrillar deposit
- A mid-peripheral clear zone
- A peripheral ring of fibrillar material with striations projecting towards the centre – best seen on pupil dilation
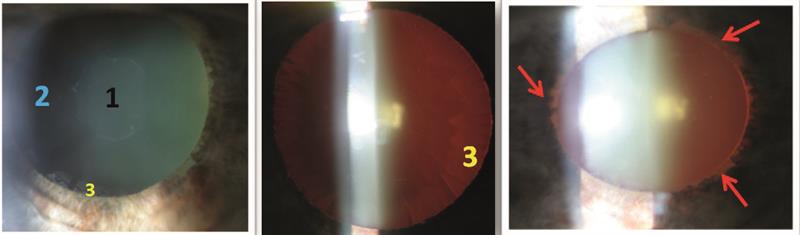 Figure 11: Pseudoexfoliation syndrome appearance showing 1; central bullseye fibrillary deposit, 2; corneal haze, 3; cortical deposition. Also note the transillumination of the pupillary margin (red arrows)
Figure 11: Pseudoexfoliation syndrome appearance showing 1; central bullseye fibrillary deposit, 2; corneal haze, 3; cortical deposition. Also note the transillumination of the pupillary margin (red arrows)
transillumination defects located at the pupillary margin (red arrows in figure 11) and not in the iris mid-periphery. This translucent zone is created by the iris rubbing against the anterior surface of the lens. Scraping removes the pseudoexfoliative material, as well as giving a secondary removal of melanin from the iris pigment epithelium at the pupillary margin. This leaves a saw-tooth appearance at the pupil margin due to peri-pupillary iris atrophy (loss of pigmented ruff). This is a fourth distinct observation in PEX syndrome.
Gonioscopy reveals moderate to severe pigmentation of the trabecular meshwork. Pigmentation will be seen both in the posterior as well as the anterior part of the meshwork (figure 12). The anterior meshwork is demarcated by Schwalbe’s line and, anterior to this, the Sampaolesi line.
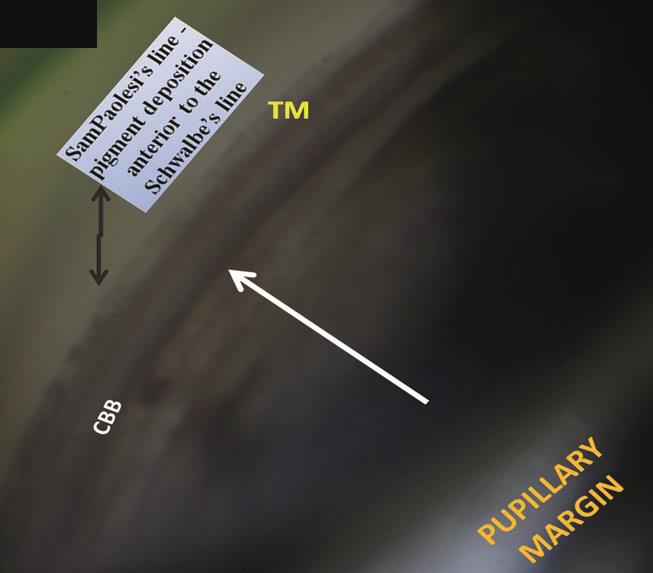 Figure 12: Starting at the pupil margin and working towards the white arrow at the peripheral iris, the iris root is attached to the dark ciliary body band (CBB). Then the faint white band of the scleral spur can be seen, then the homogenous brown posterior trabecular meshwork (TM) and the non-pigmented anterior TM. When the latter is heavily pigmented, it is described as a Sampaolesi line (suggestive of PEXs)
Figure 12: Starting at the pupil margin and working towards the white arrow at the peripheral iris, the iris root is attached to the dark ciliary body band (CBB). Then the faint white band of the scleral spur can be seen, then the homogenous brown posterior trabecular meshwork (TM) and the non-pigmented anterior TM. When the latter is heavily pigmented, it is described as a Sampaolesi line (suggestive of PEXs)
