
The TFOS DEWS II classification is: ‘Dry eye is a multifactorial disease characterised by loss of tear film homeostasis with tear film instability and hyperosmolarity as well as ocular inflammation and ocular surface damage, and neurosensory abnormality play etiological roles.’
Daily in practice we have patients, especially the elderly, who complain of dry eyes. For them the solution is to lubricate and all our instructions on lid hygiene, hot compresses and supplements usually fall on deaf ears. It can be frustrating for us practitioners as the patient will usually contact their GP and be prescribed eye drops that are not ideally suitable for their dry eyes. Drops with hyaluronic acid or carbomethyl cellulose with high molecular weight or cross-linked applied four to six times a day are most appropriate.
In essence, in practice I tend to segregate patients into categories of whether we are able to treat them or whether they need medical care. Patients with Sjörgen’s, Lupus and Ehler-Danlos should be seen by rheumatologists and ophthalmologists. Patients with tear deficiency should again be in the realms of eye specialists who would be able to fit punctum plugs to retain tears. Patients with acne rosacea should either be under the care of a dermatologist or their medical practitioner.
Setting up a dry eye clinic is not rocket science and it is imperative that we both identify dry eye patients and we have at our disposal fluorescein dye and a slit lamp to get a basic idea. How we at Radlett Opticians conduct our dry eye clinic is as follows:
- Identify dry eyes.
- Identify other conditions associated with dry eyes.
- Fluorescein tear break up time.
- Slit-lamp assessment of the anterior segment.
- Measure tear osmolarity.
- Accurate measurements using the SBM System IDRA:
- Interferometry.
- Non-invasive tear break up time.
- Tear meniscus.
- Meiobography.
- Blink quality.
- Manage the dry eyes and associated conditions.
- Finally, treatment.
I will run through some of the items listed above with diagrams so they will be easier to understand. The most important equipment we feel helps practitioners and patients is the IDRA and the ICP software, which gives us a meaningful results in a traffic light pattern. Once we have shown the patients their dry eye issues then we are able to give a long-term treatment with intense pulse light treatment (IPL). For our soft contact lens patients who suffer from dry eyes we sometimes move them to orthokeratology lenses as they benefit from day time relief from dry eyes.
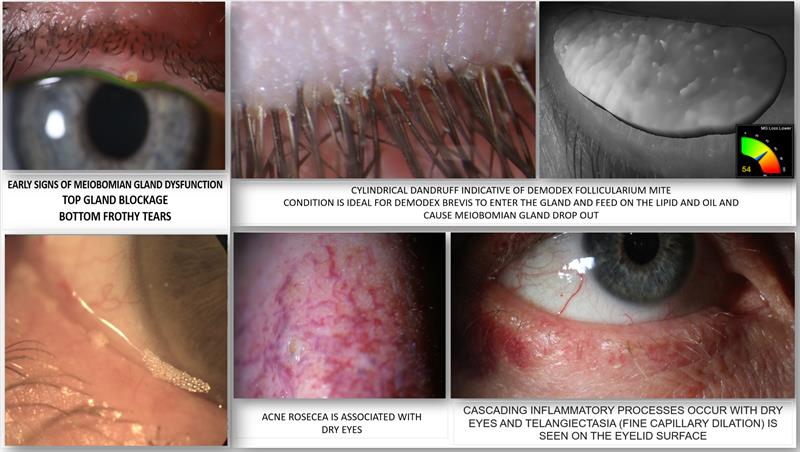 2: Identify other conditions associated with dry eyes: slit-lamp vital
2: Identify other conditions associated with dry eyes: slit-lamp vital
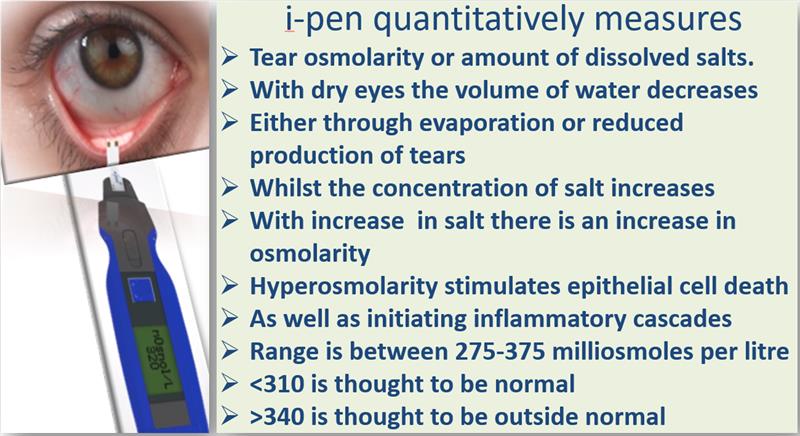 5: Measure tear osmolarity
5: Measure tear osmolarity
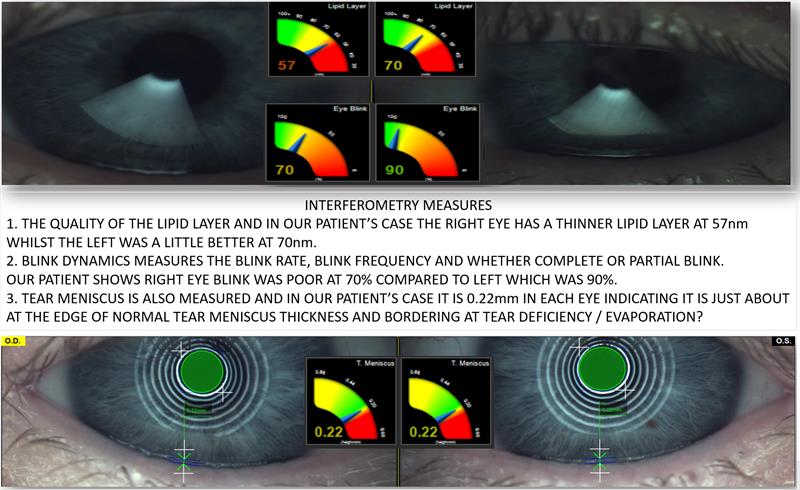 6: Accurate measurements with idra and sbm system:
6: Accurate measurements with idra and sbm system:
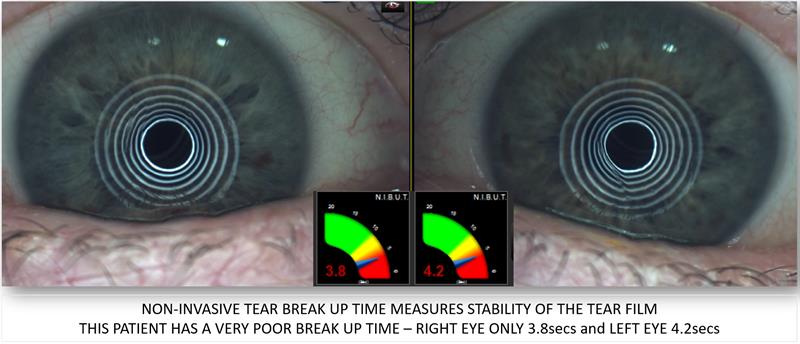 6a: Non-invasive tear break up time – Gives contact time for tears to remain on the corneal surface
6a: Non-invasive tear break up time – Gives contact time for tears to remain on the corneal surface
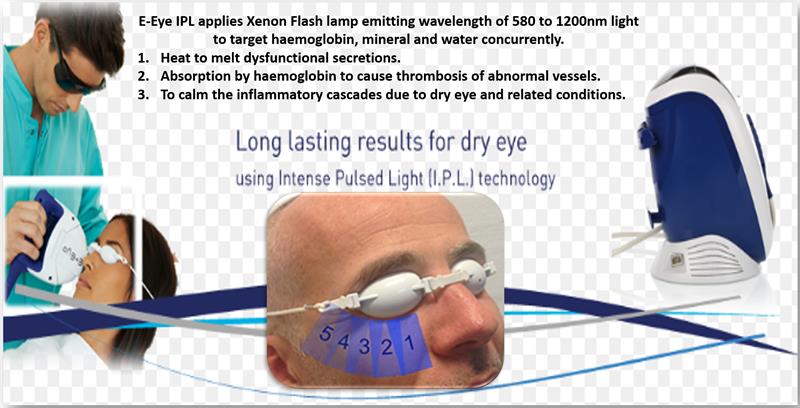 8: Treatment – We use E-Eye IPL treatment to stimulate the meibomian glands and allow it to produce a good quality lipid layer. The other advantages of IPL treatment are to kill the demodex mites as well as helping relieve abnormal vessels on the eyelid margins (telangiectasia). Finally, IPL is thought to provide relief from inflammation and neurogenic pain
8: Treatment – We use E-Eye IPL treatment to stimulate the meibomian glands and allow it to produce a good quality lipid layer. The other advantages of IPL treatment are to kill the demodex mites as well as helping relieve abnormal vessels on the eyelid margins (telangiectasia). Finally, IPL is thought to provide relief from inflammation and neurogenic pain
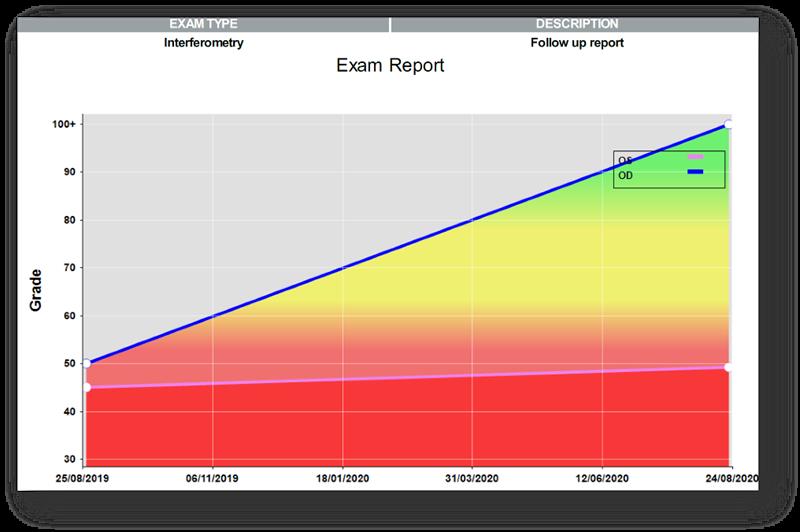
Results after treatment: ICP software is able to provide a follow up after treatment. One example is the interferometry shown below depicting a big improvement in the right eye a year later following treatment. The left eye shows no appreciable improvement.
In summary, an optometrist is able to diagnose dry eyes and associated conditions and should be well placed to advise the patient correctly and able to treat them with variety of drops and wipes. IPL treatment offers patients a long-term solution to their dry eye issues.
Kirit Patel is an optometrist in independent practice in Radlett, Hertfordshire.
