
There are so many webinars and online events at present that it is a real pleasure when you come across one that really stands out. Such a case was the recent online talk arranged by Thea Pharmaceuticals as part of its ongoing eye care education programme. Professor Christine Purslow, Thea Head of Medical Affairs in UK & Ireland, had managed to pin down for an hour the estimable Professor Harwaz Hossein who, as consultant ophthalmologist and renowned corneal specialist, is a key member of the team at the Southampton NHS Trust and University. Southampton is fast becoming a key centre for Covid-19 research and management, and this is now more widely known since the artist Banksy recently gifted a painting of NHS Heroism now to be found hanging in the hospital corridor (figure 1).
Not post-Covid yet
An initial audience poll of the 400 or so taking part found that 44% were currently undertaking clinical work at the slit-lamp, but with personal protective equipment (PPE), 34% were planning to do so soon and just 22% had yet to confirm any plan to do such work. The threat from SARS-CoV-2 infection from such work was highlighted by Hossain, initially by a short tribute to Li Wenliang, the ophthalmologist in Wuhan who first blew the whistle on the severity of the viral disease Covid-19, despite government resistance, and who sadly died soon after. His death serves as a reminder that eye care professionals have a particular risk of infection as, even though the ocular route for viral infection is a low risk one, it is significant. Also, Hossain cited two papers highlighting patients whose first symptom of Covid-19 is a viral conjunctivitis. The point here was that all of us are likely to see a first presentation of Covid-19 in the coming months or years.
PPE
Much of the rest of the session focused on PPE. Different types of mask, as long as they are well fitted, will reduce the risk of virus being spread from the wearer (figure 2). The speaker then showed some excellent videos from the American Academy of Ophthalmology which used blue light and fluorescent dye to show droplet, and therefore viral, spread under different
conditions.
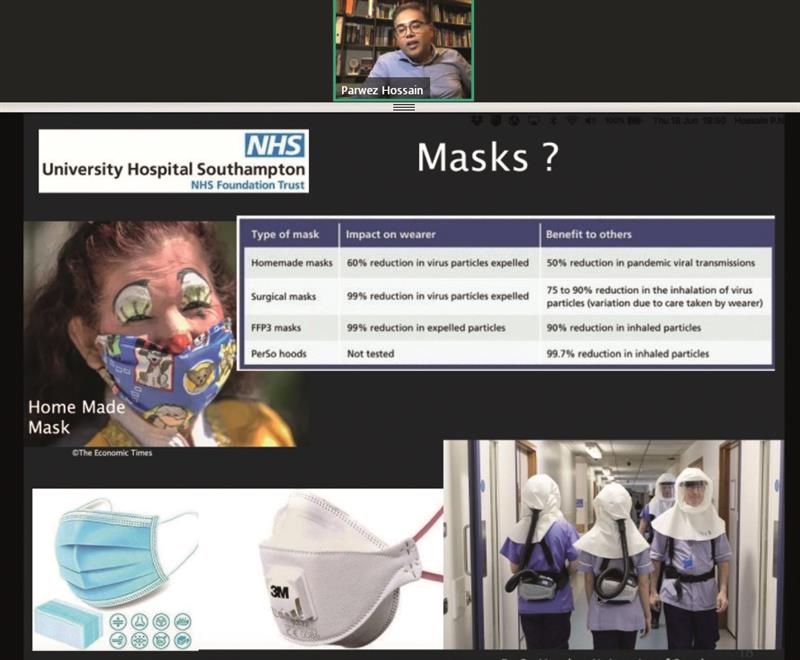 Figure 2
Figure 2
Firstly, it is clear that the smaller slit lamp breath shields offer little resistance to a sneeze, cough or even speech-spread spray. However, larger shields restrict patient contact for thorough assessment. Though distance between patient and practitioner may be maintained by the use of various camera adaptations, this may also restrict the thoroughness of the examination. For example, the all-important lid eversion would be impossible.
The videos then showed the viral spread when just the patient or the practitioner is masked or when the patient has a poorly fitting mask. It is clear that well-fitting N95 masks on both results in minimal droplet spread and so minimal risk of infection (figure 3).
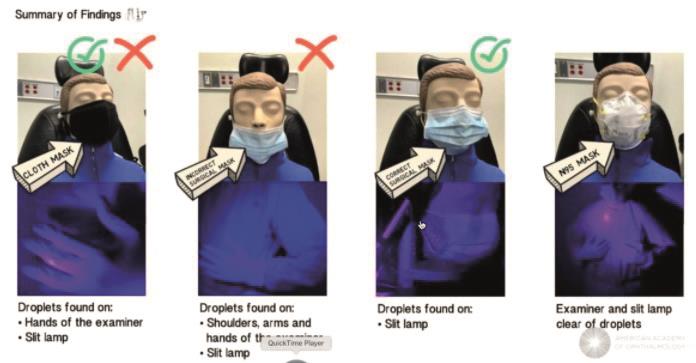 Figure 3
Figure 3
One issue raised both at this point, and later as a common thread through the questions from the audience, was of eye protection. It is important to keep the eyes protected and Hossain recommended the use of some of the more comfortable wraparound style safety specs available from companies like Norville. Steaming up is still a problem, but having as tight a seal around the specs with the face was important for minimising infection.
Most of the remainder of the presentation reflected some of the interesting and challenging cases managed in Southampton and included an excellent pictorial record of the repair of a corneal ulceration/perforation with a synthetic disc being glued into place. Of the many clinical pearls during this discussion, we learned that contact lenses may be applied from gloved hands – but the glove must be completely dry for it to be successful. Also, with adequate PPE, techniques that may be potential sources of aerosol, such as lacrimal syringing or Blephex lid abrasion, should be quite safe.
Main Points
This excellent and entertaining session carried a key message. Viral transmission is a real risk and, with Covid-19 having a high fatality rate, ‘we need to stay safe.’ Though virtualisation is possible, it ‘has its limitations – we still need to do face-to-face examinations.’
However, patients can be safely seen with the correct use of PPE and ‘there have been no reported cases [of infection] when wearing full PPE, even when treating severe Covid-19 positive patients.’ Or, as the professor put yet more succinctly, ‘you can’t go wrong with the right PPE.’
The audience supported this view – a final poll revealed 97% knew that PPE is essential to protect both the patient and the practitioner.
• For information about future events, go to
www.thea-pharmaceuticals.co.uk.
