
I hope you enjoyed our recent special supplement on myopia and its management (see Optician 03.12.21). One feature summarised the findings of the Northern Ireland Childhood Errors of Refraction (NICER) study and subsequent research, which has led to the development of some essential resources to help clinicians when dealing with myopic and likely-to-be myopic patients. Dr Sara McCullough (figure 1), a research associate in Optometry and Vision Science based at Ulster University, has been integral to this important work, so I caught up with her recently to find out more about her research.
Bill Harvey: The NICER study began in 2006. Could you give an overview of its scope and aims?
Sara McCullough: The initial aim of the study was to update the evidence on the prevalence of refractive errors in the UK, with a particular interest in investigating whether the prevalence of myopia had risen in contemporary children. Previously the only robust report on the refractive error profile of children living in the UK was by Sorsby et al in the 1960s,1 so an update was long overdue. There was also an increasing interest in the myopia epidemic that was occurring elsewhere in the world, and therefore we (and by ‘we’, I really mean Professor Kathryn Saunders, the lead on the NICER study and Dr Julie McClelland) were interested in whether this increase was occurring among children living in the UK.
We were then lucky to receive College of Optometrist funding to extend the research into a longitudinal study. Initially, this was to review the participants again three years later and then we received subsequent funding to review the same children at six and nine years after their baseline eye examination. This meant we had data from the younger cohort, children aged between six to seven years and 15 to 16 years, and the older cohort, aged between 12 to 13 and 21 to 22 years.
The NICER study is now the largest study of its kind in the UK and Ireland, a study whose aim is to examine prospectively how children’s eyes change throughout childhood, adolescence and into early adulthood.
BH: Am I right in thinking your own work has focused on using data from the NICER study to look for predictors of future myopia and myopic progression? If so, when did your involvement begin?
SM: Yes, we have been able to look at predictors for future myopia in those children who aren’t myopic and whether a child is likely to be a fast or slow progressor once myopia has onset. We were able to do this from the nine-year longitudinal data set.
When the NICER Study commenced in 2006, I was still an undergrad. Dr Lisa O’Donoghue conducted the first phase of the study for her PhD research, Phase 2 was carried out by Dr Karen Breslin for her PhD and subsequently me and Dr Lesley Doyle carried out Phases 3 and 4 respectively for our post-doctoral work. So, there has been a lot of people involved, all very grateful for the funding and support from the College of Optometrists.
It really needed a team effort with such a large study, spanning over 11 years of data collection, with Professor Kathryn Saunders leading the project from the outset. Using the data from the nine-year data set, we’ve developed a tool for eye care practitioners This is called the PreMO (Predicting Myopia Onset and progression) risk indicator. But more of that later.
BH: Could you explain a little more about what data were gathered and how you were able to interpret this to indicate myopia prediction strategies?
SM: For the initial assessment, over 1,000 children were carefully recruited using random cluster sampling to obtain two cohorts aged between six and seven years and between 12 and 13 years. This is critical for the NICER project, as these are not children volunteering for clinical trials or children tested as part of hospital or community eye services and, as such, reflect what is happening in the underlying general population. We had the help of an epidemiologist to determine how we should sample children to reflect this appropriately.
We recruited the children through the help of the school system, and carried out data collection during the school day, on school premises, for almost all of the study. By phases 3 and 4, the older cohort had left school and so we had to locate other sites to test them at. These included local church halls and football clubs where easy access helped to encourage continued participation. At each time point in the study, we assessed refractive error using open field autorefraction under cycloplegia, measured ocular biometry using the Zeiss IOL Master (figure 2), and assessed visual and oculomotor status. We also asked the participants and their parents questions about their family history, lifestyles and environment.
 Figure 2: Assessing ocular biometric data with the Zeiss IOL Master
Figure 2: Assessing ocular biometric data with the Zeiss IOL Master
BH: So, which predictive metrics are you confident we should look for in practice?
SM: The nine-year data analysis revealed several clinical metrics that were predictive of future myopia. The key features, unsurprisingly, were as follows:
• Family history of myopia. If a child has at least one myopic parent, they are 6x more likely to become myopic by the age of 16 years compared to a child with no myopic parents. Cross-sectionally, the NICER study results also show that, at age 12 to 13 years, a child was at approximately a 3x increased risk of myopia with one myopic parent, increasing to over 7x when both parents were myopic, when compared to a child with no myopic parents.
- Refractive status at a young age. Children aged six to seven years who are not currently myopic, but who have a spherical equivalent refractive error of less than +0.75DS of hyperopia under cycloplegia, are highly likely to become myopic by 9 to 10 years of age.
- Axial length. Children with axial lengths of greater than or equal to 23.19mm at age six to seven years are those who are most likely to develop myopia by nine to 10 years of age. Likewise, for every additional mm of axial length at age six to seven years, a child is 2.5 times more at risk of future myopia.
Unfortunately, when we started the NICER Study in 2006, little research had been done in relation to the amount of time a child spent outdoors, so this wasn’t included in our earliest questionnaires at Phase 1.
We were also able to generate growth charts for change in axial length with increasing age (figure 3). These are similar to what health visitors use to monitor children’s growth in terms of height and weight and are divided into centile curves, with the 50th centile being average eye growth. These can be a really powerful way to determine whether a child’s eyes are growing normally or not. Children who had longer eyes in the 75th centile or above were more likely to become myopic, but adding to this, we noticed those children who demonstrated eye growth that did not follow along a centile line, eg jumping from the 75th to 90th centile, were not following normal eye growth and this seems to be a signal that myopia is likely to occur within the next few years. It is good to see that modern biometers are incorporating these types of growth data to support practitioners in monitoring eye growth (figure 4).
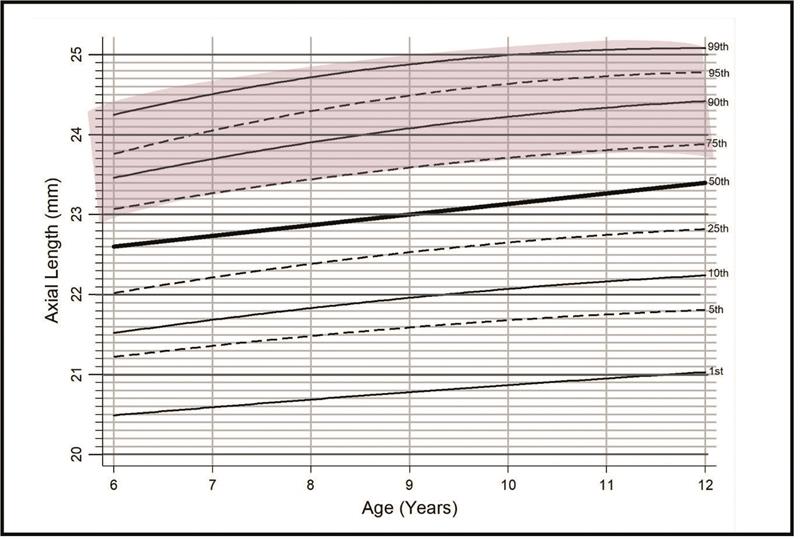 Figure 3: Axial length chart for patients aged between six and 12 years
Figure 3: Axial length chart for patients aged between six and 12 years
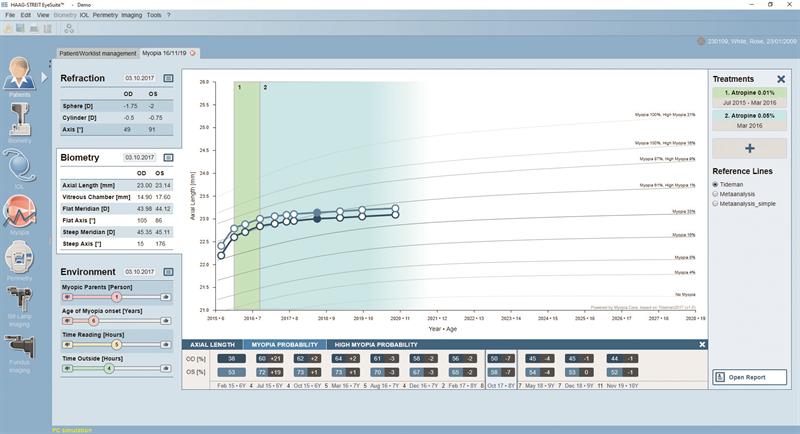 Figure 4: Example of an axial length progression chart produced by the Lenstar Myopia (from Haag Streit UK)
Figure 4: Example of an axial length progression chart produced by the Lenstar Myopia (from Haag Streit UK)
BH: Can you tell me about the PreMO Risk Indicator; how might this be used in everyday primary care practice?
SM: The PreMO risk indicator incorporates the key clinical metrics; family history of myopia, a child’s refractive status and axial length. This means that eye care practitioners can use the PreMO to determine, firstly, a child’s likely risk of myopia onset and, secondly, at what age they are likely to become myopic.
Once myopia has onset, the risk indicator uses the age of the child and their previous change in refractive error to determine if they are likely to be a fast or slow progressor. It is designed to support practitioners in how soon they should review the patient to monitor progression; when it would be useful to give advice about lifestyle and environmental modifications (for example, time spent outdoors or how best to balance near work/screen time with other activities) and when myopia management strategies should be commenced or discussed with the child and parent. It uses a traffic light system to show the child and their parent where they sit in relation to myopia risk (figure 5). We think this makes it a helpful visual aid on which to base these conversations.
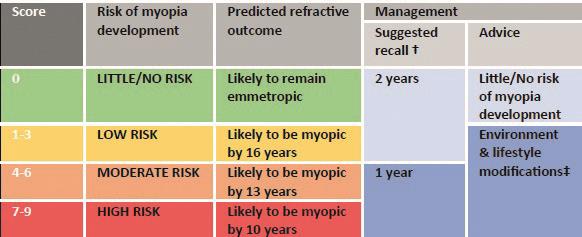 Figure 5: A traffic light system offers a useful visual aid to conversations about myopia
Figure 5: A traffic light system offers a useful visual aid to conversations about myopia
BH: Even though more of us have access to instruments able to measure axial length, is this essential for myopia management? Is the ‘Manchester estimation’ method2 valid?
SM: Within the PreMO risk indicator, we’ve included supplementary tables to determine the risk scores for axial lengths calculated using keratometry and refractive error results. This is because we recognise that, at present, a good majority of practitioners don’t have access to ocular biometry.
We used calculations based on the optics of the eye developed by Professor Phil Morgan at Manchester University to determine these estimates of axial length and the associated risk score.2 These are useful in determining whether a child has longer than average, average or shorter than average eyes, and can be used to determine relative risk of future myopia. The calculations don’t consider the crystalline lens, which still plays a part in determining the overall refractive error of the eye in childhood. Therefore, the estimations are not accurate enough if you want to monitor eye growth.
If you are instigating myopia management strategies that are aimed at slowing the growth of the eye, to reassure ourselves as practitioners and also to demonstrate to the patient and parent that these treatment options are having the expected effect, then we really need to consider purchasing an ocular biometer. There are now a few commercially available biometers designed with myopia management in mind. I think, in the future, all practices are likely to have one just like the shift in practice equipment with fundus cameras and OCTs that has taken place over recent years.
BH: Have there been or are there any plans for further interpretation of the NICER data, perhaps for reasons other than myopia management?
SM: There have been lots of publications of the results of the NICER study not solely relating to myopia management. These include studies of:
- Levels of visual impairment among Northern Irish children3
- Prevalence and progression of astigmatism4
- Prevalence of hyperopia and anisometropia5
One other key finding relating to hyperopes (and yes, we care about them too) which can be helpful for practitioners to know is that, if the child has ≥ +3.50DS of hyperopia, this is likely to persist. Often, we get asked by parents if their child will outgrow their glasses, and this information can be useful to inform this conversation.
BH: Finally, if you could choose the most important things for practising optometrists that can be learned from your research, what would they be?
SM: In the past, we waited until a myope presented with reduced acuity and then we corrected their refractive error. Using the NICER study results, we can now be more accurate at determining those most at risk of myopia and be proactive in our advice to the child and their parents.
I think this reflects the ‘mitigation’ part of the World Council of Optometry call to action6 in terms of the new standard of care for myopia. By doing this, we can be proactive in trying to delay myopia onset for as long as possible by giving advice on environmental modifications. If we can delay myopia onset, even by just a few years, we can have a significant impact on the resultant level of myopia. Early conversations with parents about myopia risk and the available interventions, if required, can ensure that children attend for regular eye examinations and interventions can be instigated early to have the best effect.
References
- A. Sorsby, G.A. Leary, M. Joan Richards. Correlation ametropia and component ametropia. Vision Research, Volume 2, Issues 9–10, 1962, pp 309-313
- Morgan P et al. Estimation of ocular axial length from conventional optometric measures. Contact Lens & Anterior Eye, 2019, 43 (1), pp18-20
- O’Donoghue L et al. Refractive error and visual impairment in school children in Northern Ireland. British Journal of Ophthalmology, 2010, 94 (9), pp 1155
- O’Donoghue L et al. The changing profile of astigmatism in childhood: The NICER Study. Investigative Ophthalmology & Visual Science, 2015. Vol. 56(5): pp 2917-25
- O’Donoghue L et al. Profile of anisometropia and aniso-astigmatism in children: prevalence and association with age, ocular biometric measures, and refractive status. Investigative Ophthalmology & Visual Science, 2013, Vol.54, pp 602-608
- https://worldcouncilofoptometry.info/resolution-th...


