Whether it be a smartphone, smart watch or a wrist band fitness monitor, many readers will already be using devices which are capable of acquiring a whole host of data about the wearer’s activity both day and night. The ease of acquisition is matched by the ease with which this data is interpreted, displayed, or used to offer useful tips on lifestyle improvement or adaptation.
It was only a matter of time before someone thought about using spectacles to carry data tracking technology and be able to usefully incorporate this into a clinical management plan.
Refractive correction
Coincident with the evolution of technology that digitisation has allowed, there has been an explosion in the options available for refractive correction. Spectacle lenses can now be made to reflect the refractive profile of individual patients and surfaced in a way that helps minimise aberration while, in the case of high-end progressive lenses, mimic the way a wearer uses their head and eyes in viewing their surroundings. Presbyopic contact lenses are a major breakthrough but the final best correction, whether that be a full multifocal, adapted or enhanced monovision or even full monovision or distance lenses with reading spectacles is usually only established with complete confidence once the patient has experienced their correction in operation in everyday life for a period of time.
This same problem is a challenge to refractive and cataract surgeons. Accurate measurement of the structure and focus of the eye is possible through a range of techniques, such as cycloplegic refraction, biometry, optical coherence tomography and topography, but such data is only representative of eye use for any particular direction and distance and will not reflect the duration of different optical demands upon the patient. Nor will the influences of factors such as pupil size, amplitude of accommodation or depth of focus, and habitual ocular and head movements be easily known for individual visual task requirements.
Rarely these days is the final given refractive correction the full distance refraction in each eye. More typically, some degree of monovision or a multifocal or accommodative solution is offered that best meets the patient’s future needs. But how can these needs be accurately predicted when the usual way to understand a patient’s visual behaviour is through a question and answer session. And, sadly, it is still all too often that optometrists are left to pick up the pieces when a anisometropic monocular or intolerable binocular correction has been established through surgery and re-treatment is not an option available or wanted.
Vivior visual behaviour monitor
Perhaps for the reasons already touched upon, it is in the field of refractive surgery that the first spectacle mounted visual behaviour monitoring system has been tried. The technology company Vivior has assembled a design team supported by a Medical Advisory Board consisting of renowned surgeons from the US and Europe. Together they have developed a Visual Behaviour Monitor (VBM) which is small enough to add to the side of any standard spectacle frame (figure 1).
The device itself contains much of that already widely available in most smart devices. Infrared sensors are able to locate distances from and proximity to near objects, while the combination of an accelerometer, magnetometer and gyroscope is able to accurately record position and change of position of the unit. Added to that, a photosensor is able to detect changes in ambient lighting. Through these means, the VBM is able to continually collect data of the wearer of the device, including:
- Viewing distances of tasks
- Duration of viewing tasks
- Head motion
- Physical movement including head positioning
- Ambient lighting levels
By wearing the VBM, data can be assimilated that helps build a picture of the viewing habits of any individual and help to influence the subsequent decision about best correction of their refractive error. Figure 2 shows a representation of the different viewing positions (in pink) of a wearer during a day in their office.
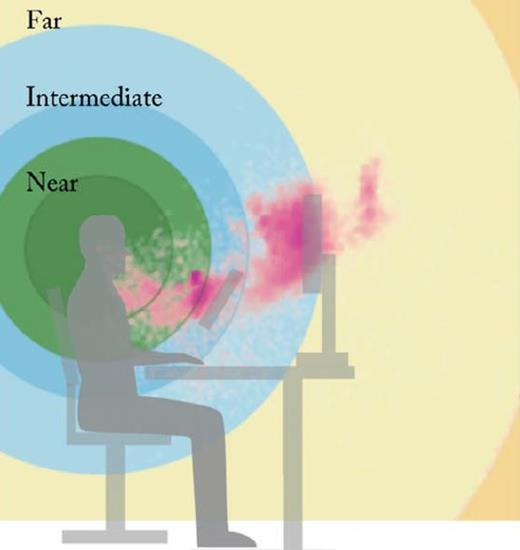
Figure 2: VBM measured viewing positions (in pink) during a day at the office
The profile of each wearer differs significantly, as can be seen in figure 3 which shows the distances viewed by a number of patients and reflects the different near, intermediate and distance requirements for each.
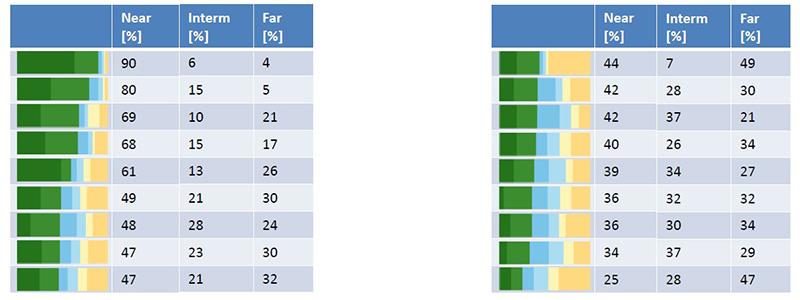
Figure 3: Percentage of time spent viewing near, intermediate and distance targets for 18 different patients as measured by a VBM over one day
This data can be analysed in a variety of ways. Figure 4, for example, shows the refractive error for a pseudophake for a range of viewing distances displayed in terms of the percentage of the day they occur. Note how focusing on infinity (as implied by a full distance correction) only represents a tiny fraction of a typical daily visual demand in either patient data sets.
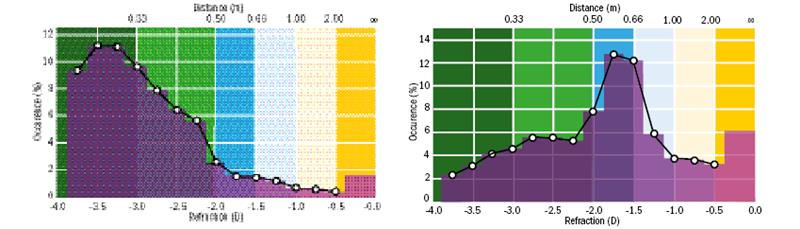
Figure 4: Viewing distance in terms of percentage of time adopted and refractive error for a non-accommodating patient with primarily near demands (a) or intermediate demands (b)
This data has been used successfully in deciding the final IOL power, design and degree of residual error left to best match the visual demand of the patient. Initial successes have been reported at recent refractive surgery conferences. Moreover, involvement of the patient in the process appears to be paying dividends in managing patient expectations and subsequent satisfaction with any compromise in binocular acuity. Patient education and involvement is a key benefit according to early reports.
The future
When discussing a presbyopic correction, whether that be through spectacles, contact lenses or via a wide range of surgical interventions, at the moment we are limited by the detail of our questions when deciding on how a patient uses their eyes throughout any typical day. How many of us, for example, have recommended a ‘hard’ design progressive power lens to a map-reading driver who failed to mention their significant use of a desk top computer every evening and who, therefore, soon returned unimpressed by the lens prescribed?
Though currently mainly aimed at refractive surgery outcome decision, the VBM is a device I suspect we will be hearing much more about in the coming years. Being able to map the visual behaviour and to incorporate the patient in the process has some obvious attraction for those of us prescribing and dispensing high value modern corrections, whether contact or spectacle. Also, how long before such a device might include further capability, such as eye tracking technology, blink monitoring or adaptive optical lens input. The potential for a research tool and patient interface is truly impressive.
For further information go to www.vivior.com

