The first article (Optician 01.06.18) outlined the background and importance of using lissamine green as part of a useful diagnostic adjunct in a routine dry eye work up. This second article through the use of case studies and images (from Sarah Farrant’s private dry eye clinic) will help demystify how to get the best clinical results with lissamine green and answer questions such as what are normal/incidental findings and what indicates ocular surface pathology?
Clinical Top Tips
Figure 1 Preparation using a lissamine green strip and saline

Preparation – Wet the strip with saline (figure 1) and rock the drop back and forward up and down the strip to increase the concentration of the lissamine green in the drop. You could also use two strips together to increase the concentration. We advocate using lissamine green and fluorescein separately which makes it easier to evaluate the tissue(s) and interpret any ocular surface staining.
Application – TFOS DEWS II recommends instillation on the temporal conjunctiva just above the lid margin (figure 2).1 You need a larger volume than fluorescein but be gentle, to avoid causing surface damage to the palpebral or tarsal conjunctiva.
Figure 2: Application technique

Artefacts – Do not confuse evidence/staining caused by poor application technique with the true ocular surface integrity interpretation (figure 3).
Figure 3: Surface damage on the lower tarsal conjunctiva from poor instillation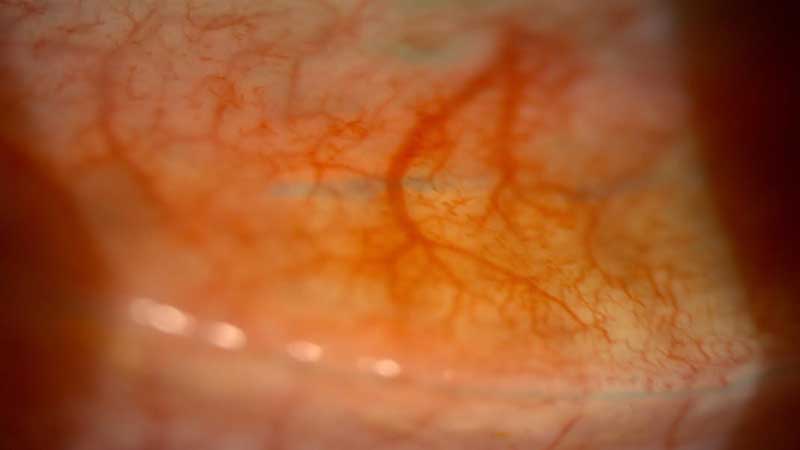
Normal findings – Understand normal features that are stained. These are:
- Line of Marx (figure 13) – The distinct line of cells running along the majority of the inner eyelid marginal zone, reflecting the natural mucocutaneous junction between the eyelid margin and bulbar conjunctiva/cornea surfaces.
- Conjunctival folds (figure 5) – This pooling is normal and indicates areas of ‘baggy’ conjunctiva.
- Mucous strands (figures 6 and 7) – There is debate over whether the dye stains mucin, if it does it will move on blink.
Figure 4: Lid wiper epitheliopathy grade 1, band staining 25% of the width of the lid wiper (Korb grade 1)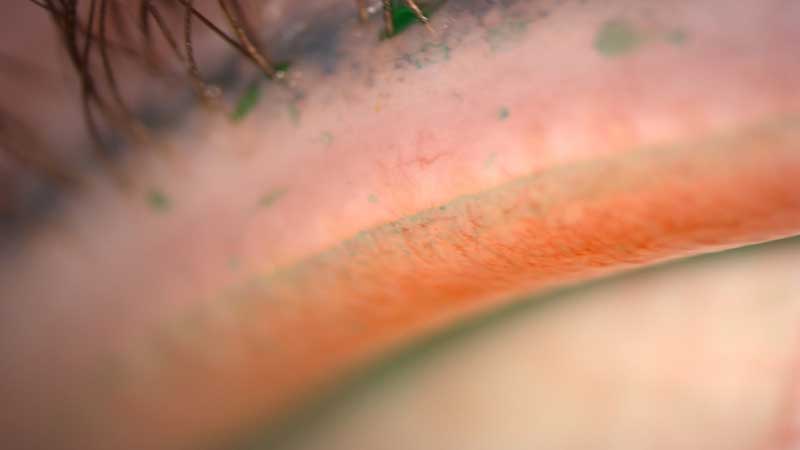
Incidental findings – General ocular conditions (especially those affecting the conjunctiva and lid margins), poor fitting contact lenses or post refractive surgery may result in staining or pooling (figure 8).
Ocular surface integrity evaluation
- Bulbar conjunctiva (figure 2) – The best approach is to evaluate the number of dots, using a grading scale to an accuracy of 0.1 increments. Supplement the findings with sketches and images.
- Cornea – Our view is to best use fluorescein but still worth a quick glance during a slit lamp sweep.
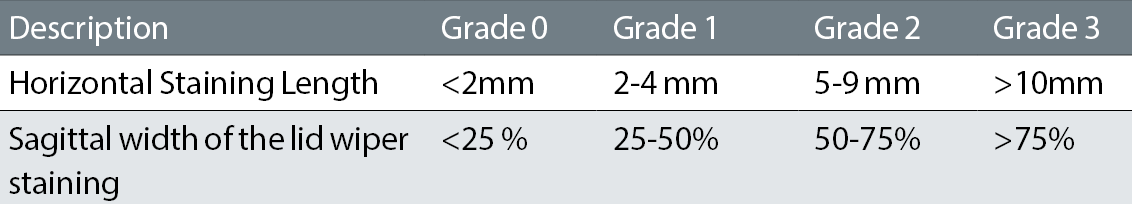
- Lid wiper region (figure 4) – The author’s tip is to always add a second drop in line with the process outlined below. Both lids can be assessed although the lower lid assessment can be more challenging. Marx line should be present if the right volume of stain has been used, assess any staining away from this anchor (we use Korb’s grading scale as outlined in table 1). Note, sketch and image any irregular appearances.
Figure 5: Lissamine green pooling in conjunctival folds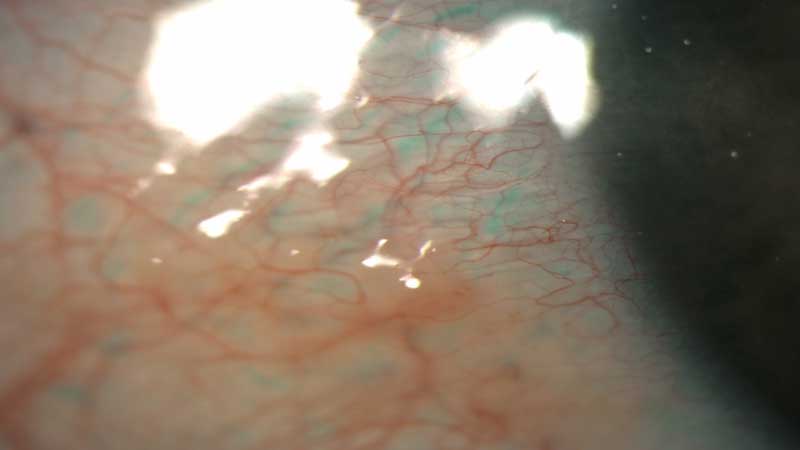
Figure 6: Staining of an excess mucous strand in the tear film
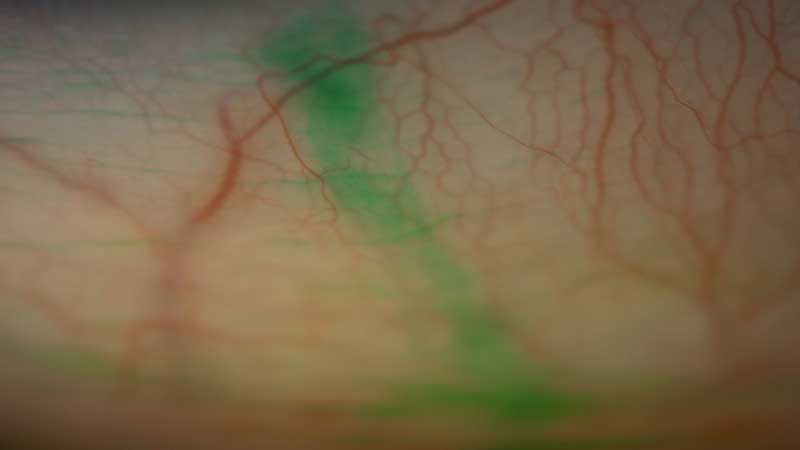
Figure 7: Same eye as figure 6 showing movement of stain on blinking indicative of mucous strand staining

Figure 8: Subtle staining over a damaged elevated area of conjunctiva due to the presence of pinguecula

Table 1: Korb grading scale
Best practice technique (using strips)
- Wash your hands and check the strip expiry date.
- Use saline to wet the strip without contaminating the saline bottle. Ensure a whole drop (or two) stays on the strip for >5 seconds.
- Apply a large drop of the stain at the outer canthus to avoid ocular surface damage. A larger volume is needed compared with fluorescein.
- Evaluate one to four minutes post instillation using white light, low illumination (some also advocate using a red filter).
- Assess cornea and conjunctiva- use grading scales and sketch/image the findings.
- Add a second drop after five minutes and evert the upper lid to assess the lid margins three to six minutes later, also inspect the lower lid margins.
- Irrigate the stain from the eyes, the dye is not contact lens compatible.
- For any discoloured surrounding skin, use a wipe with some oil or ointment as the dye is not water soluble.
If combined assessment of both stains is required then both strips can be wet and applied at the same time, if done separately apply fluorescein first. More lissamine green is needed than fluorescein, so consider using two strips of lissamine green together with one fluorescein strip.
Case Studies
We will now look at some case examples to illustrate how lissamine green may aid diagnosis, clinical decision making and patient management.
Case 1: Mrs PJ, age 72
Presented as a new patient to the dry eye clinic having attended the practice for a routine eye examination. The optometrist detected obvious signs of dry eye disease and discussed the need for a more thorough dry eye diagnosis and management within the specialist clinic.
Figure 9: DEQ scoring for patient PJ
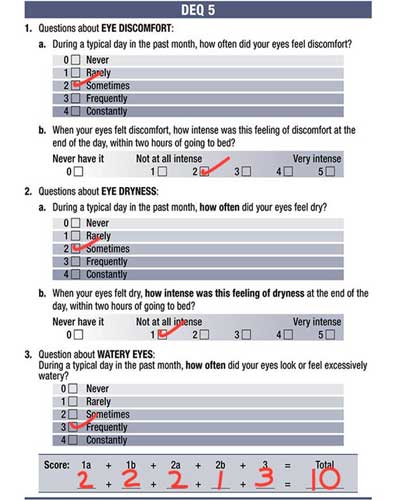
Figure 10: Exposed Demodex mite visible on central lash confirmed diagnosis of Demodex blepharitis
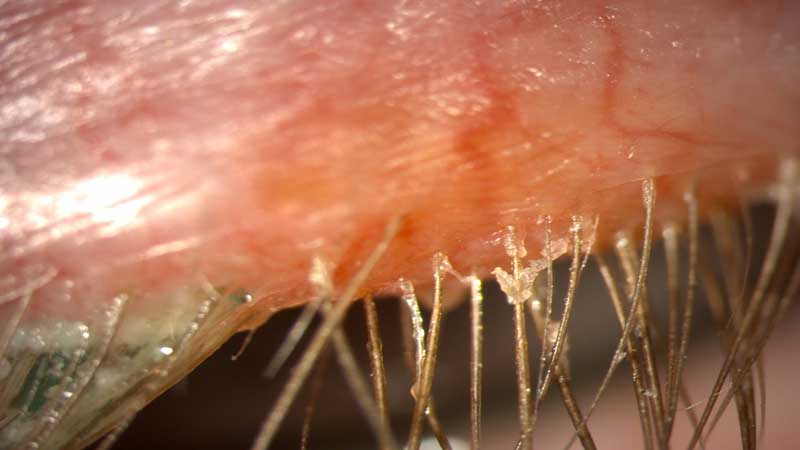
Figure 11: Irregular band of Lid wiper epitheliopathy along the lower lid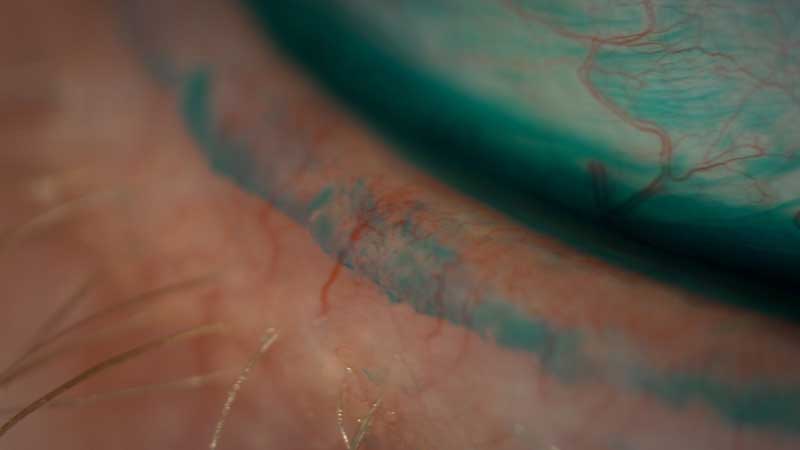
There was a history of longstanding irritation, grittiness, soreness and redness which was similar in both eyes (at least three years). Occasional visual disturbance was reported, which cleared on blinking. No discharge was found. The patient had tried hypromellose eye drops and warm flannels as recommended by their GP but found no relief from the symptoms. No mouth dryness or swollen glands.
General Health: diabetes
Medication: metformin, statin, atenolol
Ocular History: none, though aware of early bilateral cataract. No contact lens wear
Lifestyle: reading and gardening, tablet use for one hour a day
Visual Acuity (varifocals six months old)
R 6/7.5
L 6/9
DEQ-5 score (figure 9): 10 (DEWS II diagnostic criteria for dry eye are scores ≥6 for symptomology+ at least one sign from the list of clinical tests)
Osmolarity score: R 327 L 316 (DEWS II criteria ≥308 mOsm/L in either eye, or inter-eye difference of more than 8mOsm/L)
Further examination showed evidence of demodex infestation (figure 10), meibomian gland drop out (figure 12) and blockage (figure 14), and changes to Marx’s line (figures 11 and 13).
Figure 12: Meibomian gland atrophy nasally on lower lid seen with visible light (left) and infra-red (meibography on the right)
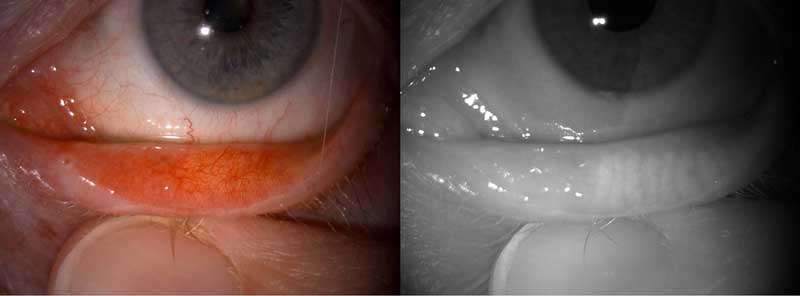
Figure 13: Upper lid showing Marx’s line (demarcates keratinised skin with mucous membrane) with meibomian gland orifices visible as partially engulfed and bisected by the lissamine green band

Normally the meibomian gland orifices should sit anterior to Marx’s line in front of the tear prism in normal cases. This position facilitates normal meibum secretion onto the outermost surface of the tear film where it forms the outermost lipid layers. It is not unusual that marks line moves forward with age and cicatricial changes can pull the MG orifices posteriorly resulting in them being engulfed by Marx’s line and sitting within the tear prism. The result is a less efficient lipid layer, given that any gland secretion occurs directly into the aqueous portion of the tears. It is always useful to therefore note where the MG orifices are relative to Marx’s line.2
The patient was diagnosed with moderate meibomian gland dysfunction and demodex blepharitis and, after thorough discussion including showing her the images gathered on the slit lamp, she was given an initial management plan as follows with a planned six month follow up:
- In office: full gland expression 6/12ly, Blephex and Tea tree oil 6/12ly
- At Home: warm compress using an eye warming device with ocular massage, daily lid hygiene and omega 3 supplements.
Case 2: Mrs CB, age 57
Mrs B is a longstanding patient with mild meibomian gland dysfunction. She has been under the dry eye clinic for roughly three years and historically has been managed well with a basic regime of an in-office six monthly gland expression using meibomian gland forceps and lid margin debridement with golf club spud, coupled with daily warm compress and massage. She had been controlling the condition well with minimal symptoms day to day.
Figure 14: Grade 2 (left and central gland) and 3 (right gland) meibum secretion on gland expression inferiorly. All four lids were expressed both to aid diagnosis and as a treatment strategy to help improve gland function and clear stagnant meibum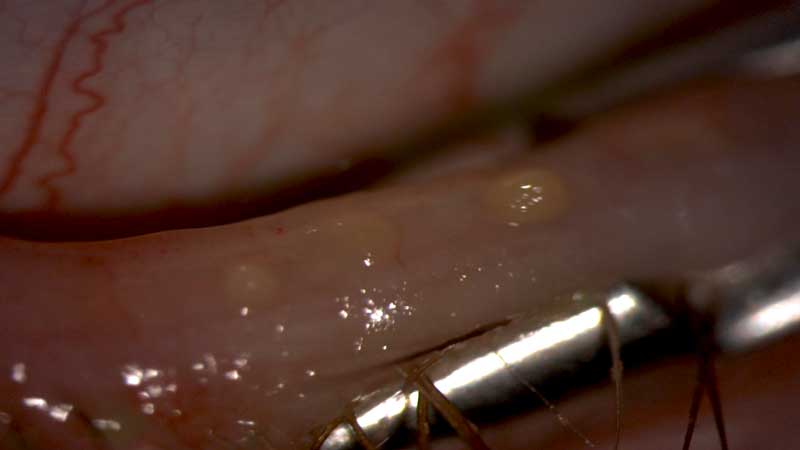 Figure 15: Fluorescein stain in the left eye showing large (right) and small (left) filaments
Figure 15: Fluorescein stain in the left eye showing large (right) and small (left) filaments
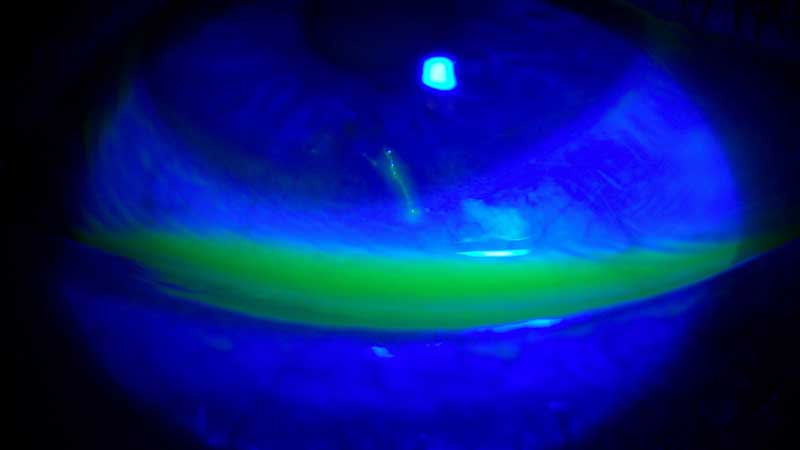
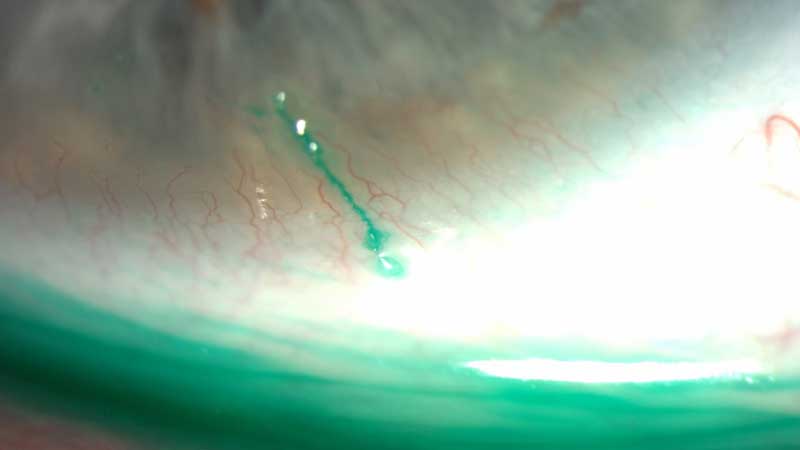
Figure 16: Lissamine green stain of filament showing movement on blinking and highlighting corneal attachment location Figure 17: Instillation of lissamine green highlighted the filament strand to aid diagnosis and facilitate removal under white light conditions
Figure 17: Instillation of lissamine green highlighted the filament strand to aid diagnosis and facilitate removal under white light conditions
General Health: controlled blood pressure and cholesterol
Medications: ramipril, atorvastatin
Ocular History: low myope, last eye exam nine months ago.
Lifestyle: office work, use of digital screens six hours daily, reading
Visual Acuity
R 6/6
L 6/6
Current DEQ-5 score: 17 (was total of three at last routine dry eye review three months ago)
Previous osmolarity score at last dry eye review three months ago: R 302 L 296 mOsm/
Figure 18: Removing the filament with jeweller’s forceps She presented to the clinic outside of her normal six monthly checks with complaints of greatly increased discomfort which had started roughly two weeks ago. No trauma history and no other change to her regime, health or lifestyle could be identified. The discomfort seemed to be in her left eye only, with worsening symptoms on blinking, but generally constant throughout the day. The pain level was not sufficient to wake her up during the night.
She presented to the clinic outside of her normal six monthly checks with complaints of greatly increased discomfort which had started roughly two weeks ago. No trauma history and no other change to her regime, health or lifestyle could be identified. The discomfort seemed to be in her left eye only, with worsening symptoms on blinking, but generally constant throughout the day. The pain level was not sufficient to wake her up during the night.
The diagnosis of filamentary keratitis was made after slit lamp review and fluorescein (figure 15) and lissamine green instillation. Filamentary keratitis is a condition in which strands composed of degenerated epithelial cells and mucus form and stick to the corneal surface and result in foreign body sensation. There is often an increase in the tear film mucus to aqueous ratio. It is usually associated with decreased tear production but can also be a result of increased production or accumulation of the mucin component. Small defects in the cornea allow mucin to attach and act as an anchoring surface for the filaments and loose epithelium (figures 16 and 17).
Figure 19: Post filaments removal with small corneal epithelial defect visible with fluorescein (left) on the cornea, but not visible with lissamine green and white light (right).
The strands (one large, one small) were removed with jeweller’s forceps after local anaesthetic instilled (figures 18 and 19). The additional condition was described to the patient and the patient was prescribed ilube bd for 1/12. This mucolytic helps to break down the mucus to stop strands forming. No additional follow up was planned with a SOS to return if required. She was instructed to attend her planned routine dry eye appointment in three months’ time.
Final Thought
Lissamine green also has a useful role in contact lens patients. Lid wiper epitheliopathy is thought by some authorities to potentially be the only clinically visible sign of contact lens discomfort. In addition, a tight fitting soft contact lens can induce indentation on the conjunctiva that can be highlighted with lissamine green staining. Having a healthy ocular surface is key to contact lens comfort and successful retention.
This article shows a few ways in which lissamine green is a useful aid to diagnosis in a primary care dry eye clinic setting. It should be considered as a useful part of our diagnostic armoury. It can also be used for other interesting purposes such as highlighting the mires in Goldmann tonometry.
Neil Retallic is an optometrist and professional services manager with CooperVision. Sarah Farrant is a therapeutic optometrist with a specialist interest in dry eye disease practising in Somerset, UK. Both authors are panel members of the Lissamine Green Consensus Panel, this report once finalised will be published and sent to the MHRA with a view to a statement from the GOC.
References
- TFOS DEWS2 http://dx.doi.org/10.1016/j.jtos.2017.05.001
- Yamaguchi M, Kutsuna M, Uno T, et al. Marx line: fluorescein staining line on the inner lid as indicator of meibomian gland function. Am J Ophthalmol. 2006; 141:669-675
