
So far in the recent CPD series on age-related macular degeneration, the focus has been on assessment and management. In part 1, there was a detailed discussion of the latest theories of the causes of the condition and its many and various risk factors. By knowing these, it is possible to undertake a more focused and detailed history and symptoms to investigate any patient either known to have or suspected to have AMD. Part 2 of the series took a closer look at the investigation of the disease using a variety of techniques, both established and using newer technologies.
In our recent VRICS exercise, you were presented with 12 cases to interpret.
Retinal Photography
Case 1
This patient was a 67-year-old male attending for a routine eye examination. He was a pseudophake, having had his cataracts removed some five years previously. His last eye examination was just after his surgery and, since then, he had noticed a slow decline in his ability to read smaller print. He is now finding this becoming inconvenient and so has attended today hoping for stronger spectacles.
His current spectacles are as follows:
- R: +0.50/ -0.50 x 180 (6/9)
- L: +0.25 / -0.75 x 175 (6/9)
- Add: +3.00 (N6- R&L) @ 35cm
There is no improvement with pinhole.
Q1. Which of the following cannot be seen in the retinal image?
A: Exudates.
The foveal area clearly shows pale, hypopigmented patches with associated darker, hyperpigmented patches. Taken in context with the reduced acuity, this would appear to be highly characteristic of dry AMD. As you move further from the fovea, the patches become more discrete and without pigment, with smaller patches combining with larger ones where they have coalesced; a typical appearance of soft drusen. More peripheral still, notably in the superior area beyond the arcades, discrete drusen are highly distinguishable. As photography does not indicate lesion depth, which would easily distinguish an intraretinal lesion such as an exudate from a subretinal lesion such as drusen, it is useful to consider the vasculature. As there is no obvious association between the white patches and the vessels, and as the vessels appear healthy, then exudates are unlikely.
Case 2
This patient had last had an eye examination some nine months ago. He is a 70-year-old smoker and had been told at the last eye examination of some ‘age changes at the back of his eyes’. He had been given advice about smoking cessation, diet, and had been issued with an Amsler chart, which, he confessed, he had not used. He did, however, feel that there had been some change to his vision in the left eye ‘a week or so’ ago, but had not acted on this. Today, however, he woke to notice a dramatic drop in the vision in this same eye which you measured to be 6/60.
Q2. Which of the following is the most likely explanation of the visual disturbance ‘a week ago’?
A: Serous elevation of the fovea leading to hypoxia.
Q3. Which of the following is the most likely explanation of the visual disturbance this morning?
A: Subfoveal haemorrhage.
This case is a good illustration of the appropriate management of suspected wet AMD. The initial and sudden onset central visual disturbance is a useful indication of serous fluid pushing up the foveal neuroretina. Previously, this might have been confirmed by distortion or metamorphopsia on an Amsler, but the advent of OCT has made it far easier to detect such fluid elevation (see also OCT section). As the foveal photoreceptors rely on oxygen supply from the choroidal vasculature, this elevation of the retina leads to hypoxia in the region, a build-up of vascular endothelial growth factor (VEGF) and a subsequent risk of neovascularisation. Prompt referral of the elevation might allow anti-VEGF treatment to prevent future neovascularisation.
Prompt referral would mean immediate contact with the vitreoretinal clinic by your usual correspondence route to arrange a clinic appointment as soon as possible, and definitely in fewer than 14 days. It is also good practice to tell the patient that, if they have not heard from the clinic about an appointment within 48 hours, then they should contact you to chase up.
Perhaps counterintuitively, once a subfoveal haemorrhage has occurred, blood makes accurate assessment of the nature of vessel proliferation less accurate and, of course, suggests that the opportunity for most effective anti-VEGF intervention may have passed. With blood present, and especially where acuity has dropped below 6/96, the hospital may well suggest a less urgent referral, allowing opportunity for blood reabsorption and a better assessment of the foveal area.

Case 3
This 71-year-old female attended for her annual eye examination. She had been told a year ago about early AMD changes and given appropriate advice. Her best corrected acuity was 6/9 in each eye The fundus appearance (figure 3a) appeared very similar to last year. Since last year, your practice has acquired an OCT and a volume scan of the posterior pole was undertaken, one line scan of which is shown in figure 3b.
Q4. What does the retinal image show?
A: Soft drusen, reticular drusen and crystalline drusen.
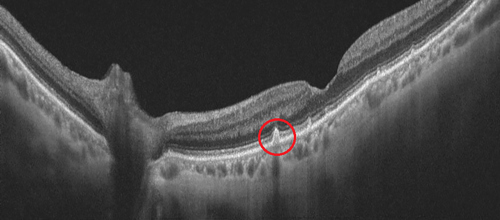
Q5. What are the hyperfluorescent lesions outlined by the red circle on the OCT scan?
A: Reticular drusen.
The retinal photograph shows the larger, coalescent lighter lesions characteristic of soft drusen. The crystalline, shiny appearance of the larger ones suggests the presence of calcification, a change that is common in longstanding drusen. Remember, the etymology of the word ‘drusen’ is from the German ‘druse’ meaning crystallised ore.
The OCT scan shows the typical subretinal bumps of these drusen, most noticeably on the left side of the image. However, the area circled shows hyperfluorescent patches within the retina. This is not fluid, which would be hypofluorescent, but instead indicate the presence of reticular drusen. Look out for a detailed discussion of these often-ignore lesions in a future CPD article in Optician.

Case 4
This 78-year-old male attends for a low vision assessment has attended for a low vision assessment, having been certified as eligible for sight impairment registration. His best corrected acuity is 0.9 logMAR right and left, and he can achieve N24 @ 25cm with a +4.00DS add.
Q6. Which of the following is not seen in the retinal image?
A: Macular oedema.
This is a sight-impaired registered patient from my low vision clinic. On a retinal photo, the presence of crystalline drusen, along with the longstanding stable, albeit poor, acuity supports the diagnosis of late stage dry AMD. The generalised pallor and absence of drusen centrally is indicative of a geographic atrophy, which makes it possible, on occasion, to see choroidal vascular incidents such as the small haemorrhagic change shown.
Q7. What magnification would be predicted for him to achieve N8 with a 2:1 acuity reserve?
A: 6x.
Some good old low vision revision here. To achieve N8 with a 2:1 acuity reserve, the target acuity would be half of N8, so N4. N4 is 6x smaller than N24, the acuity achieved with unit magnification (as given by a +4.00DS add).

Optical Coherence Tomography (OCT)
Case 5
A 75-year-old woman attends for a routine eye test, having previously been told she had dry AMD. Her OCT scan is shown here.
Q8. Which of the following terms best describes the feature outlined in red on the OCT scan?
A: Drusenoid RPE detachment
Though a large, likely soft, drusen lying on Bruch’s membrane is the reason for the appearance, the small peak is caused by the drusen pushing up the overlying RPE, and thus described as a drusenoid RPE elevation, is the best description.
Case 6
This 82-year-old is registered as severely sight impaired, each eye having a best acuity of 1.3 logMAR.
Q9. What can be identified from the OCT scan?
A: Geographic atrophy
The en face image on the left reveals a large diameter, well defined circle of thinned, atrophic retina allowing a clear view of the underlying choroidal vasculature. The cross-section on the right reveals how in this area there is loss, or atrophy, of deeper retinal tissues. A classic geographic (essentially, meaning over a large area) atrophy as is expected in late-stage dry AMD.

Case 7
A 61-year-old female smoker attends for a routine eye examination. Her corrected acuities are 6/5 R&L (N4.5 with a +2.25DS add). You undertake a scan of her posterior pole and decide to discuss your findings with her. She asks about two things (marked 1 and 2) on the scan image.
Q10. What is shown at position 1?
A: Hard drusen.
The small discrete white dots seen on the left, en face view are seen in cross-section (right view) to be overlying the Bruch’s membrane and under the RPE; so are hard drusen.
Q11. What is shown at position 2?
A: Shadow from retinal vessel.
The central green line on the en face view represents where the cross-section on the right is being viewed. As the line passes along a retinal vein around position 2, then the darker area is the shadow caused by the vessel blocking the incident light from the OCT.

Case 8
A 78-year-old male myope, with a best corrected acuity of 0.3 logMAR in the left eye has noticed a gradual reduction in the quality of his vision over the last year. His notes show that, around five years ago, he had been referred for a visual disturbance and a posterior vitreous detachment had been confirmed at that time.
Q12. What is the bright spot on the left en face image?
A: Image artefact.
Q13. What can be seen in the red circle on the line scan on the right?
A: RPE detachment.
I am sure most readers will be familiar with this appearance, one caused by the OCT lens needing a good clean. That said, this image shows how useful information can be gained even with a dirty lens. The en face image shows the black streaks suggestive of an epiretinal membrane while the cross-section shows an obvious RPE detachment.

Case 9
A 68-year-old female, to whom you had issued an Amsler chart eight months ago, attends for an appointment within 24 hours of telephoning your practice to say she had noticed distortion of the grid that morning. This had not been noticed previously.
Q14. What is shown in this scan?
Answer: Serous detachment.
Q15. What might be your management of the patient?
Answer: Fast-track referral.
The large black area seen under the retina shows serous fluid lifting up the overlying retina. As discussed, earlier, a fast-track referral is warranted here. A retinoschisis would be seen as a split (or dark space) within the more central retinal layers and is also very rare at the posterior pole.

Advanced Technologies
While this last section features technology that might not be currently available within many primary care practices, each has a clear benefit in retinal assessment and, in my view, will become standard in the coming years.
Case 10
Q16. What technique has been used to produce these images?
A: OCT-angiography.
OCT-angiography, or OCT-A, uses a Doppler effect from flowing blood to represent areas of blood perfusion in different layers of the deeper retina. In this image, the top left view clearly shows a cluster of choroidal new vessels.

Case 11
Q17. What technique has been used to produce these images?
Answer: Multicolour scanning laser imaging.
By using selected wavelengths of light, such as blue, red and green, to construct a composite multicolour image, greater resolution of structures relevant to the different depths of colour penetration is possible. This is a view of geographic atrophy not dissimilar to that shown in figure 6.

Case 12
Q18. What technique has been used to produce these images?
A: Fundus autofluorescence.
Fundus autofluorescence, or FAF, as shown here, uses shorter (blue or green) wavelength incident light that excites certain molecules such as lipofuscin. As lipofuscin is an indicator of inflammatory processes that take place in degeneration of retina, then it makes it possible to show hypofluorescent, dark areas of atrophy surrounded by fluorescence where degeneration is still under way.

- In April, the CPD series will continue with a discussion of AMD referral pathways, medical management and follow-up.


